Table of Contents
Factors Influencing UTI Development Timeline
The timeframe for UTI development is influenced by various factors, including anatomical, physiological, and environmental elements. Anatomical differences, such as the shorter urethra in women compared to men, facilitate quicker bacterial access to the bladder. Hormonal changes during pregnancy or menopause can also alter urinary tract dynamics, contributing to UTI susceptibility (Yeung et al., 2025).
Additionally, lifestyle factors play a significant role. High sugar intake, inadequate hydration, and poor hygiene practices increase the risk of developing UTIs. For instance, dehydration can lead to urinary stasis, allowing bacteria to multiply (Yeung et al., 2025). Furthermore, sexual activity can facilitate bacterial entry into the urinary tract, particularly during menstruation when the vaginal flora may be disrupted (Yeung et al., 2025).
Typical Duration for UTI Symptoms to Appear
UTI symptoms can develop rapidly, often within a few hours to a few days after bacterial infection. The incubation period varies depending on the individual’s immune response and the virulence of the causative bacteria. Common symptoms include increased urinary frequency, urgency, burning sensation during urination, and cloudy or strong-smelling urine (Yeung et al., 2025). If left untreated, UTIs can progress to more severe symptoms, such as fever, chills, and flank pain, indicating possible kidney involvement (Yeung et al., 2025).
How Risk Factors Affect UTI Onset
Several risk factors contribute to the onset of UTIs, with some individuals being more predisposed than others. These risk factors include:
- Age: Older adults may experience structural changes in the urinary tract, leading to increased susceptibility.
- Sexual Activity: Women who are sexually active are at a higher risk due to the potential introduction of bacteria into the urinary tract.
