Table of Contents
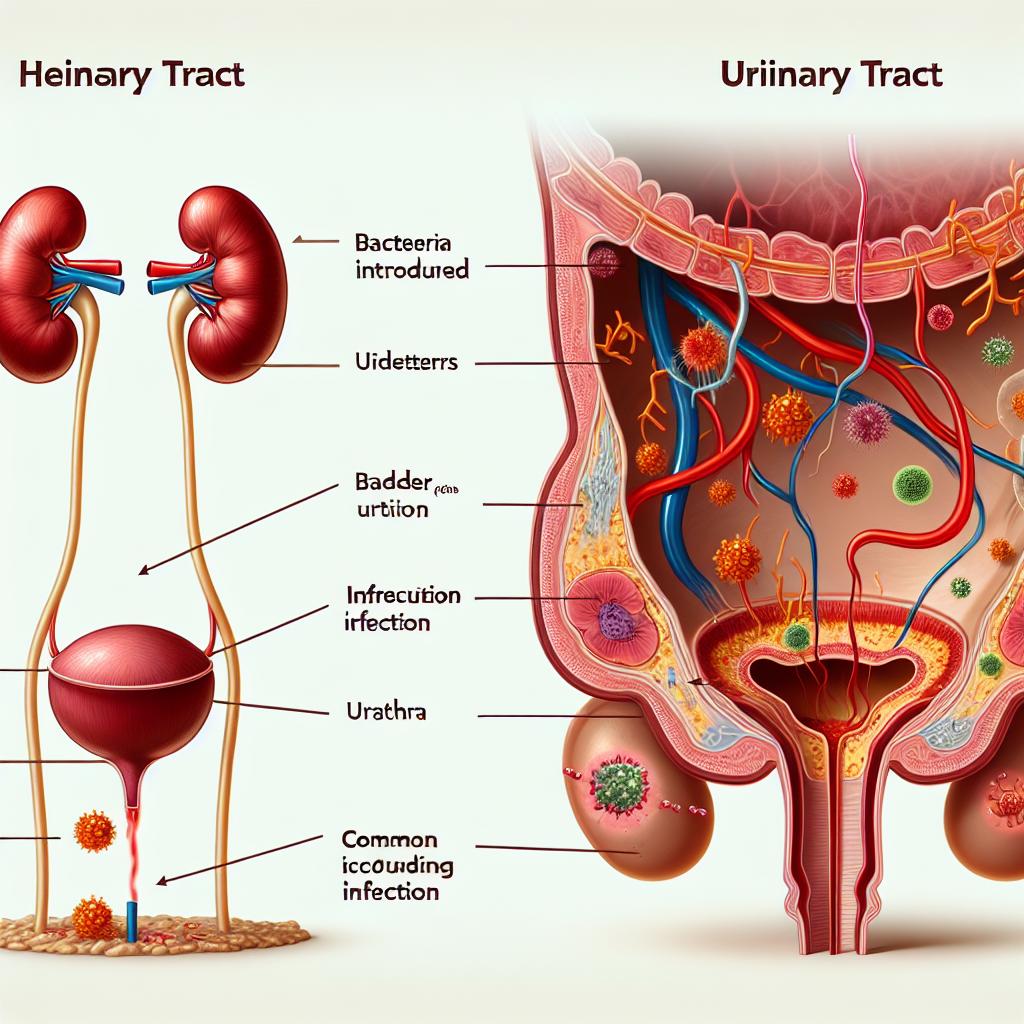
Causes of Lower Back Pain in UTI Patients
Lower back pain in UTI patients can arise from several factors. The infection can lead to inflammation and irritation of the urinary tract, which may radiate pain to the lower back. According to Brennand & Holroyd-Leduc (2025), the prevalence of urinary tract infections increases significantly after menopause due to decreased estrogen levels, which affect urogenital mucosal immunity. This can lead to changes in the urinary tract, making it more susceptible to infections that could manifest as back pain.
