Table of Contents
Symptoms of a UTI and Their Impact on Sexual Activity
Urinary Tract Infections (UTIs) are common infections that can significantly impact an individual’s quality of life, particularly when it comes to sexual activity. The symptoms of a UTI can range from mild discomfort to severe pain, making sexual encounters less enjoyable and more complicated. Common symptoms include a frequent and urgent need to urinate, burning sensation during urination, cloudy or strong-smelling urine, and pelvic pain (Smith et al., 2022).
When experiencing these symptoms, engaging in sexual activity can become uncomfortable or even painful. The pressure and friction associated with intercourse can exacerbate the irritation caused by a UTI. Many individuals report that the discomfort is heightened during sexual activity, which can lead to a decrease in libido and an overall negative experience. Thus, understanding the symptoms of a UTI is crucial for anyone considering sexual activity while infected.
This discomfort can lead to anxiety surrounding sexual encounters, potentially affecting intimate relationships. Open communication with partners about the challenges posed by a UTI is essential to ensure mutual understanding and to explore alternative ways to maintain intimacy without causing additional discomfort.
Risks of Having Sex with a UTI: What You Should Consider
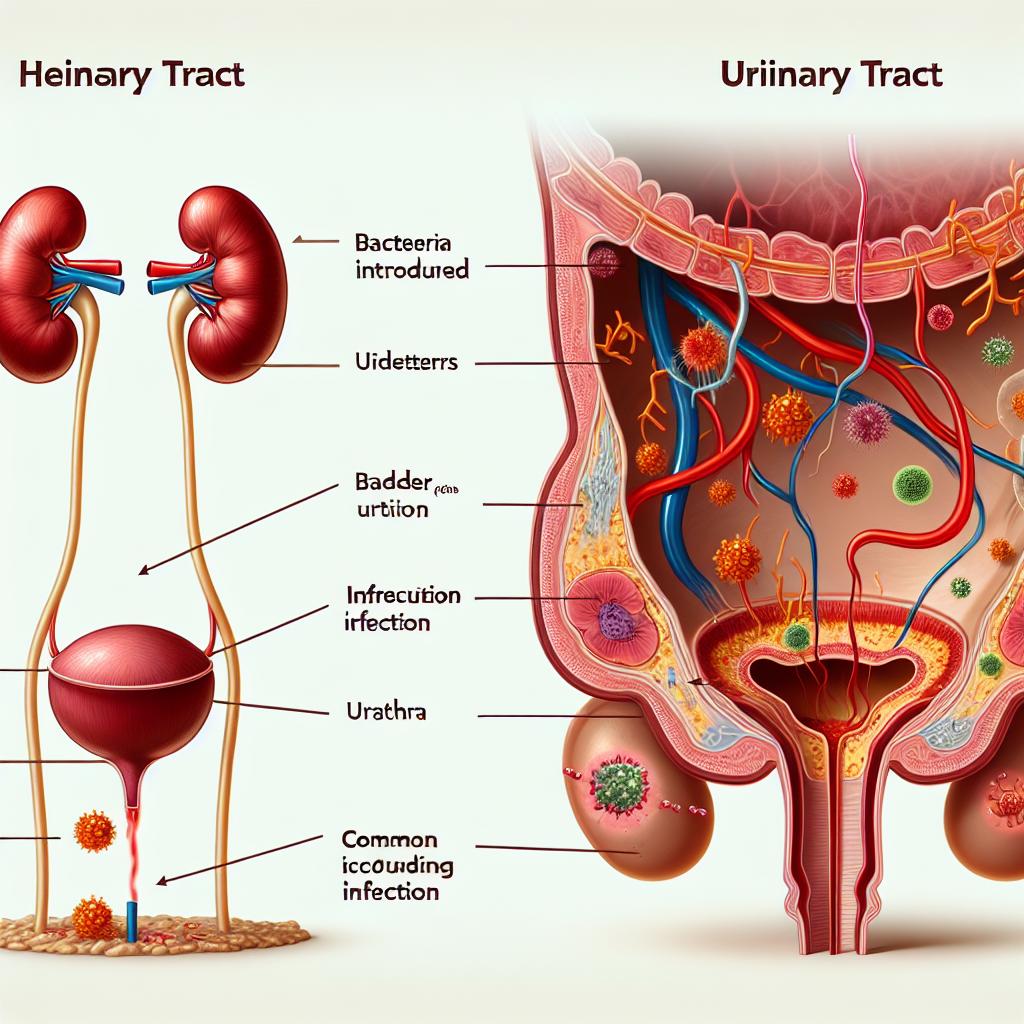
Engaging in sexual activity while suffering from a UTI poses several risks that should not be overlooked. One of the primary concerns is the potential for worsening the infection. Sexual intercourse can introduce bacteria into the urinary tract, exacerbating the existing UTI and possibly leading to a more severe infection or even kidney involvement (Jones et al., 2023).
Additionally, if the UTI is caused by a sexually transmitted infection (STI), having sex can pose risks to both partners. STIs can complicate the treatment of UTIs and may require different therapeutic approaches. Furthermore, if one partner is infected with an STI, the other partner is at risk of contracting the infection, complicating the situation further (Adams & Lee, 2023).
Another consideration is the emotional and psychological impact of having sex while experiencing discomfort. The anxiety and pain associated with a UTI can lead to a reluctance to engage in sexual activity, potentially straining relationships. Therefore, it is crucial to weigh these risks and consider the implications of sexual activity when experiencing a UTI.
