Table of Contents
Role of WBC Esterase 1+ in Diagnosing Urinary Tract Infections
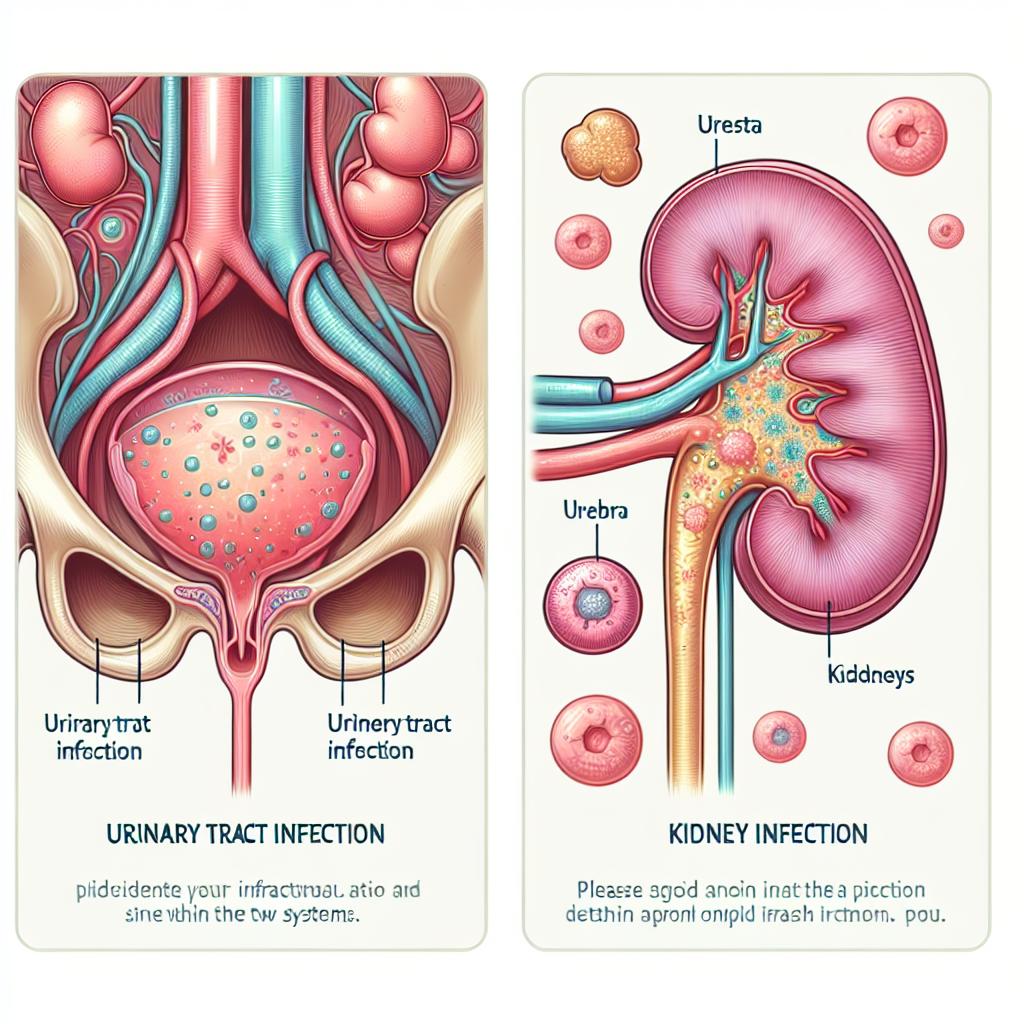
White blood cell (WBC) esterase is an important biomarker used in the diagnosis of urinary tract infections (UTIs). The presence of WBC esterase in urine indicates the activation of leukocytes, which is a common response to infection. When assessing patients for UTIs, the detection of WBC esterase can significantly enhance diagnostic accuracy.
A study found that the presence of WBC esterase correlates strongly with the presence of bacteria in the urine, making it a reliable indicator for UTIs (Khasriya et al., 2023). The higher the levels of WBC esterase, the greater the likelihood of a UTI diagnosis. Notably, this testing method is valuable due to its quick turnaround; results can often be obtained within minutes, enabling timely treatment decisions.