- Pregnancy: Hormonal changes and anatomical shifts during pregnancy can create an environment conducive to bacterial growth (Yeung et al., 2025).
- Diabetes: Individuals with diabetes are more prone to infections due to compromised immune function and increased glucose levels in urine, which serve as a nutrient source for bacteria (Yeung et al., 2025).
- Catheter Use: Indwelling catheters can introduce bacteria directly into the bladder, increasing the risk of UTIs.
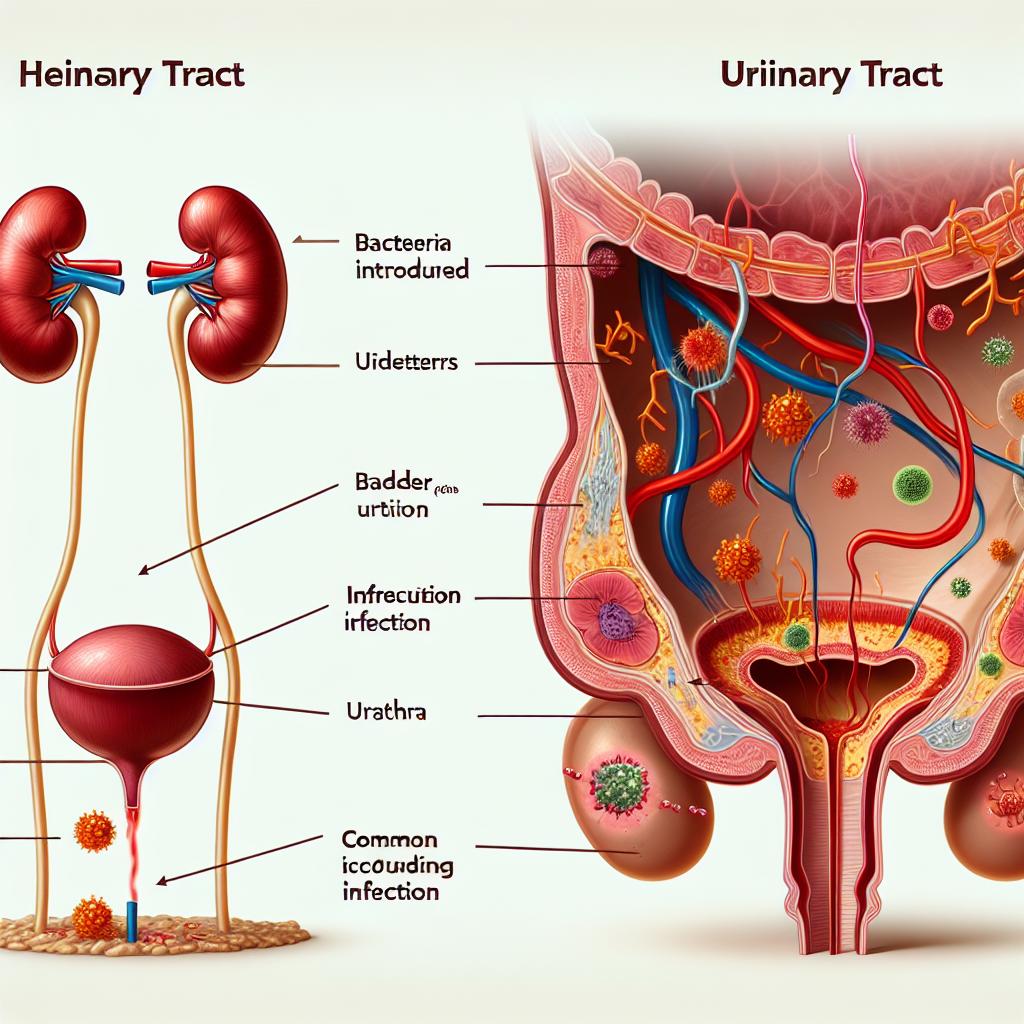
The Role of Bacterial Growth in UTI Development
Bacterial growth is central to UTI development. The most common pathogens responsible for UTIs include Escherichia coli (E. coli), which accounts for approximately 80-90% of cases. These bacteria adhere to the uroepithelium, evade the host’s immune response, and multiply rapidly, leading to infection (Yeung et al., 2025).
The adherence of bacteria to the urinary tract is facilitated by fimbriae, which allow them to latch onto the uroepithelial cells. Once established, the infection can cause inflammation and damage to the bladder wall, leading to the characteristic symptoms of a UTI (Yeung et al., 2025). Moreover, bacterial biofilms can form, making the infection more difficult to treat and increasing the likelihood of recurrent Utis.
Importance of Early Detection and Treatment of UTIs
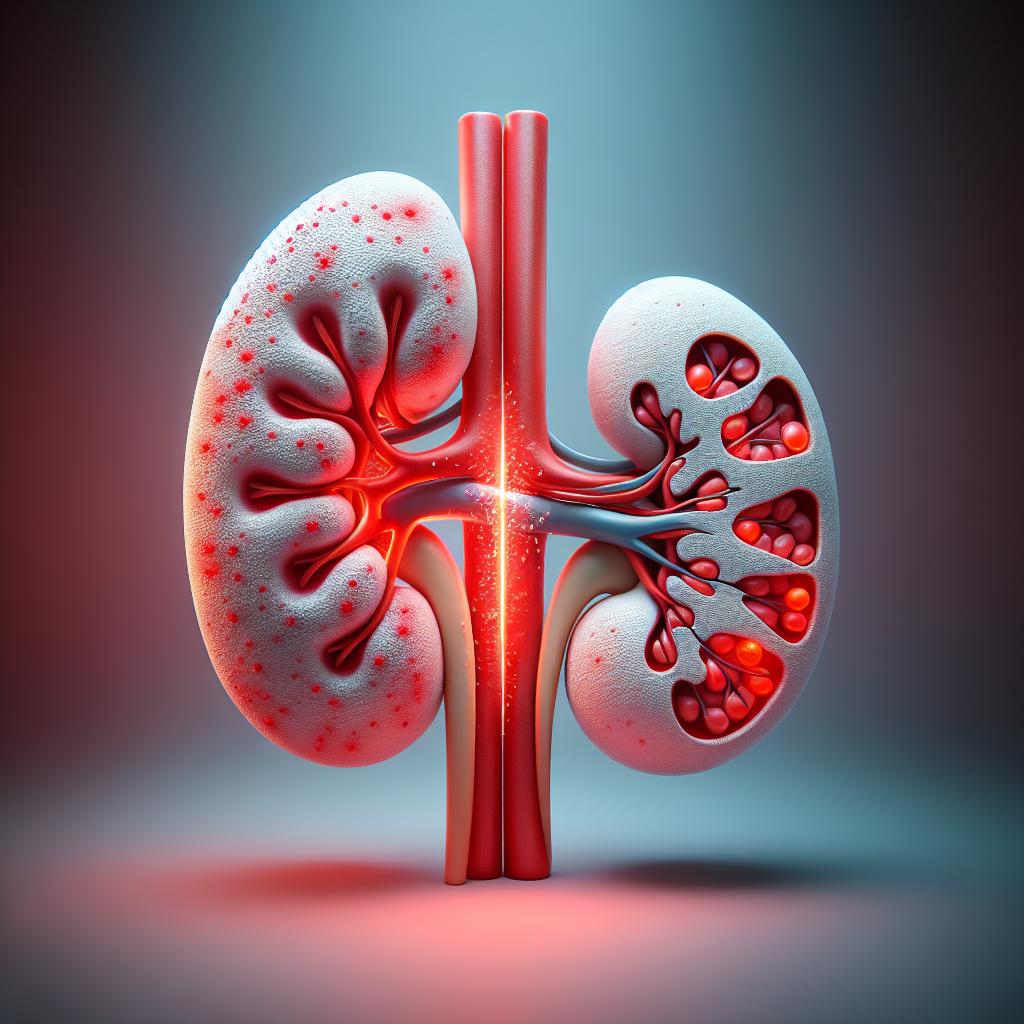
Early detection and treatment of UTIs are crucial to prevent complications, such as pyelonephritis (kidney infection) and sepsis. A delay in treatment can lead to severe outcomes, particularly in vulnerable populations such as pregnant women, the elderly, and individuals with diabetes (Yeung et al., 2025).
Diagnosis typically involves a urinalysis and culture to identify the causative organism and determine antibiotic sensitivity. Prompt treatment with appropriate antibiotics can significantly shorten the duration of symptoms and reduce the risk of complications. It is also essential to educate patients on preventive measures, such as proper hydration, hygiene practices, and post-coital urination, to minimize the risk of recurrent infections (Yeung et al., 2025).