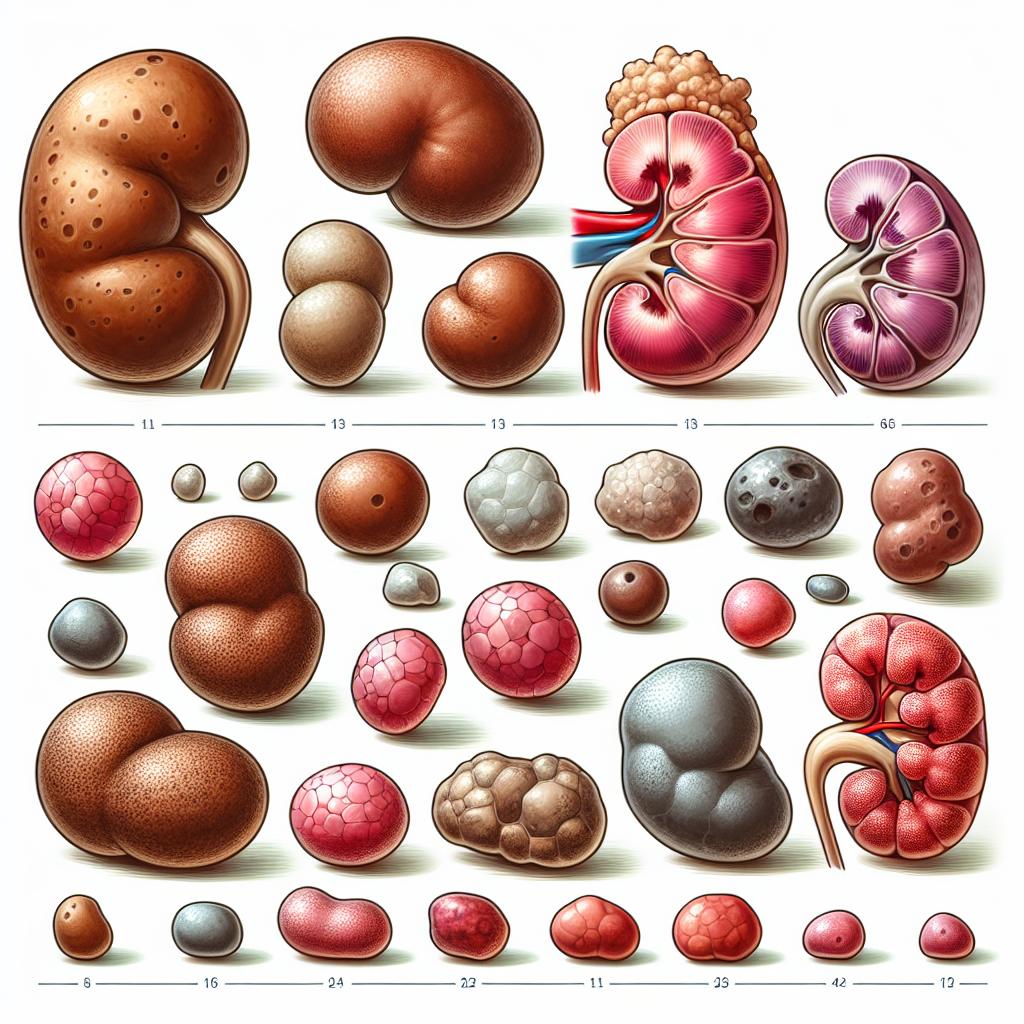
In addition to inflammation, the kidneys may also be involved, particularly if the infection ascends and leads to pyelonephritis, an infection of the kidneys characterized by flank pain, which is often confused with lower back pain. The presence of kidney stones may also contribute to lower back pain and is a common complication associated with recurrent Utis (Brennand & Holroyd-Leduc, 2025).
Symptoms of UTI That May Not Include Fever
While fever is a common symptom of UTIs, many individuals, especially older adults, may not exhibit this sign. Symptoms of a UTI without fever can include:
- Dysuria: Pain or burning sensation during urination.
- Increased urinary frequency: A strong urge to urinate often.
- Urgency: A sudden, compelling need to urinate.
- Suprapubic pain: Discomfort in the lower abdomen.
- Changes in urine appearance: Cloudy or foul-smelling urine.
- Hematuria: Presence of blood in the urine.
Older adults may also present with atypical symptoms, such as confusion or delirium, which can complicate the diagnosis of UTIs (Brennand & Holroyd-Leduc, 2025). These symptoms can lead to misdiagnosis or delayed treatment, particularly in cases where lower back pain is the primary complaint.
