Table of Contents
The Role of Amoxicillin in UTI Treatment
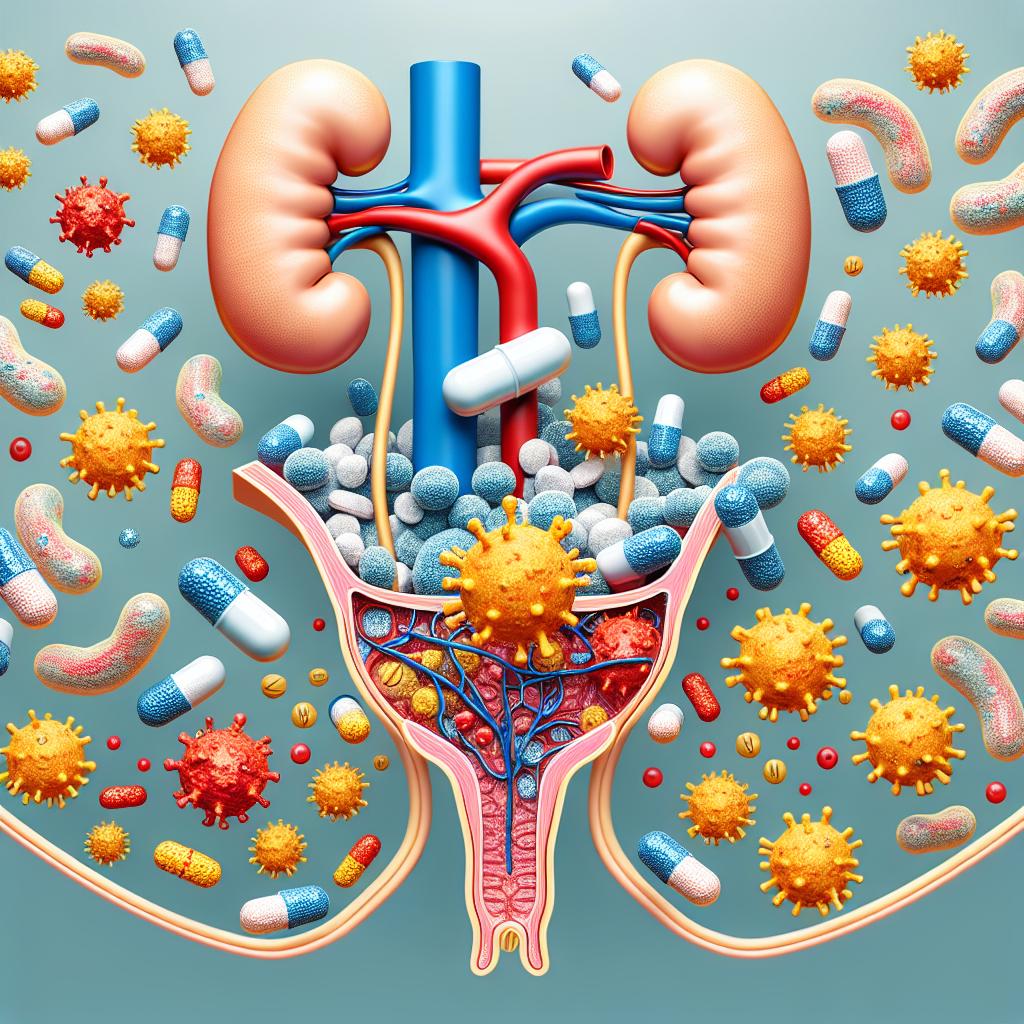
Urinary tract infections (UTIs) are among the most prevalent bacterial infections globally, leading to millions of hospital visits and substantial healthcare costs each year. An estimated 400 million UTIs occur annually, with a significant number of these cases leading to serious complications such as pyelonephritis and sepsis (1). The primary causative agent of UTIs is Escherichia coli (E. coli), responsible for 80-90% of cases. Other pathogens can also be involved, especially in complicated UTIs (2).
Amoxicillin, a penicillin-type antibiotic, is often considered for treating uncomplicated Utis due to its effectiveness against common uropathogens. While it is generally well-tolerated and has a broad spectrum of activity, the rise of antimicrobial resistance poses a challenge to its efficacy in some populations (3). Understanding the clinical context in which amoxicillin is prescribed is crucial for effective UTI management.
Efficacy of Amoxicillin Against Uropathogens
The effectiveness of amoxicillin in treating UTIs largely depends on the susceptibility profile of the causative uropathogen. Studies show that E. coli strains are increasingly developing resistance to amoxicillin and other beta-lactam antibiotics (4). The Clinical and Laboratory Standards Institute (CLSI) and the European Committee on Antimicrobial Susceptibility Testing (EUCAST) provide guidelines for determining susceptibility, which are crucial in selecting appropriate antibiotics (5).
Recent data indicate a concerning trend: resistance rates for amoxicillin among E. coli isolates vary significantly depending on geographic location and local antimicrobial stewardship practices. A study conducted in Brazil found that while 100% of strains were susceptible to carbapenems, only 73.58% were susceptible to amoxicillin (6). This underscores the importance of local antibiograms to guide empirical therapy in UTI cases.
Table 1: Antimicrobial Resistance Patterns for E. coli in UTI Cases
| Antibiotic | Susceptibility Rate (%) | Resistance Rate (%) |
|---|---|---|
| Amoxicillin | 73.58 | 26.42 |
| Piperacillin | 85.0 | 15.0 |
| Nitrofurantoin | 88.68 | 11.32 |
| Ciprofloxacin | 78.7 | 21.3 |
| Meropenem | 100 | 0 |
| Gentamicin | 90.5 | 9.5 |
*Data compiled from recent studies on urinary tract infections (6, 7).
