Table of Contents
Definition of Mixed Urogenital Flora
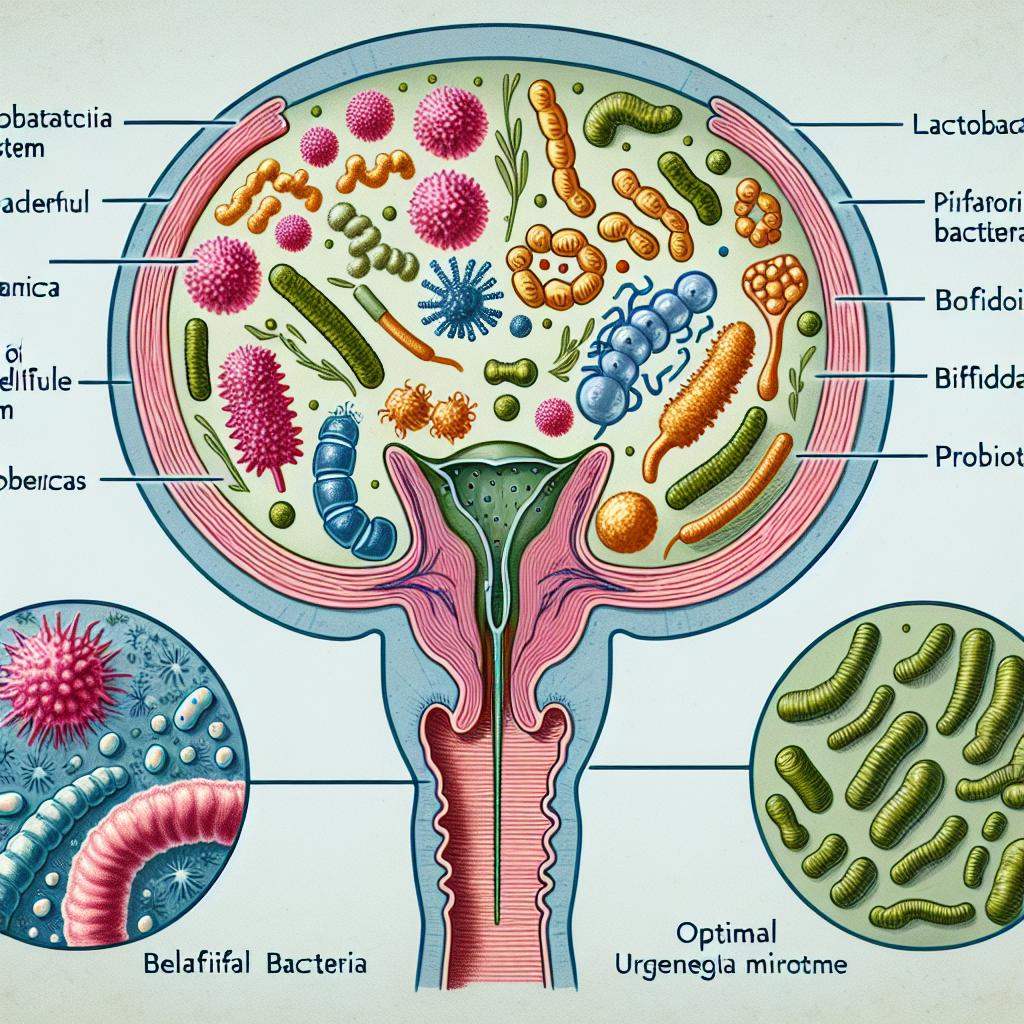
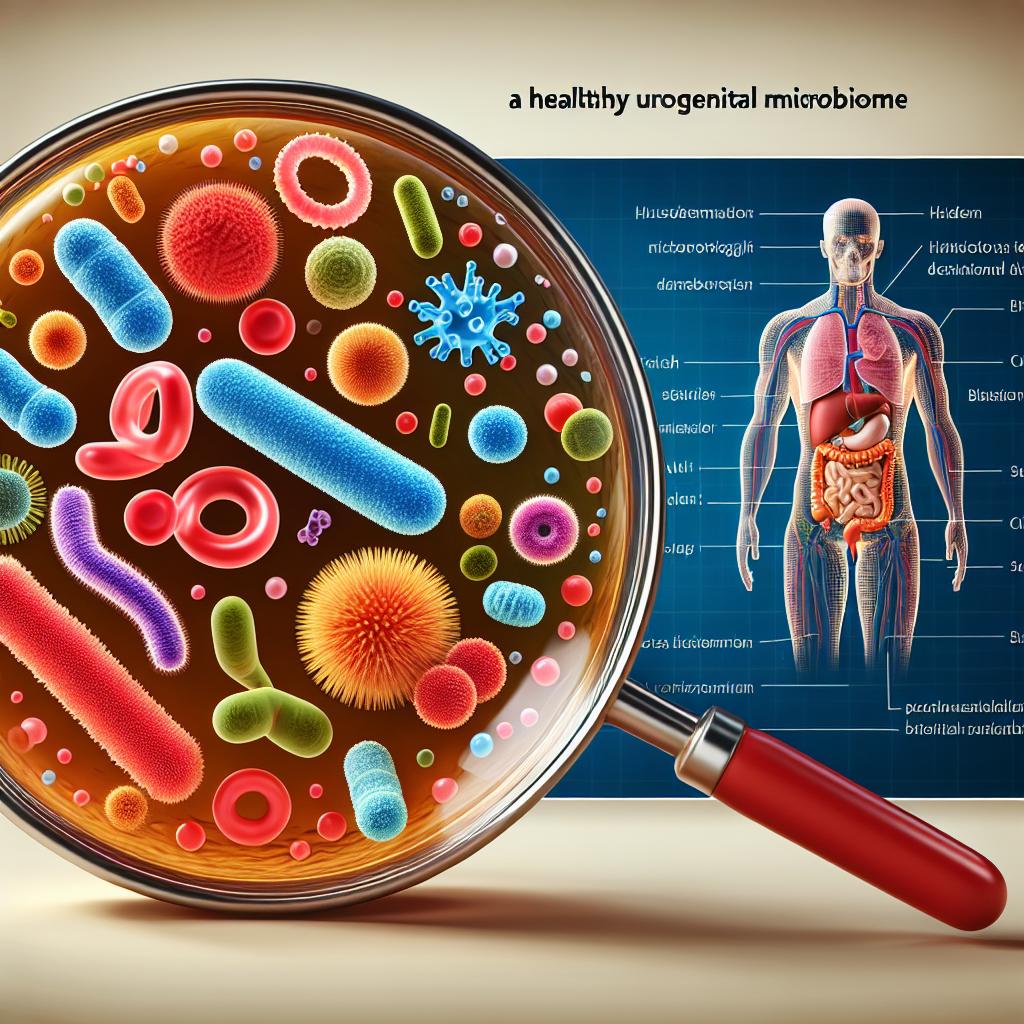
Mixed urogenital flora refers to the diverse population of microorganisms, including bacteria, fungi, and viruses, that inhabit the urogenital tract of both men and women. This ecosystem is characterized by the presence of various species that coexist in a delicate balance, contributing to the overall health of the host. In women, the vaginal microbiota is particularly important, as it plays a crucial role in preventing infections and maintaining reproductive health. The primary bacterial species found in a healthy vagina are Lactobacillus, which helps to maintain an acidic environment, thus inhibiting the growth of pathogenic organisms.
The composition of mixed urogenital flora can vary significantly among individuals and is influenced by several factors, including hormonal changes, sexual activity, hygiene practices, and the use of antibiotics. A balanced urogenital flora is essential for preventing conditions such as bacterial vaginosis, urinary tract infections (UTIs), and other reproductive health issues.
Importance of Balanced Urogenital Flora
Maintaining a balanced mixed urogenital flora is vital for several reasons. Firstly, a healthy microbiota protects against pathogen colonization. For instance, Lactobacillus species produce lactic acid, which helps to lower the pH of the vagina, creating an environment that is inhospitable to harmful bacteria (1). Furthermore, balanced flora can enhance the immune response by producing antimicrobial substances, which play a protective role against various infections (2).
Additionally, the microbiota contributes to the metabolic health of the host. It aids in the digestion of certain nutrients and the production of essential vitamins. Research has shown that disturbances in the urogenital microbiome can lead to significant health issues, including increased susceptibility to sexually transmitted infections (STIs) and reproductive health disorders (3). Therefore, understanding and maintaining a healthy balance of urogenital flora is crucial for overall health.
Factors Affecting Urogenital Flora Composition
Several factors influence the composition of mixed urogenital flora, including:
-
Hormonal Changes: Fluctuations in estrogen levels during menstrual cycles or menopause can significantly alter the vaginal microbiome. For example, decreased estrogen after menopause often leads to a reduction in Lactobacillus species and an increase in pathogenic bacteria (4).
-
Antibiotics: The use of antibiotics can disrupt the natural balance of the microbiome, leading to a decrease in beneficial bacteria and an overgrowth of harmful species. This dysbiosis can result in conditions like recurrent bacterial vaginosis and yeast infections (5).
