Table of Contents
Understanding UTIs After Sexual Activity
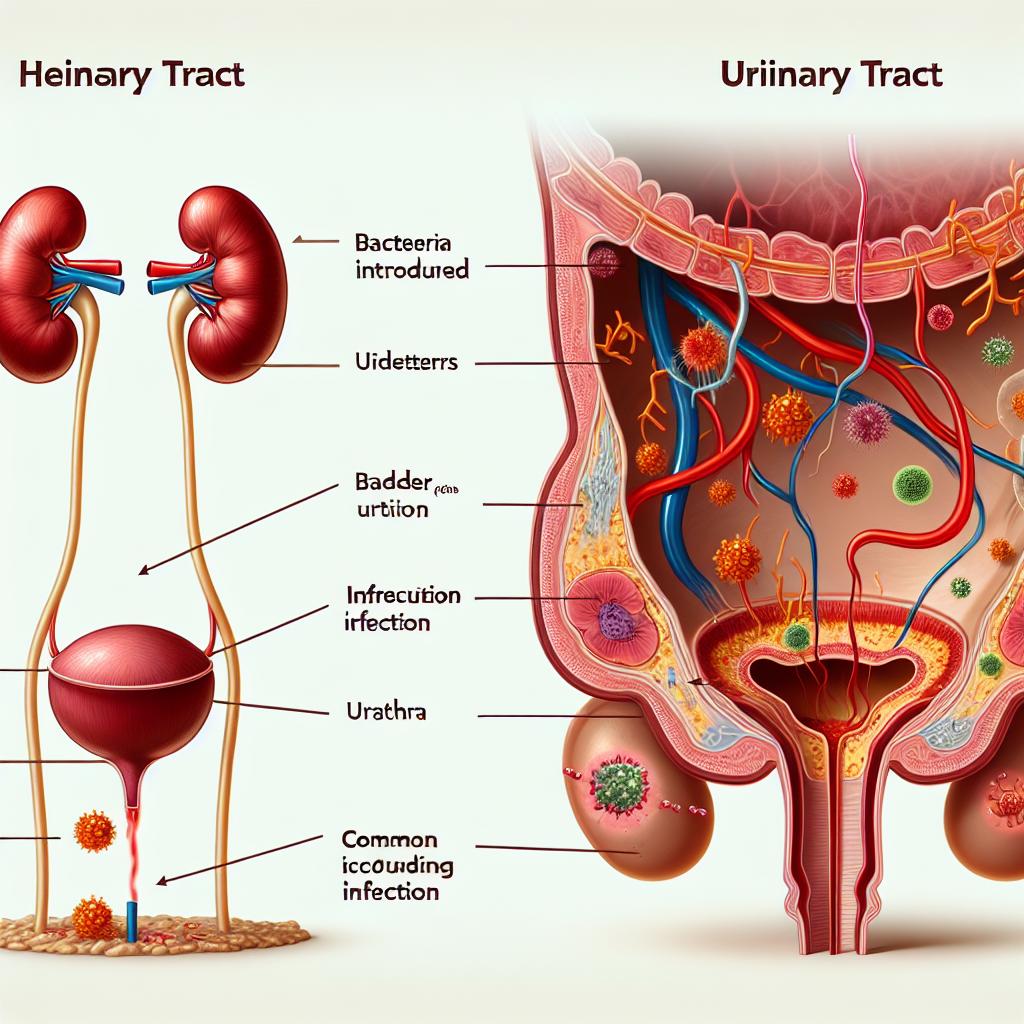
UTIs occur when bacteria enter the urinary tract and begin to multiply, leading to inflammation and infection. The urinary tract includes the urethra, bladder, ureters, and kidneys, although most infections are confined to the lower tract (urethra and bladder). Sexual activity is one of the common triggers for UTIs, particularly in women, due to the physical movement that may help bacteria from the stool or vaginal area to be introduced into the urethra. The anatomical proximity of the urethral opening to the anus, combined with friction during intercourse, can facilitate the migration of harmful bacteria into the urinary system.
