Table of Contents
Signs and Symptoms of Protein in Urine During Pregnancy
Expecting mothers may not always exhibit obvious symptoms of proteinuria. However, there are certain signs that may indicate its presence. Common symptoms include:
- Swelling or Edema: This often occurs in the hands, feet, and face. While some swelling can be normal during pregnancy, sudden or severe swelling may be a cause for concern.
- High Blood Pressure: Pregnancy-induced hypertension may accompany proteinuria, leading to further complications.
- Sudden Weight Gain: Rapid weight gain over a short period can signal fluid retention, which may be linked to proteinuria.
- Headaches and Vision Changes: Severe headaches or changes in vision, such as blurriness or seeing spots, can indicate serious conditions like preeclampsia, which is associated with proteinuria.
These symptoms should prompt immediate medical evaluation to ensure both maternal and fetal health.
Common Causes of Proteinuria in Expecting Mothers
Proteinuria can arise from several causes during pregnancy. The most common include:
- Gestational Hypertension and Preeclampsia: These are conditions characterized by high blood pressure and proteinuria. Preeclampsia can lead to serious complications if not monitored and managed appropriately (Simancas-Racines et al., 2023).
- Urinary Tract Infections (UTIs): UTIs can lead to proteinuria. Pregnant women are more susceptible to UTIs due to hormonal changes and pressure on the bladder (Bryliński et al., 2023).
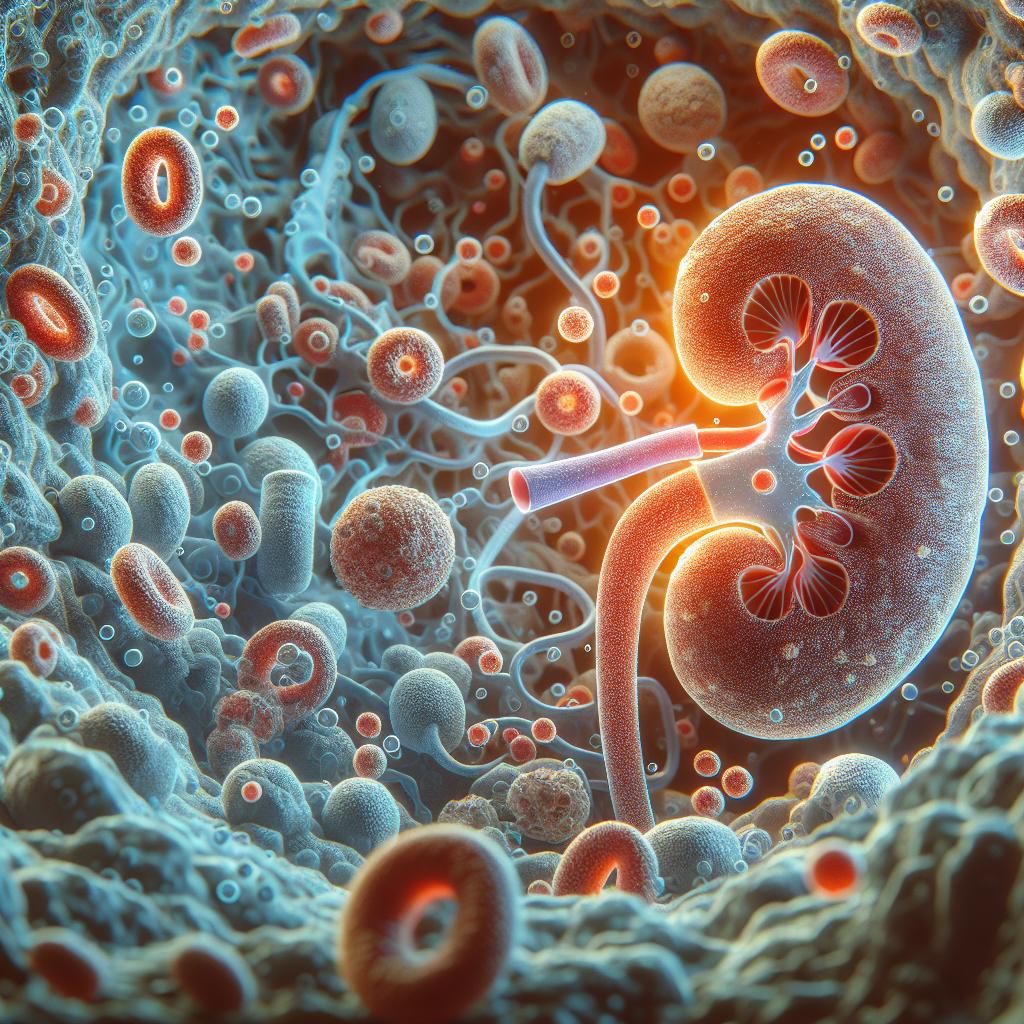
- Kidney Disease: Pre-existing kidney conditions can exacerbate during pregnancy, resulting in increased protein levels in urine.