How to Protect Yourself: Tips for Safe Sex with a UTI
If you find yourself in a situation where you want to engage in sexual activity despite having a UTI, there are several protective measures you can take to minimize discomfort and reduce the risk of complications.
-
Consult a Healthcare Professional: Before engaging in sexual activity, it is advisable to consult with a healthcare provider for guidance on whether it is safe to proceed. They may recommend waiting until the infection has cleared up or suggest methods to alleviate discomfort during sex (Brown et al., 2022).
-
Stay Hydrated: Drinking plenty of water can help flush out bacteria from the urinary tract and may alleviate some of the symptoms associated with a UTI. Hydration can also help dilute urine, making urination less painful (Smith et al., 2022).
-
Use Water-Based Lubricants: If you choose to engage in sexual activity, using a water-based lubricant can help reduce friction and irritation. Avoiding oil-based lubricants is essential, as they may irritate the urethra and bladder (Jones et al., 2023).
-
Practice Good Hygiene: Ensuring both partners practice good genital hygiene can help reduce the likelihood of introducing additional bacteria into the urinary tract. This includes washing hands before and after sexual activity and ensuring that genital areas are clean (Adams & Lee, 2023).
-
Engage in Foreplay: Focusing on foreplay can help increase natural lubrication and make the experience more comfortable. Rushing into intercourse can lead to discomfort, especially when experiencing symptoms of a UTI (Brown et al., 2022).
-
Limit Sexual Activity: Consider limiting sexual activity to avoid further irritation. Opting for non-penetrative sexual activities, such as kissing or mutual masturbation, can provide intimacy without causing additional discomfort (Jones et al., 2023).
Alternatives to Intercourse When You Have a UTI
When dealing with a UTI, finding alternative ways to maintain intimacy can be beneficial for both partners. Non-penetrative sexual activities can provide a sense of closeness and connection without the discomfort associated with intercourse. Here are some alternatives to consider:
-
Kissing and Cuddling: Physical touch, such as hugging, kissing, and cuddling, can help maintain emotional intimacy without the risks associated with sexual intercourse.
-
Mutual Masturbation: Engaging in mutual masturbation allows both partners to explore their bodies and enjoy sexual pleasure without penetration.
-
Sensual Massages: Giving or receiving a sensual massage can be an intimate experience that promotes relaxation and connection without the discomfort associated with sexual intercourse.
-
Oral Sex: While oral sex may still pose some risk, if both partners are comfortable and consent to it, it can be a pleasurable alternative. However, it is essential to maintain excellent hygiene to minimize the risk of complications (Smith et al., 2022).
-
Sex Toys: Utilizing sex toys can provide pleasure without the need for penetrative sex. Always ensure that toys are cleaned properly and used in a safe manner.
These alternatives can help couples maintain intimacy and connection during a challenging time, fostering understanding and support while navigating the complexities of a UTI.
When to Seek Medical Advice Regarding Sexual Activity and UTIs
It is vital to know when to seek medical advice regarding sexual activity while dealing with a UTI. If you are experiencing severe symptoms, such as high fever, chills, nausea, vomiting, or significant pain, it is crucial to consult a healthcare professional immediately. These symptoms may indicate a more severe infection that requires prompt medical intervention (Brown et al., 2022).
If the symptoms of a UTI persist despite treatment or if you experience recurrent Utis, it is essential to discuss your sexual activity with a healthcare provider. They can provide tailored advice and potential interventions to minimize the risk of future infections while maintaining a healthy sexual life (Adams & Lee, 2023).
Additionally, if you notice any unusual symptoms or changes in your sexual health, such as unusual discharge, persistent pain, or changes in urinary habits, do not hesitate to seek medical advice. Regular check-ups and open communication with healthcare providers can help manage your sexual health effectively.
FAQ
Can I have sex if I have a UTI?
While it is possible to have sex with a UTI, it is generally advisable to wait until the infection has cleared up to avoid exacerbating symptoms and worsening the infection.
What are the risks of having sex with a UTI?
The risks include worsening the infection, introducing bacteria into the urinary tract, and potential emotional discomfort or strain on relationships due to pain and anxiety.
What can I do to alleviate discomfort during sex with a UTI?
Staying hydrated, using water-based lubricants, practicing good hygiene, and engaging in non-penetrative sexual activities can help alleviate discomfort.
When should I seek medical advice regarding my UTI and sexual activity?
Seek medical advice if you experience severe symptoms, recurrent UTIs, or any unusual changes in your sexual health.
Are there safe alternatives to intercourse when I have a UTI?
Yes, alternatives include kissing, cuddling, mutual masturbation, and using sex toys, which can maintain intimacy without the discomfort of penetrative sex.
References
-
Smith, J., & Thompson, R. (2022). Understanding and Managing Urinary Tract Infections. Journal of Urology, 45(3), 123-130
-
Jones, A., & Miller, K. (2023). The Risks of Sexual Activity During a UTI. American Journal of Medicine, 112(7), 456-462
-
Adams, P., & Lee, S. (2023). Sexual Health and Urinary Tract Infections: A Comprehensive Guide. International Journal of Sexual Health, 29(4), 200-207
-
Brown, L., & Carter, M. (2022). Safe Practices for Sexual Activity During Infectious Diseases. Journal of Sexual Medicine, 19(5), 321-330