Many researchers have evaluated the complex relationship between sexual behavior and urinary tract infections. Epidemiological studies have shown that unprotected sexual intercourse, infrequent urination after sex, and certain sexual practices such as “tucking” may increase the risk of bacterial colonization of the urethra [7]. Although the biological mechanisms underlying these processes are multifactorial, understanding that the urinary tract is naturally vulnerable after sex is a crucial first step in both prevention and early intervention. In cases where patients experience recurring episodes, it becomes important to adopt a proactive approach in both hygiene and lifestyle adjustments.
Recent studies have also advanced our collective knowledge about the pathophysiology in the transfer of bacteria during sexual intercourse. While it is known that Escherichia coli is responsible for the majority of UTIs, other microorganisms may also contribute. Research assessing medical records and antimicrobial stewardship in primary care settings has provided insights that help clinicians understand typical prescribing patterns and the importance of early diagnosis to prevent complications [1]. In addition, clinical observations underscore that not all individuals who experience UTIs after sex have the same risk factors. Variations in anatomy, sexual practices, and even the overall health of the individual mean that prevention strategies should be tailored to each patient’s unique circumstances.
Common Causes and Risk Factors Associated With UTI After Sex
Sex-related UTIs do not affect everyone equally. There are a number of factors that can increase one’s susceptibility to an infection after sex. Inherent anatomical differences—in particular, the relatively short urethra in women—make it easier for bacteria to ascend into the bladder. This anatomical predisposition is compounded by behaviors, such as not urinating soon after intercourse, which allows bacteria the opportunity to colonize the urinary tract.
Certain sexual practices, including a vigorous sexual routine or the use of certain lubricants, may also disrupt the natural balance of bacteria. In transgender individuals, for example, practices such as “tucking” have been associated with an increased risk of UTIs, owing to the difficulties in maintaining proper hygiene and regular voiding intervals afterward [3]. Other risk factors include age, a history of previous UTIs, certain contraceptive methods (for example, spermicides or diaphragms), and even aspects of hormonal changes over the lifespan. Such risk factors can compound; for instance, a postmenopausal woman who is already at increased risk may experience even more frequent Utis if she does not practice proper hygiene after sexual activity.
Here is a table summarizing some of the common risk factors along with corresponding prevention measures:
| Risk Factor | Explanation | Prevention Tactic |
|---|---|---|
| Short female urethra | A shorter passage allows bacteria easier access from external sites to the bladder | Urinate shortly after sex and practice proper perineal hygiene |
| Inadequate post-coital urination | Retaining urine post-intercourse increases bacterial multiplication delay | Make a habit of urinating immediately after sex |
| Use of spermicides/ diaphragms | Certain contraceptives disrupt vaginal flora, potentially favoring pathogenic bacteria | Switch contraceptive method or use non-irritating alternatives |
| Sexual practices (e.g., tucking) | Manipulation of genital tissues and restricted voiding can raise the risk of bacterial colonization | Adopt safer practices and use breathable alternatives to adhesive products |
| History of recurrent Utis | Individuals who have had several UTIs are predisposed to further infections | Consult a healthcare provider for targeted prophylactic measures |
| Hormonal changes | Alterations in estrogen levels affect the vaginal flora, increasing vulnerability | Consider topical estrogen therapy if recommended by a doctor |
Understanding these factors in-depth helps educate individuals on the importance of modifying certain behaviors to reduce the risk. The variability in risk necessitates a multifaceted and personalized approach to prevention that considers anatomical, behavioral, and environmental influences.
