Table of Contents
Symptoms of Yeast Infections and UTIs: A Quick Comparison
Yeast infections and UTIs manifest through various symptoms, which can sometimes overlap, leading to confusion.
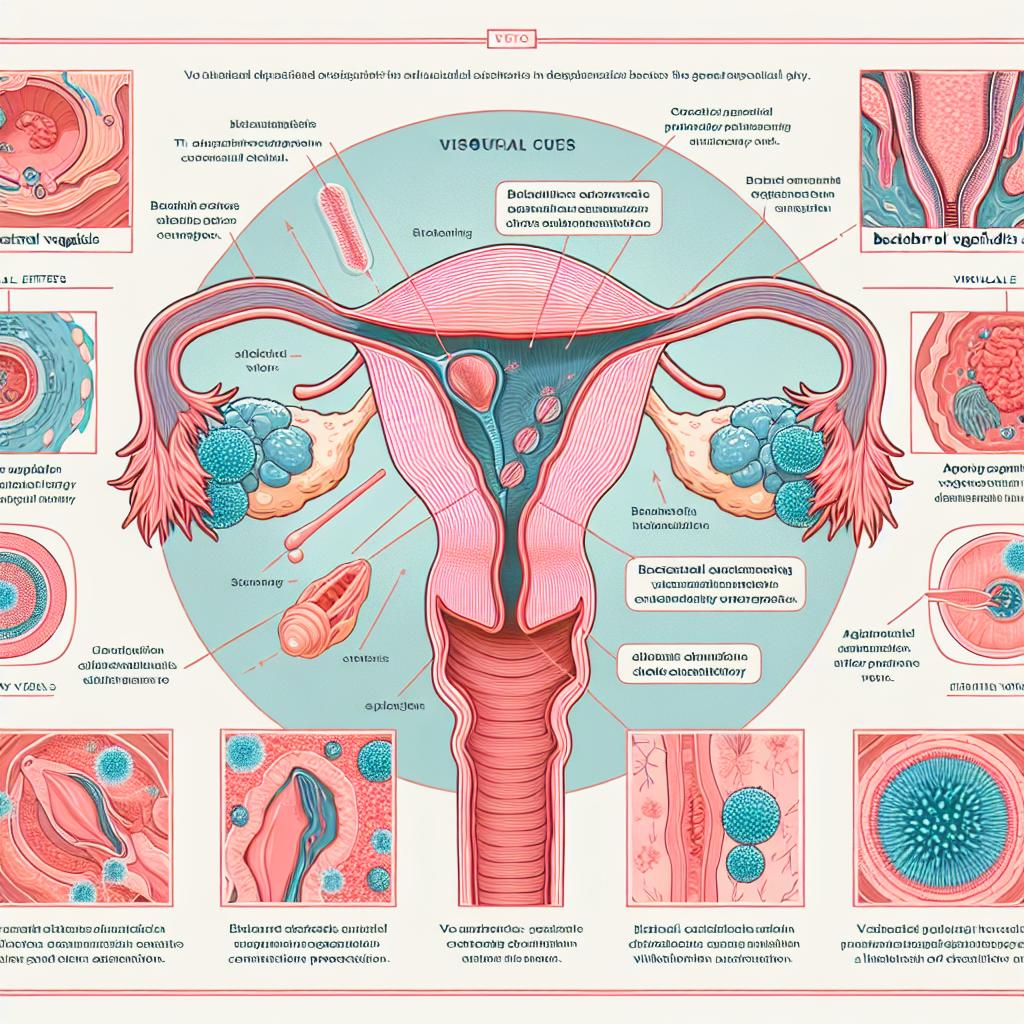
Yeast Infection Symptoms:
- Itching and Irritation: Intense itching around the vagina and vulva.
- Discharge: Thick, white discharge resembling cottage cheese, often odorless.
- Redness and Swelling: Swelling of the vulva and surrounding areas.
- Pain During Intercourse: Discomfort or pain during sexual activity.
- Burning Sensation: A burning sensation during urination, often confused with UTI symptoms.
UTI Symptoms:
- Frequent Urination: An urgent need to urinate frequently, often producing little urine.
- Burning Sensation: A burning feeling during urination.
- Cloudy Urine: Urine may appear cloudy, dark, or have a strong odor.
- Pelvic Pain: Discomfort in the lower abdomen or pelvic area.
- Fever and Chills: In more severe cases, fever may occur, indicating a possible kidney infection.