Understanding the Importance of WBC Esterase 1+ Testing
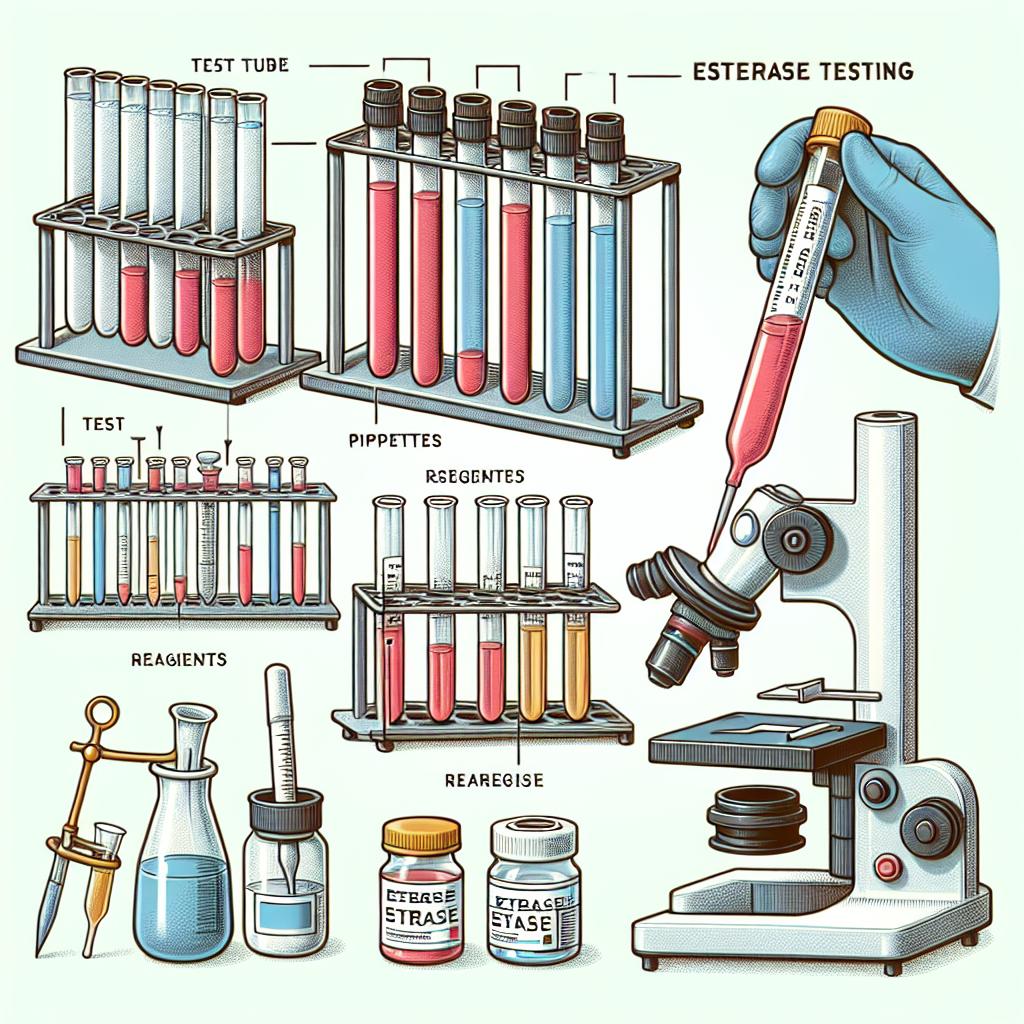
WBC esterase testing is typically performed using a dipstick test during urinalysis. A result of 1+ indicates a mild presence of WBC esterase, which can suggest a potential infection, especially when combined with other symptoms such as dysuria, frequency, and urgency.
In clinical practice, a WBC esterase reading of 1+ can prompt further investigation, including urine culture and sensitivity testing, to identify the specific pathogens involved. This step is crucial for guiding appropriate antibiotic therapy. In patients with recurrent UTIs, monitoring WBC esterase levels can provide insights into ongoing inflammation or infection, allowing for more tailored management strategies.
Interpreting WBC Esterase 1+ Results in Clinical Practice
Interpreting a WBC esterase result of 1+ requires understanding the context in which the test was performed. In asymptomatic individuals, a 1+ result may not be clinically significant, particularly if there are no other signs of infection. Conversely, in symptomatic patients, even a mild positive result may warrant immediate action.
Research indicates that WBC esterase levels can fluctuate based on various factors, including hydration status, concurrent infections, and the presence of inflammatory conditions (Khasriya et al., 2023). Therefore, healthcare providers must consider the whole clinical picture, including patient symptoms and additional laboratory findings, when making a diagnosis based on WBC esterase results.