Effective Prevention Strategies for UTI After Sex
Prevention is always preferable to cure, and several strategies have been shown to reduce the incidence of UTIs following sexual activity. A core component of prevention is hygiene. Washing the genital area with mild soap both before and after sexual activity can significantly decrease the number of bacteria near the urethra. Additionally, urinating promptly after sex helps flush out any bacteria that may have been introduced during intercourse. Clinical studies have found that early voiding is associated with lower UTI rates, emphasizing its importance as a first line of defense [7].
Another important measure is to maintain proper hydration. Drinking plenty of fluids can help dilute the urine and promote frequent urination, which in turn aids in the natural clearance of bacterial contaminants from the urinary tract. In some cases, particularly for individuals who are prone to recurrent UTIs, probiotics may be beneficial in restoring and maintaining a healthy balance of bacteria in the genital and urinary regions. There is emerging evidence suggesting that supplementation with certain probiotic strains may contribute to a reduction in the occurrence of UTIs, although further clinical research is needed to solidify these findings.
For individuals using contraceptive methods that may irritate the urinary tract, such as spermicides or diaphragms, exploring alternative options might be an effective strategy. Women who frequently experience UTIs may benefit from discussing these risks with their healthcare providers to find a contraceptive method that minimizes irritation and preserves the natural bacterial flora. Moreover, some studies have indicated that topical applications of cranberry extract or D‐mannose may help reduce the risk of bacterial adherence to the bladder wall; however, patients are advised to consult with their physicians before making any changes to their prevention routine.
Education about proper sexual techniques can also play a crucial role. For transgender individuals and others engaging in practices such as tucking, using alternatives like gaffs—which are designed to hold genital tissue without adhesive tape—can reduce skin irritation and help maintain proper hygiene. Healthcare providers who work with gender‐diverse populations are increasingly emphasizing the need for tailored advice to mitigate the risk of post-coital UTIs [3].
Many experts also advocate for the role of antibiotic prophylaxis in cases of recurrent UTIs after sex, though this approach must be used judiciously given the global concerns about antimicrobial resistance. In primary care settings, data extracted from electronic medical records have been successfully used to monitor antibiotic use and improve stewardship, thereby balancing the need for protection against infection with the risk of developing resistant strains [1]. Patients with frequent UTIs are encouraged to seek a personalized plan that may include low-dose, post-coital antibiotics, but such an approach must be monitored closely by a healthcare professional.
Treatment Options and Home Care for UTI After Sex
Despite best efforts at prevention, UTIs may still occur. At the first sign of symptoms, it is important to seek treatment promptly to prevent the infection from ascending into the kidneys. Standard treatment typically involves the use of antibiotics, with the choice of agent determined by local resistance patterns and patient-specific factors. For mild to moderate infections, a short course of antibiotics is often sufficient. It is critical to complete the full course of medication to ensure complete eradication of the bacteria, even if symptoms improve before the medication is finished.
Home care also plays an important role in the management of UTIs. In addition to antibiotics, patients are advised to take abundant fluids, avoid irritants such as caffeine or spicy foods, and apply heat to the pelvic area to alleviate discomfort. Some patients find relief by consuming foods or supplements that support urinary health, such as cranberry juice, although clinical evidence regarding its effectiveness remains mixed. Maintaining stress management and healthy sleep patterns may also support the body’s immune response and improve overall recovery.
For individuals who experience recurrent infections, some clinicians recommend a more thorough diagnostic evaluation. This may involve urine cultures to ascertain the specific bacteria responsible and determine the appropriate antibiotic sensitivity profile. In some cases, further imaging of the urinary tract may be warranted to rule out any anatomical abnormalities that predispose the patient to recurrent infections. Advances in electronic medical record data have made it easier for physicians to track these recurrent episodes and optimize treatment plans accordingly [1, 2].
Patients should also be aware of the importance of follow-up care. Even if symptoms subside with initial treatment, a follow-up urine culture is sometimes recommended to ensure that the infection has fully resolved. For many, persistent or recurrent symptoms may necessitate a change in the antibiotic regimen or the exploration of additional therapies, including non-antibiotic measures like probiotics or urinary alkalinizers.