-
Sexual Activity: Sexual intercourse can introduce new bacteria into the urogenital tract, altering the microbial balance. Additionally, the presence of multiple sexual partners can increase the risk of STIs, which can further disrupt the microbiome (6).
-
Hygiene Practices: The use of vaginal douches or certain hygiene products can disrupt the natural flora. It’s generally advised to avoid such practices, as they can lead to increased irritation and infections (7).
-
Diet: A diet high in processed foods and sugars may negatively impact the microbiome, while a diet rich in fiber can promote a healthy microbiota (8).
Understanding these factors is essential for maintaining the health of the urogenital microbiome and preventing related health issues.
Health Implications of Mixed Urogenital Flora
The health implications of mixed urogenital flora are significant. An imbalance in this ecosystem can lead to various health issues, including:
-
Bacterial Vaginosis: This condition arises when there is a decrease in Lactobacillus and an overgrowth of other bacteria. Symptoms may include discharge, odor, and irritation (9).
-
Urinary Tract Infections (UTIs): An imbalance can lead to higher susceptibility to UTIs, particularly in women. UTIs can cause painful urination, frequent urges to urinate, and abdominal pain (10).
-
Sexually Transmitted Infections (STIs): A disrupted microbiome can increase the risk of acquiring STIs, as the protective mechanisms offered by beneficial bacteria are compromised (11).
-
Pelvic Inflammatory Disease (PID): An unhealthy urogenital flora can lead to PID, a serious infection of the reproductive organs that can result in long-term complications such as infertility (12).
-
Genitourinary Syndrome of Menopause (GSM): As estrogen levels decline during menopause, changes in the vaginal flora can lead to GSM, characterized by dryness, irritation, and discomfort (13).
Maintaining a balanced mixed urogenital flora is essential for preventing these conditions and promoting overall reproductive health.
Strategies for Maintaining Healthy Urogenital Flora
To maintain a healthy balance of mixed urogenital flora, consider the following strategies:
-
Probiotics: Consuming probiotics, particularly Lactobacillus strains, can help restore and maintain a healthy vaginal microbiome. Probiotic supplements or foods like yogurt may be beneficial (14).
-
Dietary Choices: A diet rich in fruits, vegetables, and whole grains can promote a healthy microbiome. Reducing sugar and processed food intake is also recommended (15).
-
Hygiene Practices: Avoid douching and using harsh soaps in the genital area. Opt for gentle, unscented products to maintain the natural balance of bacteria (16).
-
Regular Medical Checkups: Regular gynecological exams can help monitor reproductive health and address any issues before they escalate. Discuss any symptoms or concerns with a healthcare provider (17).
-
Safe Sexual Practices: Use barrier methods during sexual activity to reduce the risk of STIs and potential disruptions to the microbiome. Additionally, consider limiting the number of sexual partners (18).
Implementing these strategies can help support the health of the urogenital microbiome and reduce the risk of associated health issues.
FAQs
What is mixed urogenital flora?
Mixed urogenital flora refers to the diverse community of microorganisms, including bacteria, fungi, and viruses, present in the urogenital tract, crucial for maintaining health and preventing infections.
How can I maintain a healthy urogenital flora?
You can maintain a healthy urogenital flora by consuming probiotics, eating a balanced diet, practicing good hygiene, having regular medical checkups, and engaging in safe sexual practices.
What are the signs of an imbalanced urogenital flora?
Signs of an imbalanced urogenital flora may include unusual discharge, odor, irritation, frequent urinary tract infections, and discomfort during intercourse.
Can antibiotics affect urogenital flora?
Yes, antibiotics can disrupt the natural balance of urogenital flora by killing beneficial bacteria, leading to conditions such as bacterial vaginosis and yeast infections.
Are there specific foods that promote a healthy urogenital microbiome?
Foods rich in probiotics, such as yogurt, kefir, and fermented vegetables, along with a diet high in fiber from fruits, vegetables, and whole grains, can promote a healthy urogenital microbiome.