Recommended Dosage and Treatment Duration for UTIs
The recommended dosage of amoxicillin for treating uncomplicated UTIs typically involves administering 500 mg every 8 hours for a duration of 7 to 14 days. This extended duration is particularly important for pregnant women and patients with recurrent Utis, as it ensures the complete eradication of the infection (7).
For patients with complicated UTIs, the duration may be adjusted based on clinical response and urine culture results. It is essential to perform follow-up urine cultures to confirm the resolution of infection, especially in populations at high risk of recurrent infections (8).
Potential Side Effects of Amoxicillin in UTI Patients
While generally safe, amoxicillin can cause side effects in some patients. Common adverse effects include gastrointestinal issues like diarrhea, nausea, and vomiting. Severe allergic reactions, although rare, can occur and manifest as hives, difficulty breathing, or swelling of the face and throat (9).
In pediatric populations, careful monitoring is required due to the potential for developing antibiotic-associated diarrhea, often linked to Clostridium difficile infection (10). In light of these potential side effects, clinicians should provide patients with clear instructions regarding the use of amoxicillin and educate them about the signs of allergic reactions.
Table 2: Common Side Effects of Amoxicillin
| Side Effect | Frequency |
|---|---|
| Diarrhea | Common |
| Nausea | Common |
| Vomiting | Common |
| Rash (allergic reaction) | Rare |
| Anaphylaxis | Very Rare |
*Adverse effects listed according to clinical guidelines (9, 10).
Alternatives to Amoxicillin for Urinary Tract Infections
Given the rising rates of antibiotic resistance, alternative antibiotics are often utilized when amoxicillin is ineffective. These include:
- Nitrofurantoin: Particularly effective against uncomplicated UTIs caused by E. coli, with a favorable safety profile in pregnant women, except in the last trimester due to risk of hemolytic anemia in newborns (11).
- Trimethoprim/Sulfamethoxazole: A combination antibiotic frequently used; however, resistance rates are increasing (12).
- Fosfomycin: A single-dose treatment option for uncomplicated UTIs, noted for its efficacy and low resistance profile (13).
- Fluoroquinolones: Such as ciprofloxacin, generally reserved for complicated cases due to potential side effects and resistance concerns (14).
Table 3: Alternative Antibiotics for UTI Treatment
| Antibiotic | Indication | Resistance Concerns |
|---|---|---|
| Nitrofurantoin | Uncomplicated UTIs | Low |
| Trimethoprim/Sulfamethoxazole | Uncomplicated UTIs | Increasing |
| Fosfomycin | Uncomplicated UTIs | Low |
| Fluoroquinolones | Complicated UTIs | High |
*Alternative treatment options and their indications (11, 12, 13, 14).
Conclusion
Amoxicillin remains a viable option for treating uncomplicated urinary tract infections, but its efficacy is increasingly compromised by the emergence of resistant strains of E. coli. Local antibiograms should guide empirical therapy, ensuring the most effective treatment decisions based on current resistance patterns. Clinicians must also consider alternative antibiotics and the potential side effects associated with amoxicillin, tailoring their approach to each patient’s clinical scenario.
Frequently Asked Questions (FAQ)
What is the first-line treatment for UTIs? The first-line treatment for uncomplicated UTIs typically includes amoxicillin or nitrofurantoin. The choice depends on local resistance patterns and patient-specific factors.
How long should antibiotics be taken for a UTI? Antibiotics are usually prescribed for 7 to 14 days for uncomplicated UTIs, while complicated cases may require longer treatment durations.
What are the side effects of amoxicillin? Common side effects of amoxicillin include gastrointestinal disturbances like diarrhea and nausea, as well as allergic reactions that can occur in rare cases.
Are there alternatives to amoxicillin for UTIs? Yes, alternatives include nitrofurantoin, trimethoprim/sulfamethoxazole, fosfomycin, and fluoroquinolones, depending on the resistance patterns and patient factors.
How can I prevent UTIs? Preventative measures include staying hydrated, practicing good hygiene, and urinating after sexual intercourse to help flush out bacteri
References
- Antimicrobial resistance: Global burden and trends. (2023). Retrieved from https://pubmed.ncbi.nlm.nih.gov/11837515/
- The role of pharmacological interventions in managing urological complications during pregnancy and childbirth: A review. (2023). Retrieved from https://pubmed.ncbi.nlm.nih.gov/11835077/
- Urinary tract infection (UTI) management. (2023). Retrieved from https://doi.org/10.3390/pathogens14020141
- Antimicrobial Susceptibility Patterns in UTIs. (2023). Retrieved from https://doi.org/10.3390/microorganisms13020231
- State of the Art of Antimicrobial and Diagnostic Stewardship in Pediatric Setting. (2023). Retrieved from https://doi.org/10.3390/antibiotics14020132
- Machine learning for predicting antimicrobial resistance in critical and high-priority pathogens: A systematic review. (2023). Retrieved from https://doi.org/10.1371/journal.pone.0319460
- Drivers of inappropriate use of antibiotics among community members in low- and middle-income countries: A systematic review. (2023). Retrieved from https://doi.org/10.1186/s12889-025-21553-6
- A Precision Medicine Model for Targeted Antibiotic Therapy in Urinary Tract Infections. (2023). Retrieved from https://doi.org/10.3390/antibiotics14020211