Table of Contents
Importance of Urogenital Flora Present in Maintaining Health
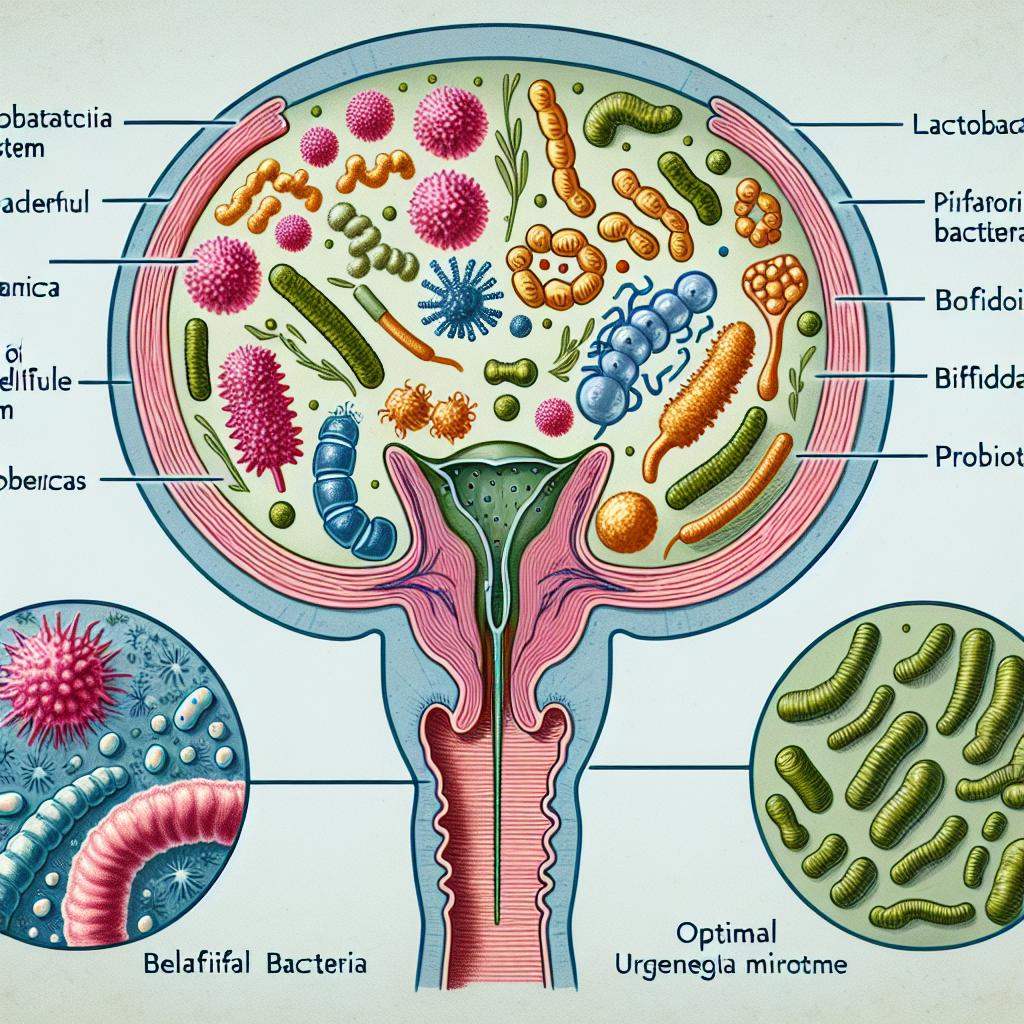
The urogenital flora, primarily composed of various microorganisms, plays a crucial role in maintaining women’s health. This intricate ecosystem, dominated by Lactobacillus species, helps to protect against infections, maintain normal pH levels, and support overall reproductive health. The presence of a diverse and balanced vaginal microbiota is vital for preventing conditions such as bacterial vaginosis (BV) and vulvovaginal candidiasis (VVC), which can lead to more severe health issues if left unchecked (van Teijlingen et al., 2024).