References
-
Mohajan, D. (2023). Historical view of diabetics mellitus: from ancient Egyptian polyuria to discovery of insulin. Retrieved from https://doi.org/10.56397/SSSH.2023.07.05
-
Khursheed, R., Singh, S. K., & Wadhwa, S. (2019). Treatment strategies against diabetes: success so far and challenges ahead. European Journal of Pharmacology, 862, 172625. doi:10.1016/j.ejphar.2019.172625
-
Antman, M. (2024). Exploring cutting-edge approaches in diabetes care: from nanotechnology to personalized therapeutics. Naunyn-Schmiedeberg’s Archives of Pharmacology, 394(1), 1-19. doi:10.1007/s00210-024-03532-7
-
Barbot, M., Ceccato, F., & Scaroni, C. (2018). Diabetes mellitus secondary to Cushing’s disease. Frontiers in Endocrinology, 9, 284. doi:10.3389/fendo.2018.00284
-
Duxbury, M. S., Ito, H., Zinner, M. J., Ashley, S. W., & Whang, E. E. (2004). Focal adhesion kinase gene silencing promotes anoikis and suppresses metastasis of human pancreatic adenocarcinoma cells. Surgery, 135(5), 555-561. doi:10.1016/j.surg.2003.10.017
-
O’Sullivan, K. M., Ford, S. L., Longano, A., Kitching, A. R., & Holdsworth, S. R. (2018). Intrarenal Toll-like receptor 4 and Toll-like receptor 2 expression correlates with injury in antineutrophil cytoplasmic antibody-associated vasculitis. American Journal of Physiology-Renal Physiology, 315(4), F1283-F1294. doi:10.1152/ajprenal.00040.2018
-
Mazhar, M., Zhu, Y., & Qin, L. (2023). The interplay of dietary fibers and intestinal microbiota affects type 2 diabetes by generating short-chain fatty acids. Foods, 12(5), 1023. doi:10.3390/foods12051023
-
Kaur, M., Kumar, M., Parkash, J., & Prasad, D. N. (2019). Oral hypoglycemic drugs: an overview. Journal of Drug Delivery and Therapy, 9(3-s), 770-777. doi:10.22270/jddt.v9i3-s.2815
-
Zare, F., Ataollahi, E., & Mardaneh, P. (2024). A combination of virtual screening, molecular dynamics simulation, MM/PBSA, ADMET, and DFT calculations to identify a potential DPP4 inhibitor. Scientific Reports, 14, 7749. doi:10.1038/s41598-024-58485-x
-
Liu, H., Shan, X., & Yu, J. (2020). Recent advances in inhaled formulations and pulmonary insulin delivery systems. Current Pharmaceutical Biotechnology, 21(2), 180-193. doi:10.2174/138920102066619101115224831612824
-
Kopp, J. B., Anders, H. J., Susztak, K., et al. (2020). Podocyte A20/TNFAIP3 Controls Glomerulonephritis Severity via the Regulation of Inflammatory Responses and Effects on the Cytoskeleton. Cells, 14(5), 381. doi:10.3390/cells14050381
-
Köhler, P., Ribeiro, A., Honarpisheh, M., et al. (2025). Podocyte A20/TNFAIP3 Controls Glomerulonephritis Severity via the Regulation of Inflammatory Responses and Effects on the Cytoskeleton. Cells, 14(5), 381. doi:10.3390/cells14050381
-
Myeong, J., Lee, M., et al. (2025). Microbial metabolites control self-renewal and precancerous progression of human cervical stem cells. Nature Communications, 14, 57323. doi:10.1038/s41467-025-57323-6
-
Lam, L. N., Savage, K. E., Shakir, C. N., & Lemos, J. A. (2025). Genome-wide analysis of Enterococcus faecalis genes that facilitate interspecies competition with Lactobacillus crispatus. Journal of Bacteriology, 207(1), e00438-24. doi:10.1128/jb.00438-24
-
Wang, Y., Liu, Q., Kang, S.-G., et al. (2021). Dietary bioactive ingredients modulating the cAMP signaling in diabetes treatment. Nutrients, 13(9), 3038. doi:10.3390/nu13093038
-
Kimura, Y., Ichii, O., et al. (2023). Vaginal microbiota transplantation alleviates vaginal atrophy in ovariectomized mice. Scientific Reports, 12, 92881. doi:10.1038/s41598-025-92881-1
-
Zang, L., Hao, H., Liu, J., et al. (2017). Mesenchymal stem cell therapy in type 2 diabetes mellitus. Diabetology & Metabolic Syndrome, 9. doi:10.1186/s13098-017-0233-1
-
Barbier, A., & Coudray, C. (2023). Current Insights into Interactions Between Gut Microbiota and Diet in the Context of Diabetes Management. Nutrients, 15(8), 2053. doi:10.3390/nu15082053
-
Ramu, M., Vishal, S. S., & Gogia, N. (2022). Role of AMP-activated protein kinase and sirtuins as anti-aging proteins. In Anti-aging drug discovery on the basis of hallmarks of aging (pp. 241-278). Elsevier.
-
Duxbury, M. S., Ito, H., Zinner, M. J., Ashley, S. W., & Whang, E. E. (2004). Focal adhesion kinase gene silencing promotes anoikis and suppresses metastasis of human pancreatic adenocarcinoma cells. Surgery, 135(5), 555-561. doi:10.1016/j.surg.2003.10.017