- Diabetes: Pregnant women with pre-existing diabetes or gestational diabetes may experience proteinuria as a complication of their condition.
Recognizing these causes is crucial for timely intervention and management.
Risks Associated with Protein in Urine During Pregnancy
The presence of protein in urine during pregnancy poses several risks, primarily:
- Preeclampsia: This serious condition can lead to complications such as placental abruption, preterm labor, and even maternal and fetal mortality if left untreated (Simancas-Racines et al., 2023).
- Premature Birth: Proteinuria is associated with an increased risk of premature delivery, which can lead to complications for the newborn.
- Low Birth Weight: Infants born to mothers with untreated proteinuria may experience intrauterine growth restriction, leading to low birth weight and associated health issues.
- Kidney Damage: Severe proteinuria can indicate underlying kidney problems, necessitating further evaluation and treatment.
Understanding these risks is vital for both healthcare providers and expectant mothers to ensure proactive management.
Diagnostic Tests for Proteinuria in Pregnant Individuals
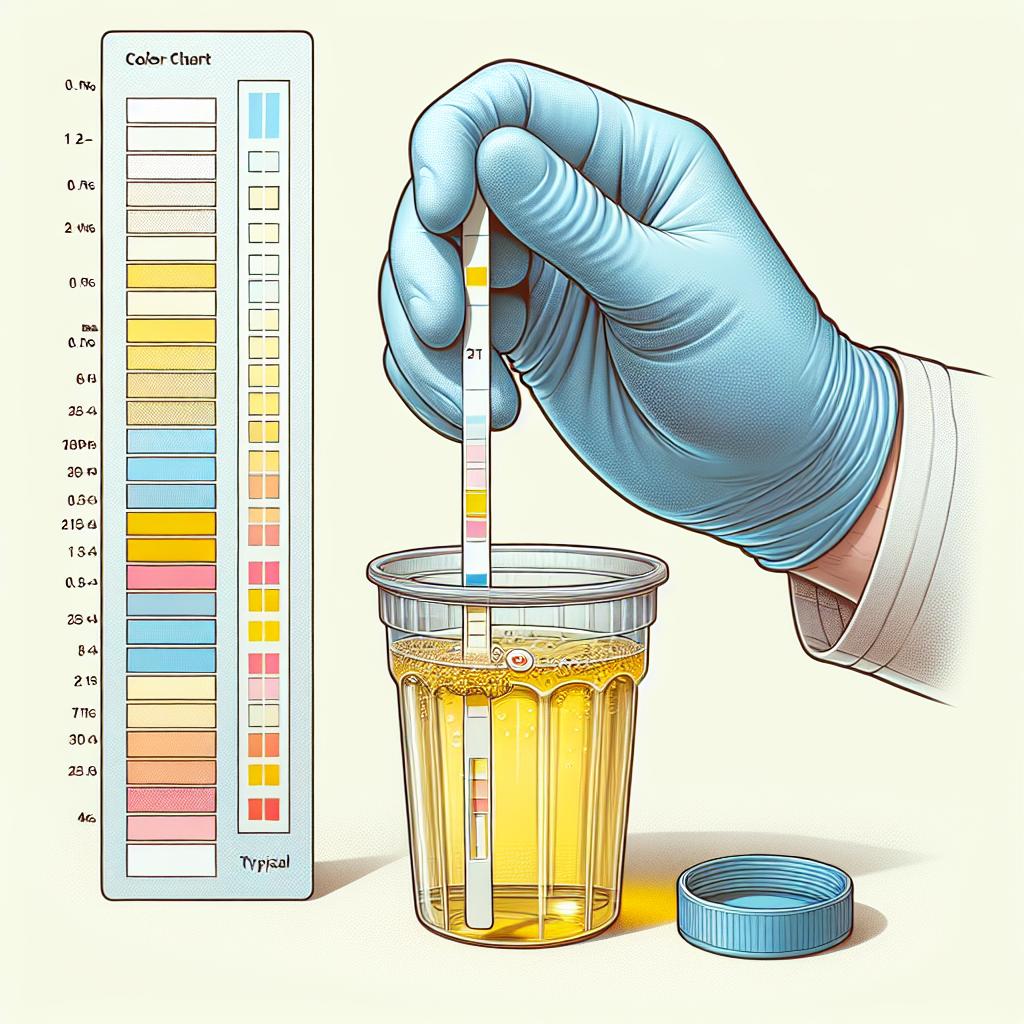
Diagnosing proteinuria typically involves several tests:
- Urine Dipstick Test: This is a quick screening tool performed during routine prenatal visits. A positive result indicates further testing is needed.