Table 1: Symptom Comparison
| Symptom | Yeast Infection | UTI |
|---|---|---|
| Itching | Yes | No |
| Thick, white discharge | Yes | No |
| Frequent urination | No | Yes |
| Burning sensation during urination | Yes | Yes |
| Cloudy or foul-smelling urine | No | Yes |
| Fever | Rare | Yes (in severe cases) |
Causes of Yeast Infections and UTIs: What You Need to Know
Causes of Yeast Infections:
Yeast infections are primarily caused by an overgrowth of the fungus Candida, particularly Candida albicans. Factors contributing to this overgrowth include:
- Antibiotics: Disruption of the normal vaginal flora.
- Hormonal Changes: Fluctuations due to menstruation, pregnancy, or hormonal therapy.
- Diabetes: High sugar levels can promote yeast growth.
- Immune System Weakness: Conditions that weaken the immune system can increase susceptibility.
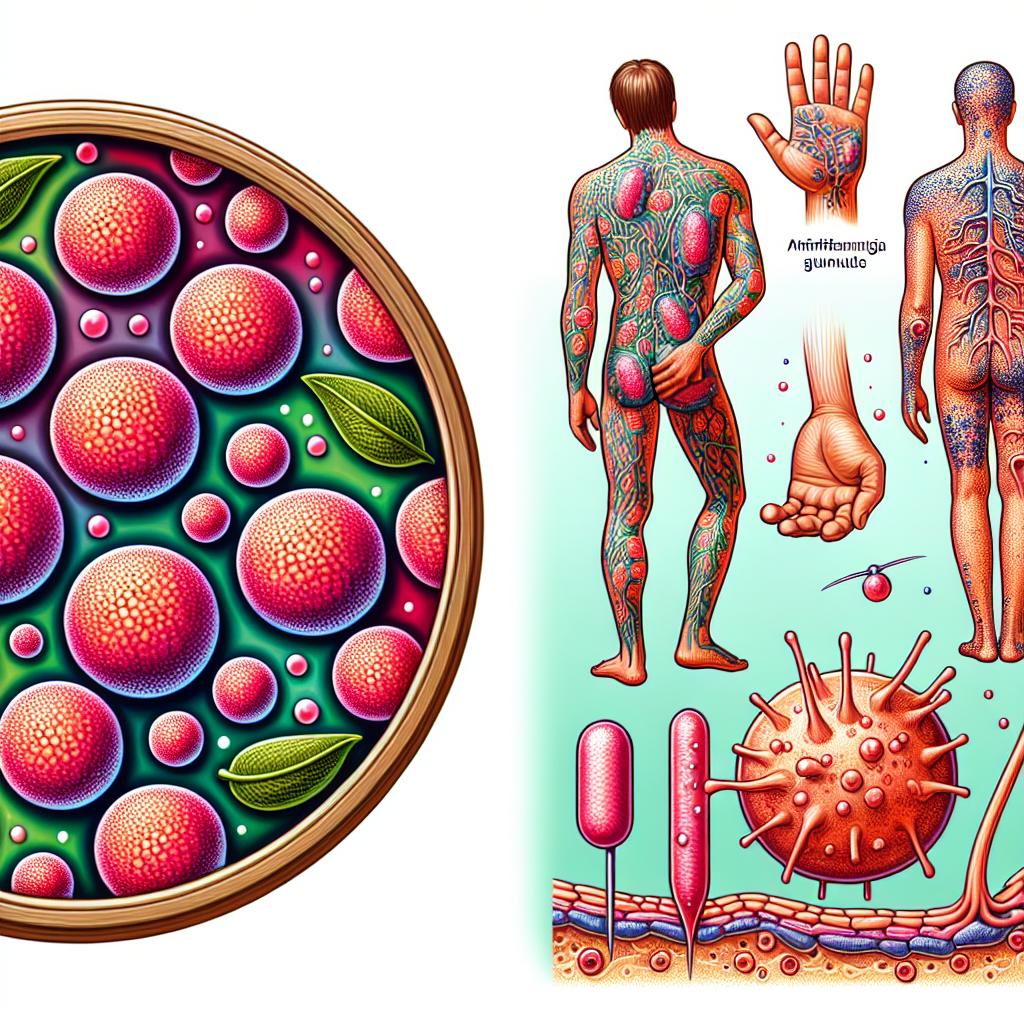
Causes of UTIs:
Urinary tract infections are caused mainly by bacteria entering the urinary tract. Common causes include:
- Bacterial Infection: Most commonly from Escherichia coli, which normally resides in the intestines.