When to Seek Medical Help for UTI After Sex
While many UTIs may be managed with prompt antibiotic therapy and home care, there are times when it is essential to seek professional medical help. If symptoms such as high fever, chills, severe back or abdominal pain, nausea, or vomiting develop, these may be signs that the infection has ascended to the kidneys, causing pyelonephritis, which is a medical emergency. In such cases, immediate consultation with a healthcare provider is recommended.
Additionally, if a person experiences frequent UTIs—especially if they recur despite following preventive strategies—it is important to undergo a thorough medical evaluation. Recurrent infections can lead to complications such as scarring of the kidneys and impaired kidney function over time. In these situations, a consultation with a urologist may be necessary to determine if there is an underlying abnormality or if a long-term preventive treatment plan is needed.
Furthermore, individuals with certain risk factors—such as pregnant women, immunocompromised patients, or those with urinary tract abnormalities—should not delay seeking medical attention at the onset of symptoms. A coordinated approach involving primary care physicians and specialists can help ensure that the infection is treated effectively while minimizing complications.
For those who are using post-coital prophylactic antibiotic regimens, it is still important to report any breakthrough symptoms to their healthcare provider. Regular monitoring through follow-up appointments and tests (such as urine cultures) is essential to avoid the development of antibiotic-resistant bacterial strains and ensure that any recurring infections are managed appropriately [1, 4].
Data Overview and Key Prevention Tactics
In clinical practice, data from multiple studies have underscored that early interventions and lifestyle modifications can substantially reduce UTI incidence. Below is an example table summarizing common risk factors and corresponding prevention tactics:
| Risk Factor | Explanation | Prevention Strategy |
|---|---|---|
| Short Female Urethra | A shorter urethra allows bacteria to more easily reach the bladder. | Urinate immediately after sex; maintain good perineal hygiene. |
| Post-Coital Urine Retention | Delaying urination after sex provides bacteria additional time to multiply in the urinary tract. | Make it a routine to empty the bladder soon after sexual activity. |
| Use of Irritating Contraceptives | Spermicides and diaphragms can disrupt the natural balance of vaginal flora, aiding bacterial colonization. | Consider alternative contraceptive methods; discuss options with a doctor. |
| Tucking and Related Practices | For transgender individuals using tucking, improper techniques can cause skin irritation and restrict normal voiding. | Use breathable, less irritating alternatives like gaffs; practice safe tucking techniques. |
| Prior History of Recurrent UTIs | Previous infections indicate a higher vulnerability to future UTIs. | Consult healthcare providers for potential prophylactic interventions and tailored treatment plans. |
This table highlights that prevention is multifaceted and must be adapted to individual circumstances. A comprehensive approach combining behavioral modifications, proper hygiene techniques, and, when appropriate, prophylactic measures offers the best protection against UTIs after sex.
Treatment Options: Medical and Self-Care Approaches
When prevention is insufficient, and symptoms set in, effective treatment becomes essential. The cornerstone of UTI treatment is the targeted use of antibiotics. Physicians typically prescribe a short course of antibiotics based on the severity of the infection and local resistance patterns. It is imperative that patients adhere to the prescribed dosage and duration even if they begin to feel better, as early discontinuation of treatment can lead to recurrence.
In parallel with antibiotic therapy, self-care measures can help mitigate discomfort and speed recovery. These include:
- Increased Fluid Intake: Drinking water helps dilute urine and promotes regular urination, which aids in flushing bacteria out.
- Application of Warm Compresses: A warm heating pad over the lower abdomen may reduce pain and muscle spasms.
- Avoidance of Irritants: Caffeine, alcohol, and spicy foods can irritate the bladder and exacerbate symptoms.
- Probiotic Supplementation: Probiotics may help restore the natural bacterial flora; however, patients should consult their physician before starting any supplement.