Table 1: Common Urological Complications During Pregnancy
| Urological Complication | Description | Prevalence | Causes/Contributors | Potential Impact |
|---|---|---|---|---|
| Urinary Tract Infections (UTIs) | Most common urological issue in pregnancy affecting urinary tract function. | Approximately 10% of pregnant women | Hormonal changes, urinary stasis, incomplete bladder emptying. | Increased risk of preterm birth, low birth weight, fetal mortality. |
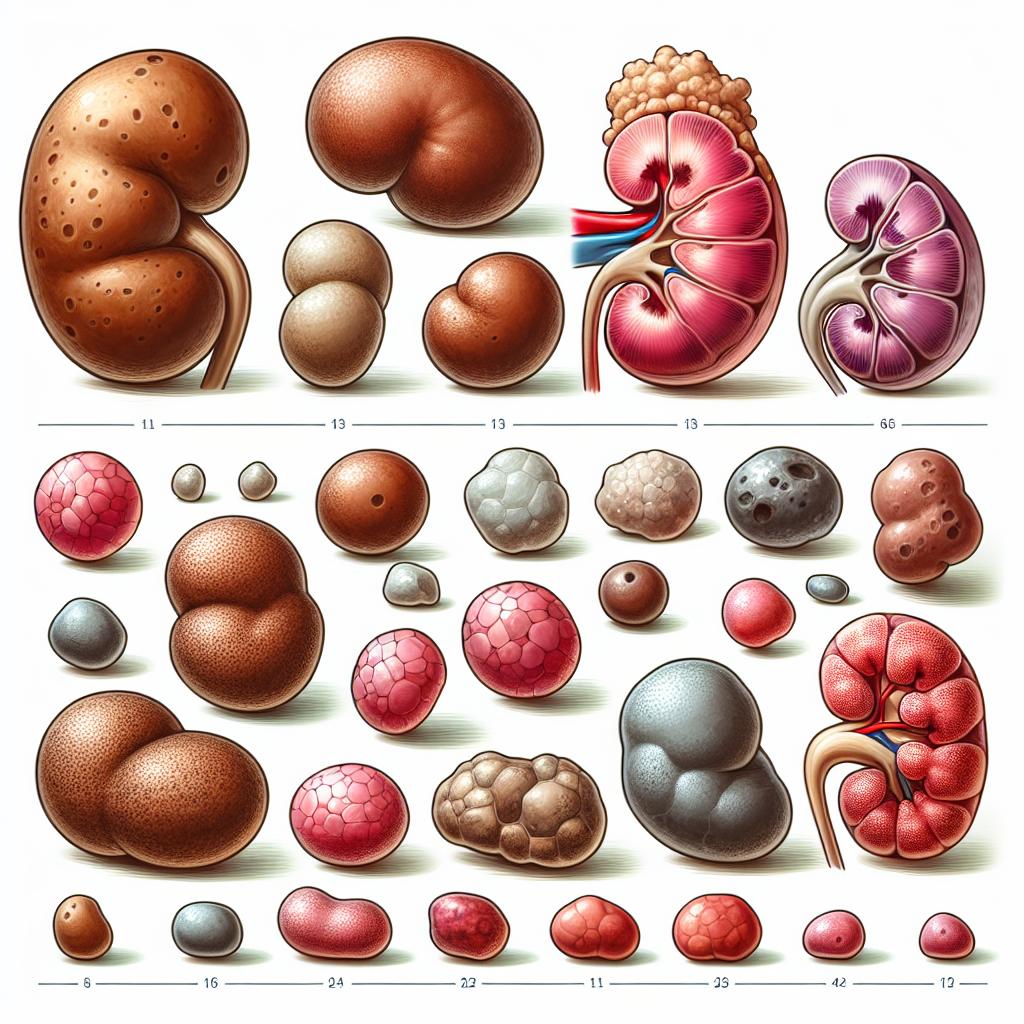
| Kidney Stones (Nephrolithiasis) | Less common but significant, causing severe pain and potential complications. | Ranges from 1 in 200 to 1 in 1500 pregnancies | Increased renal calcium excretion, decreased urine pH. | Can lead to renal colic, obstructive uropathy, infection, and preterm labor if untreated. |
| Bladder Dysfunction | Includes urinary incontinence and overactive bladder (OAB). | Up to 50% of pregnant women experience some degree. | Pressure from expanding uterus, hormonal relaxation of pelvic floor muscles. | Can cause significant discomfort, emotional distress, and increase risk of postpartum incontinence. |
Table 2: The Impact of Urological Complications on Maternal and Fetal Health During Pregnancy
| Urological Complication | Potential Impact on Maternal Health | Potential Impact on Fetal Health |
|---|---|---|
| Urinary Tract Infections (UTIs) | Can progress to acute pyelonephritis, increasing risk of maternal sepsis. | Increased risk of preterm birth, low birth weight, and fetal mortality. |
| Kidney Stones (Nephrolithiasis) | Can cause severe pain and renal colic. | Increased risk of preterm labor due to severe pain and complications. |
| Bladder Dysfunction | Can cause significant discomfort and emotional distress. | Generally less immediate impact on fetal health. |