- Sexual Activity: Increased risk due to bacteria introduced during intercourse.
- Poor Hygiene: Inadequate wiping methods can facilitate bacterial entry.
- Urinary Retention: Inability to empty the bladder completely can promote bacterial growth.
Treatment Options for Yeast Infections and UTIs
Treatment for Yeast Infections:
The treatment for yeast infections typically includes antifungal medications, which can be administered orally or topically. Common antifungal treatments include:
- Fluconazole: An oral medication that is highly effective.
- Topical Treatments: Creams or suppositories containing clotrimazole or miconazole.
Treatment for UTIs:
UTIs are generally treated with antibiotics. The choice of antibiotic may depend on the specific bacteria causing the infection. Common antibiotics include:
- Trimethoprim-sulfamethoxazole: Often the first-line treatment.
- Nitrofurantoin: Another common antibiotic used for uncomplicated UTIs.
- Fosfomycin: A single-dose treatment option for certain cases.
Preventive Measures: How to Avoid Yeast Infections and UTIs
Preventing Yeast Infections:
- Maintain Proper Hygiene: Regular washing and drying of the genital area can help.
- Avoid Irritants: Stay away from scented soaps, bubble baths, and douches.
- Wear Breathable Fabrics: Cotton underwear is advisable to reduce moisture retention.
- Limit Antibiotic Use: Only use antibiotics when necessary to avoid disrupting vaginal flora.
Preventing UTIs:
- Stay Hydrated: Drinking plenty of water helps flush out bacteria.
- Urinate Before and After Intercourse: This helps remove bacteria that may have entered the urethra.
- Wipe from Front to Back: This reduces the risk of bacteria from the rectal area reaching the urethra.
- Consider Probiotics: They may help maintain a healthy balance of bacteria in the body.
FAQ Section
Can a yeast infection lead to a UTI?
Yes, the symptoms can overlap, and irritation from a yeast infection can lead to urinary discomfort, potentially mimicking UTI symptoms.
Are yeast infections and UTIs contagious?
No, both conditions are not contagious. Yeast infections arise from imbalances in normal flora, while UTIs are typically due to bacterial infections.
How can I differentiate between a yeast infection and a UTI at home?
If you experience intense itching and thick discharge, it is likely a yeast infection. If you have frequent urination with burning sensations, it may be a UTI. However, it’s best to consult a healthcare provider for a definitive diagnosis.
Are there any home remedies for yeast infections?
Some home remedies include yogurt containing live cultures, garlic, and coconut oil, but these should be used cautiously and are not substitutes for medical treatment.
When should I see a doctor?
If symptoms persist for more than a few days, worsen, or are accompanied by fever or chills, it’s important to see a healthcare provider.
References
-
Bharti, D., Kulanthaivel, S., Mishra, P., Jain, N., Pal, K., & Banerjee, I. (2025). Emulsifier-modified sunflower oil-sunflower wax oleogel as growth modulator of probiotics. BBA Advances, 100147. https://doi.org/10.1016/j.bbadva.2025.100147
-
Yilmaz, S. (2025). Understanding oncologic emergencies and related emergency department visits and hospitalizations: a systematic review. BMC Emergency Medicine, 25(1), 1-15. https://doi.org/10.1186/s12873-025-01183-2
-
Matute, D. R., & Teixeira, M. (2025). Sporothrix is neglected among the neglected. PLOS Pathogens, 11(12), e1012898. https://doi.org/10.1371/journal.ppat.1012898
-
De Decker, M., Pavol, Z., Moens, T. G., Beckers, J., Contardo, M., Dittlau, K., Van Schoor, E., Ronisz, A., Eggermont, K., Moisse, M., Van Den Bosch, L., & Pasterkamp, R. J. (2024). C21ORF2 mutations point towards primary cilia dysfunction in amyotrophic lateral sclerosis. Brain, 147(1), 1-20
-
Guo, L.-C., Hu, S., Zhu, H.-Y., Shang, Y.-J., Qiu, Y.-J., Wen, Z., Chen, S.-X., Bai, F.-Y., & Han, P.-J. (2025). Four new species of Pichia (Pichiales, Pichiaceae) isolated from China. MycoKeys, 114, 115–132. https://doi.org/10.3897/mycokeys.114.142474
-
Maeda, M., Arakawa, M., & Saito, K. (2025). Disease‐Associated Factors at the Endoplasmic Reticulum–Golgi Interface. Traffic, 26(1-3), 1-20