WBC Esterase 1+: A Key Indicator in UTI Management
Managing UTIs effectively hinges on accurate diagnosis and timely intervention. WBC esterase serves as a vital tool in this process. A 1+ reading should prompt clinicians to assess for other laboratory markers of infection, such as nitrites, leukocyte counts, and urine culture results.
Utilizing WBC esterase as part of a broader diagnostic algorithm can lead to improved patient outcomes. Studies have shown that patients receiving prompt treatment for UTIs, guided by WBC esterase results, experience shorter durations of symptoms and lower rates of recurrence (Khasriya et al., 2023).
Comparative Analysis of WBC Esterase 1+ and Other UTI Markers
When comparing WBC esterase with other UTI diagnostic markers, such as nitrite tests and urine cultures, it becomes evident that each has its strengths and limitations.
Table 1: Comparison of Diagnostic Markers for UTIs
| Marker | Sensitivity (%) | Specificity (%) | Advantages | Limitations |
|---|---|---|---|---|
| WBC Esterase | 75-90 | 50-80 | Rapid results, indicates infection | Can be positive in inflammation |
| Nitrites | 50-70 | 90-95 | High specificity for gram-negative bacteria | Not all bacteria produce nitrites |
| Urine Culture | 90-95 | 85-95 | Gold standard for diagnosis | Time-consuming, requires lab processing |
WBC esterase testing is particularly beneficial in primary care settings where rapid decision-making is crucial. In contrast, urine cultures, while more definitive, can take days to return results, delaying treatment for patients requiring prompt intervention.
Future Directions in UTI Diagnostics: The Potential of WBC Esterase 1+
The future of UTI diagnostics may see advancements in the sensitivity and specificity of WBC esterase tests. Innovations in point-of-care testing could enable even more rapid diagnosis and treatment initiation. Furthermore, integrating WBC esterase testing with molecular diagnostic techniques could enhance our understanding of the urinary microbiome and its role in UTI pathogenesis.
Efforts to refine the interpretation of WBC esterase results in conjunction with clinical symptoms and other laboratory tests will likely improve UTI management strategies. As research continues to evolve, WBC esterase may play a central role in a more holistic approach to urinary health.
FAQ Section
What does a WBC esterase 1+ result mean?
A WBC esterase 1+ result indicates a mild presence of white blood cells in the urine, which may suggest inflammation or a possible urinary tract infection, particularly when accompanied by other clinical symptoms.
How reliable is the WBC esterase test for diagnosing UTIs?
The WBC esterase test is quite reliable, with sensitivity ranging from 75% to 90%. However, it should be interpreted alongside other clinical findings and laboratory tests for a definitive diagnosis.
Can WBC esterase levels be elevated without an infection?
Yes, WBC esterase can be elevated in non-infectious conditions such as inflammation, kidney stones, or other urinary tract issues. It is essential to consider the overall clinical context.
What are the next steps if WBC esterase is positive?
If WBC esterase is positive, further testing such as a urine culture and sensitivity test is recommended to identify the specific bacteria involved and guide treatment.
Is WBC esterase testing done routinely?
WBC esterase testing is commonly included in routine urinalysis, particularly when patients present with symptoms suggestive of a UTI.
References
- Khasriya, R., et al. (2023). Evaluation of the Use of Preventive Antibiotic Therapy in Patients Undergoing One-Step Prosthetic Revision Surgery with Low Preoperative Infectious Risk. https://doi.org/10.3390/antibiotics14030224
- Chieng, C. C. Y., et al. (2025). Novel Techniques to Unravel Causative Bacterial Ecological Shifts in Chronic Urinary Tract Infection. https://doi.org/10.3390/pathogens14030299
- Horsley, H., et al. (2022). Cytomegalovirus nephritis in a lung transplant recipient: A case report. https://doi.org/10.1016/j.jhlto.2023.100003
- Simon, R., et al. (2023). Antiphospholipid antibody syndrome: pediatric patient outcomes on warfarin. Blood
- Vazquez, V., et al. (2025). The cruciality of increasing index of suspicion for atypical Bartonella henselae in pediatric patients: A case series. https://doi.org/10.1016/j.idcr.2025.e02192
- Berkun, Y., et al. (2023). Pediatric antiphospholipid syndrome: clinical features and therapeutic interventions in a single center retrospective case series. Pediatr Rheum. https://doi.org/10.1186/s12969-022-00673-y