Diagnosis of UTI When Experiencing Back Pain
Diagnosing a UTI in patients presenting with lower back pain requires a comprehensive approach. The following steps are often taken:
- Patient History: A detailed history is vital, focusing on urinary symptoms, sexual history, and any recent catheterization or surgeries.
- Physical Examination: This may include a focused abdominal examination and a digital rectal examination in male patients to assess for prostatitis.
- Urinalysis: A dipstick test can quickly identify nitrites, leukocyte esterase, and blood, which are indicators of infection.
- Urine Culture: A definitive diagnosis requires a urine culture to identify the causative organism and determine antibiotic sensitivity (Brennand & Holroyd-Leduc, 2025).
- Imaging Studies: In cases where pyelonephritis or structural abnormalities are suspected, imaging such as ultrasound or CT scans may be warranted.
It is crucial to consider that the absence of fever does not rule out a UTI, particularly in older adults or immunocompromised patients. The criteria for diagnosing UTIs should also consider the patient’s symptoms and the results of the urinalysis and culture.
Treatment Options for UTI-Related Lower Back Pain
The treatment of UTIs, especially when lower back pain is a presenting symptom, typically involves antibiotic therapy. The choice of antibiotics depends on the sensitivity of the bacteria isolated from urine cultures. Common first-line treatments include:
- Nitrofurantoin: 50 mg four times daily for five days.
- Trimethoprim-sulfamethoxazole (TMP-SMX): 800 mg/160 mg twice daily for three days.
- Fosfomycin: A single dose of 3 g is effective for uncomplicated Utis.
In cases where lower back pain is severe, pain management may also include:
- NSAIDs: Such as ibuprofen or naproxen, to relieve pain and inflammation.
- Acetaminophen: For pain relief, especially in individuals who cannot take NSAIDs.
Patients experiencing recurrent UTIs may benefit from prophylactic antibiotics or non-antibiotic strategies, such as vaginal estrogen therapy for postmenopausal women, as suggested by Brennand & Holroyd-Leduc (2025).
When to Seek Medical Attention for UTI Symptoms
It is essential to seek medical attention if any of the following occurs:
- Persistent or worsening lower back pain.
- The onset of fever or chills.
- Nausea or vomiting.
- Symptoms of dehydration (such as dizziness or light-headedness).
- Symptoms of acute kidney injury (such as decreased urination or swelling).
Prompt medical evaluation is crucial, particularly in patients with underlying health conditions or those at risk for complications from UTIs.
FAQs
What should I do if I suspect I have a UTI but no fever?
If you suspect a UTI, it is important to consult with a healthcare provider for an evaluation and appropriate testing, even if you do not have a fever.
Can a UTI cause lower back pain without fever?
Yes, a UTI can cause lower back pain without fever, particularly if the infection is affecting the bladder or ascending to the kidneys.
What are the common antibiotics prescribed for UTIs?
Common antibiotics prescribed for UTIs include nitrofurantoin, trimethoprim-sulfamethoxazole, and fosfomycin, based on urine culture results.
When should I seek immediate medical help for UTI symptoms?
Seek immediate medical help if you experience severe lower back pain, fever, chills, or symptoms indicating potential kidney involvement, such as nausea or vomiting.
References
- Brennand, E. A., & Holroyd-Leduc, J. (2025). Urinary tract infections after menopause. Canadian Medical Association Journal. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11790305/
- Alishahi Tabriz, A., Turner, K., Hong, Y. R., Gheytasvand, S., Powers, B. D., & Elston Lafata, J. (2022). Trends and Characteristics of Potentially Preventable Emergency Department Visits Among Patients With Cancer in the US. JAMA Netw Open, 6(1), e2250423
- Hidalgo-Tenorio, C., & Sánchez-Vázquez, M. (2022). Implementation of 2% Chlorhexidine Bathing to Reduce Healthcare-Associated Infections Among Patients in the Intensive Care Unit. BMC Public Health. https://doi.org/10.1186/s12889-025-21553-6
- Ibrahim, R., Aranjani, J. M., Kalikot Valappil, & Nair, G. (2025). Unveiling the potential bacteriophage therapy: a systematic review. Future Science OA
- Yilmaz, S. (2023). Understanding oncologic emergencies and related emergency department visits and hospitalizations: a systematic review. BMC Emerg Med. https://doi.org/10.1186/s12873-025-01183-2