FAQ Section
What are the common symptoms of a UTI?
Common symptoms include increased frequency and urgency of urination, burning sensation during urination, cloudy or strong-smelling urine, and pelvic pain.
How can UTIs be prevented during pregnancy?
Preventive measures include staying hydrated, practicing good hygiene, urinating after intercourse, and avoiding irritants like douches and scented products.
What should I do if I suspect I have a UTI?
If you suspect a UTI, it’s essential to consult a healthcare provider for diagnosis and appropriate treatment.
Can UTIs affect pregnancy?
Yes, untreated Utis can lead to complications such as preterm labor, low birth weight, and even fetal mortality.
What are the risk factors for developing UTIs?
Risk factors include being female, being sexually active, having a history of UTIs, pregnancy, diabetes, and urinary tract abnormalities.
References
- Yeung, G. Y. C., Albers, C. A. W., Smalbrugge, M., de Bruijne, M. C., Jepma, P., & Joling, K. J. (2025). Audit and group feedback in nursing home physician groups: lessons learned from a qualitative study. BMC Health Services Research. Retrieved from https://doi.org/10.1186/s12913-025-12355-y
- Tse, J. H. S., & et al. (2002). Clinical outcomes of pediatric kidney transplantation in Hong Kong. Journal of Pediatrics. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11865298/
- Ward, M. M., & et al. (2011). Rising incidence of pediatric kidney stones. Urology. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11851757/
- Mørkved, S., & et al. (2019). Effectiveness of pelvic floor muscle training for urinary incontinence: A systematic review. Obstetrics & Gynecology. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11835077/
- Angelescu, R., & et al. (2016). Antibiotic treatment for urinary tract infections in pregnancy: A systematic review. Infectious Diseases in Obstetrics and Gynecology. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11835077/