The urogenital microbiome serves multiple protective functions, including the production of lactic acid, which lowers vaginal pH and creates an inhospitable environment for pathogenic bacteria (Geijtenbeek et al., 2025). Moreover, a healthy vaginal flora enhances the immune response by promoting the activity of local immune cells, thereby reducing susceptibility to sexually transmitted infections and other reproductive tract diseases (Meng et al., 2025).
Factors Affecting the Urogenital Flora Present in Women
Several factors influence the composition and stability of the urogenital flora in women. Hormonal changes, particularly during puberty, menstruation, pregnancy, and menopause, significantly impact the vaginal ecosystem. For instance, fluctuations in estrogen levels during the menstrual cycle can alter the microbiome’s composition, leading to increased susceptibility to infections (Mao et al., 2025).
Lifestyle factors, such as diet, sexual activity, and hygiene practices, also play a pivotal role in shaping the urogenital flora. Diets high in refined sugars and processed foods can disrupt the balance of beneficial bacteria, while regular intake of probiotics can help restore a healthy microbiome (Geijtenbeek et al., 2025). Smoking and the use of certain medications, such as antibiotics, can further disturb the vaginal microbiota, increasing the risk of infections (van Teijlingen et al., 2024).
| Factors Affecting Urogenital Flora | Impact |
|---|---|
| Hormonal Changes | Alters composition; increases infection risk |
| Diet | High sugar disrupts balance; probiotics restore health |
| Sexual Activity | Affects microbial diversity |
| Hygiene Practices | Proper hygiene supports healthy flora |
| Medications (e.g., antibiotics) | Can disturb flora balance |
Role of Hormones on Urogenital Flora Present During Menopause
Menopause leads to significant hormonal changes, particularly a decrease in estrogen levels, which can profoundly affect the urogenital flora. This decline results in vaginal atrophy, characterized by thinning of the vaginal epithelium, reduced lubrication, and increased susceptibility to infections (Mao et al., 2025). The decrease in estrogen diminishes the glycogen content in vaginal epithelial cells, reducing the substrate available for Lactobacillus to produce lactic acid, thereby increasing vaginal pH and promoting the growth of pathogenic bacteria (Geijtenbeek et al., 2025).
The genitourinary syndrome of menopause (GSM) encompasses symptoms associated with this hormonal shift, including vaginal dryness, burning sensations, and recurrent urinary tract infections (Mao et al., 2025). Hormone replacement therapy (HRT) has been shown to alleviate some of these symptoms by restoring estrogen levels, thereby promoting a healthier vaginal environment and improving the urogenital flora (Meng et al., 2025).
Urogenital Flora Present and Its Connection to Infections
The balance of the urogenital flora is essential in preventing infections. A decline in Lactobacillus species, often observed during hormonal changes or after antibiotic use, can lead to dysbiosis, characterized by an overgrowth of pathogenic bacteria, such as Gardnerella or Candida species (van Teijlingen et al., 2024). This dysbiosis is closely linked to conditions like bacterial vaginosis and vulvovaginal candidiasis, which can cause significant discomfort and lead to more severe health issues if untreated (Meng et al., 2025).
Recent studies have indicated that vaginal dysbiosis can also impact systemic health, including increasing the risk of acquiring sexually transmitted infections (STIs) such as HIV (Geijtenbeek et al., 2025). The presence of certain bacterial species, such as Prevotella timonensis, has been associated with enhanced HIV transmission due to their effect on dendritic cell function, highlighting the importance of maintaining a healthy vaginal microbiome (van Teijlingen et al., 2024).
| Infection Type | Associated Flora Changes | Health Impact |
|---|---|---|
| Bacterial Vaginosis | Decreased Lactobacillus, increased Gardnerella | Increased risk of STIs |
| Vulvovaginal Candidiasis | Decreased Lactobacillus, increased Candida | Discomfort, risk of recurrent infections |
Therapeutic Approaches to Restore Healthy Urogenital Flora Present
Restoring a healthy urogenital flora can significantly improve women’s health outcomes and reduce the risk of infections. Various therapeutic approaches are being explored, including probiotics, vaginal microbiota transplantation (VMT), and hormone replacement therapy (HRT).