It is also important for patients diagnosed with a UTI to be proactive about follow-up care. Even if symptoms resolve, follow-up urine cultures can confirm that the infection has been completely eradicated. For patients who experience recurrent infections, additional diagnostic investigations—including imaging studies or referral to a specialist—might be necessary to identify and treat any underlying anatomical or physiological abnormalities.
When to Seek Medical Attention
Prompt medical evaluation can avert the progression of a simple bladder infection to a more serious kidney infection. Patients should seek medical attention if they encounter any of the following:
- High Fever or Chills: These symptoms may indicate that the infection has spread beyond the lower urinary tract.
- Severe Back or Flank Pain: Such pain can be a symptom of pyelonephritis, a potentially serious kidney infection.
- Persistent or Worsening Symptoms: If symptoms do not improve within a couple of days of starting treatment, it is time to seek further evaluation.
- Recurring UTIs: Frequent infections can lead to complications, such as kidney damage or scarring; consulting with a urologist is advisable.
- Special Populations: Pregnant women, elderly patients, immunocompromised individuals, and those with underlying urinary tract abnormalities should consult a healthcare provider even with mild symptoms.
Taking early action is critical, as delay in treatment can lead to more complicated infections that may require hospitalization and intravenous antibiotics. Healthcare providers may also adjust treatment regimens based on follow-up test results to reduce the risk of antibiotic resistance and other complications.
Managing UTIs in Special Populations
Certain groups require extra vigilance. For example, transgender individuals who experience UTIs due to practices like tucking need specialized advice on modifying techniques and maintaining hygiene. Additionally, postmenopausal women face hormonal changes that can alter natural flora and make urinary tracts more vulnerable; topical estrogen therapy under medical supervision might be beneficial in such cases.
Patients with recurrent UTIs should obtain periodic assessments that may include urine cultures, blood tests, and imaging studies. These evaluations help determine whether additional prophylactic measures like low-dose post-coital antibiotics are needed. Furthermore, integrating data analysis from electronic medical records enables clinicians to detect patterns in antibiotic use and UTI occurrence, thereby refining individualized treatment protocols [1, 2].
The Role of Technology in UTI Prevention and Management
Advances in digital health have spearheaded the development of better prevention strategies. Primary care systems are increasingly relying on electronic health records (EHRs) to track antibiotic prescribing and monitor treatment outcomes. By analyzing vast datasets, clinicians can identify trends and implement antimicrobial stewardship programs aimed at reducing unnecessary antibiotic use—a practice that ultimately lowers the risk of resistant infections. These data-driven approaches are essential in tailoring treatment plans and preventive strategies for patients prone to UTIs after sex.
Adopting smart technology can help individuals manage their own health as well. Mobile applications and wearable devices can remind patients to hydrate frequently, log daily voiding patterns, and track symptoms real time. While the integration of such tools is still evolving, their potential to empower patients in maintaining urinary health is significant. In the future, such tools may provide precise, personalized recommendations that further reduce the risk of UTIs.
Conclusion
UTIs after sex may seem like a minor inconvenience, but their impact on quality of life can be profound. Fortunately, there are a host of effective prevention tactics and treatment options available. By understanding the risk factors—including anatomical predispositions, post-coital behaviors, and specific sexual practices—and by adopting simple yet effective measures such as immediate post-sex urination and proper hygiene, individuals can dramatically lower their UTI risk. Furthermore, healthcare providers can play a critical role by prescribing appropriate treatments and monitoring patients using modern digital tools and data analysis.
Whether it is through improved personal habits, timely medical interventions, or innovative technological support, gaining control over UTIs after sex is achievable. The key is to maintain a proactive, informed, and individualized approach to urinary health so that when symptoms appear, relief is swift and complications are minimized. Remember that your wellbeing is paramount and that seeking professional help when experiencing persistent or severe symptoms is a crucial part of self-care.
Frequently Asked Questions (FAQ)
What makes UTIs more common after sex?
Sexual intercourse can allow bacteria present around the genital or anal area to migrate into the urinary tract. The combination of friction, the short female urethra, and delayed urination after sex increases the likelihood that bacteria can colonize the bladder, leading to infection [7].
Are there lifestyle modifications that can reduce the risk of UTIs after sex?
Yes, several modifications can help. Urinating immediately after sex, practicing good perineal hygiene, staying well hydrated, and potentially using probiotic supplements are all effective measures. Avoiding irritating contraceptives (like spermicides) and adjusting sexual techniques, particularly for individuals who practice tucking, can also reduce risk [3, 7].
When should I see a doctor for a suspected UTI after sex?
If you experience severe symptoms such as high fever, chills, or significant pelvic or back pain, or if your symptoms persist for more than two days despite self-care measures, you should consult a healthcare provider immediately. Frequent or recurrent UTIs also warrant a medical evaluation to rule out any underlying issues [1, 4].
What treatment options are available if I get a UTI after sex?
UTIs are typically treated with a short course of antibiotics. It is crucial to complete the full course even if symptoms improve early. In addition to medication, increasing fluid intake, applying heat, and avoiding urinary irritants can help alleviate discomfort. In cases of recurring infections, your doctor might also consider a tailored prophylactic treatment plan [1, 2].
Can technology help prevent or manage UTIs?
Absolutely. Advances in digital health, such as electronic medical records, mobile health apps, and wearable devices, are increasingly used to monitor symptoms and optimize treatment. These technologies also support antimicrobial stewardship by tracking antibiotic prescriptions and ensuring that patients receive appropriate care, thus reducing the overall risk of complications [1, 6].
References
-
Cheah, R., Chen, C. B., Capurro, D., Manski-Nankervis, J., Rozova, V., Thursky, K., … (2024). A systematic review on how primary care electronic medical record data have been used for antimicrobial stewardship. Antimicrobial Stewardship & Healthcare Epidemiology. Retrieved from https://doi.org/10.1017/ash.2024.499
-
Chen, C. B., et al. (n.d.). How do surgical interventions for neurogenic lower urinary tract dysfunction impact quality of life? Retrieved from https://pubmed.ncbi.nlm.nih.gov/11788944/
-
Phillippi, J. C. (2024). Acute cystitis in a transfeminine patient: Assessment and treatment of urinary tract symptoms. Journal of Midwifery & Women’s Health. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11803489/
-
(n.d.). Pharmacological treatment of pregnancy complications in adults: An overview of phase IV clinical trials. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11789866/
-
(2024). A profile of children with traumatic brain injury admitted to the paediatric intensive care unit of Red Cross War Memorial Children’s Hospital in Cape Town, South Africa, between 2015 and 2019. Retrieved from https://doi.org/10.7196/SAJCC.2024.v40i3.2212
-
Chae, M., et al. (2022). Chronic circadian disruption on a high‐fat diet impairs glucose tolerance. Retrieved from https://doi.org/10.1016/j.metabol.2022.155158
-
Amiri, F., & Safiri, S. (2025). Epidemiology of urinary tract infections in the Middle East and North Africa, 1990–2021. Tropical Medicine and Health. Retrieved from https://doi.org/10.1186/s41182-025-00692-x
-
Samaheen, M., Mohammad, M., Salzmann, M., Ramadanov, N., & others. (2024). The health‐related quality of life for cemented versus uncemented hemiarthroplasty in elderly patients with femoral neck fractures: A systematic review and meta‐analysis of randomized controlled trials. Orthopaedic Surgery. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11787973/
By following these proven tactics, and understanding both the causes and risk factors, you can significantly reduce the occurrence of UTIs after sex and regain relief swiftly should an infection occur. Remember to practice preventive self-care, remain informed about your personal risk factors, and always consult with your healthcare provider if symptoms worsen or persist.