Probiotics, particularly those containing Lactobacillus species, have been shown to restore and maintain a healthy vaginal microbiome. Clinical studies suggest that oral or intravaginal probiotics can help in preventing recurrent bacterial vaginosis and candidiasis (Meng et al., 2025). Additionally, VMT is emerging as a promising therapy, where healthy donor microbiota is transplanted into women experiencing dysbiosis, showing positive results in restoring balance and alleviating symptoms (van Teijlingen et al., 2024).
HRT remains a cornerstone in managing symptoms associated with menopause and GSM. By restoring estrogen levels, HRT can enhance the vaginal environment, promoting the growth of beneficial bacteria and improving overall urogenital health (Mao et al., 2025).
| Therapeutic Approach | Mechanism of Action | Expected Outcome |
|---|---|---|
| Probiotics | Restore Lactobacillus dominance | Enhanced vaginal health, reduced infections |
| Vaginal Microbiota Transplantation | Introduce healthy microbial communities | Rebalance flora, alleviate symptoms |
| Hormone Replacement Therapy | Restore estrogen levels, improve vaginal environment | Alleviate GSM symptoms, improve flora |
FAQ
What is urogenital flora?
Urogenital flora refers to the collection of microorganisms, including bacteria, fungi, and viruses, residing in the urogenital tract, which play a crucial role in maintaining reproductive health.
How does menopause affect urogenital flora?
Menopause leads to decreased estrogen levels, resulting in vaginal atrophy, changes in the urogenital flora, and increased susceptibility to infections.
What are the signs of dysbiosis in the urogenital flora?
Signs of dysbiosis may include abnormal vaginal discharge, irritation, itching, and an increased frequency of infections such as bacterial vaginosis and candidiasis.
How can I restore a healthy urogenital flora?
Restoring a healthy urogenital flora can be achieved through probiotics, vaginal microbiota transplantation, and hormone replacement therapy, depending on individual health needs.
Are probiotics effective for vaginal health?
Yes, probiotics containing Lactobacillus species can help restore and maintain a healthy vaginal microbiome, reducing the risk of infections.
References
-
Geijtenbeek, T. B. H., van Teijlingen, N. H., Sarrami-Forooshani, R., et al. (2025). Vaginal Prevotella timonensis Bacteria Enhance HIV‐1 Uptake and Differentially Affect Transmission by Distinct Primary Dendritic Cell Subsets. Immunologic Research. https://doi.org/10.1007/s12026-025-09606-9
-
Mao, X., Zhang, Y., Wang, Z., et al. (2025). Vaginal microbiota transplantation alleviates vaginal atrophy in ovariectomized mice. Scientific Reports. https://doi.org/10.1038/s41598-025-92881-1
-
Meng, J., Xiao, H., Xu, F., et al. (2025). Systemic barrier dysfunction in type 2 inflammation diseases: perspective in the skin, airways, and gastrointestinal tract. Immunologic Research. https://doi.org/10.1007/s12026-025-09606-9
-
van Teijlingen, N. H., Helgers, L. C., Zijlstra-Willems, E. M., et al. (2024). The prevalence and risk factors of vaginal Candida species and group B Streptococcus colonization in pregnant women attending antenatal care at Hawassa university comprehensive specialized hospital in Hawassa City, Southern Ethiopia. BMC Pregnancy and Childbirth. https://doi.org/10.1186/s12884-025-07402-9
-
Wang, X., Liu, X., Jiang, Y., et al. (2025). Influences of gestational diabetes mellitus on the changes in the vaginal microbiota from antepartum to postpartum. BMC Pregnancy and Childbirth. https://doi.org/10.1186/s12884-025-07411-8