- 24-hour Urine Collection: This test quantifies protein levels in the urine over a 24-hour period, providing a more accurate assessment of proteinuria.
- Blood Tests: Monitoring liver function and kidney function tests can help determine if the proteinuria is related to other serious conditions, such as preeclampsia.
- Ultrasound: In some cases, an ultrasound may be performed to assess the health of the fetus and the placenta, especially if proteinuria is associated with hypertension.
Early detection through these diagnostic tools is essential for managing potential complications effectively.
Management and Treatment Options for Proteinuria in Pregnancy
Management of proteinuria during pregnancy focuses on addressing the underlying causes and mitigating risks. Common strategies include:
- Monitoring: Regular monitoring of blood pressure and urine protein levels is essential to track the progression of any underlying conditions.
- Lifestyle Modifications: Dietary changes, such as reducing salt intake and increasing fluid consumption, may help manage symptoms and improve health outcomes.
- Medications: Depending on the severity of proteinuria and associated conditions, medications such as antihypertensives or corticosteroids may be prescribed.
- Delivery Planning: In cases of severe preeclampsia or other serious complications, early delivery may be necessary to protect the health of both the mother and the baby.
Table 1: Summary of Management Strategies for Proteinuria
| Strategy | Description |
|---|---|
| Monitoring | Regular assessments of blood pressure and urine protein levels |
| Lifestyle Modifications | Dietary changes, such as reduced salt intake |
| Medications | Use of antihypertensives or corticosteroids |
| Delivery Planning | Consideration of early delivery in severe cases |
Effective management of proteinuria during pregnancy can significantly reduce risks and improve outcomes for both mother and child.
FAQ
What should I do if I have protein in my urine during pregnancy?
If you have been diagnosed with proteinuria, it’s essential to consult your healthcare provider for further evaluation and management.
Is proteinuria common in pregnancy?
While some protein in urine can be normal, significant proteinuria may indicate underlying health issues that need to be addressed.
How is proteinuria treated during pregnancy?
Treatment focuses on monitoring your condition, lifestyle modifications, and possibly medication, depending on the severity and underlying causes.
Can proteinuria affect my baby?
Yes, untreated proteinuria can lead to complications such as low birth weight and premature birth, necessitating careful monitoring and management.
Are there any lifestyle changes I can make to help with proteinuria?
Maintaining a balanced diet, staying hydrated, and managing blood pressure can help in managing protein levels in urine during pregnancy.
References
-
Simancas-Racines, D., Frias-Toral, E., Campuzano-Donoso, M., Ramos-Sarmiento, D., Zambrano-Villacres, R., Reytor-González, C., & Schiavo, L. (2023). Preoperative Nutrition in Bariatric Surgery: A Narrative Review on Enhancing Surgical Success and Patient Outcomes. Nutrients, 17(3), 566. https://doi.org/10.3390/nu17030566
-
Bryliński, Ł., Kostelecka, K., Woliński, F., Komar, O., Miłosz, A., Michalczyk, J., Biłogras, J., & Schomburg, L. (2023). Effects of Trace Elements on Endocrine Function and Pathogenesis of Thyroid Diseases—A Literature Review. Nutrients, 17(3), 398. https://doi.org/10.3390/nu17030398
-
Simancas-Racines, D., Frias-Toral, E., Campuzano-Donoso, M., Ramos-Sarmiento, D., Zambrano-Villacres, R., Reytor-González, C., & Schiavo, L. (2023). Impact of Different Low-Volume Concurrent Training Regimens on Cardiometabolic Health, Inflammation, and Fitness in Obese Metabolic Syndrome Patients. Nutrients, 17(3), 561. https://doi.org/10.3390/nu17030561
-
Ceballos-Rasgado, M., Brazier, A. K. M., Gupta, S., Moran, V. H., Pierella, E., Fekete, K., & Lowe, N. M. (2024). Methods of Assessment of Zinc Status in Humans: An Updated Review and Meta-analysis. Nutrition Reviews
-
Nenad Blau et al. (2023). Genotype–Phenotype Correlation in a Large Cohort of Eastern Sicilian Patients Affected by Phenylketonuria: Newborn Screening Program, Clinical Features, and Follow-Up. Nutrients, 17(3), 379. https://doi.org/10.3390/nu17030379
-
Werts, S. et al. (2023). Feeding behaviors in children with Fetal Alcohol Spectrum Disorder. Journal of Pediatric Health Care.
-
Hay, S. et al. (2023). Vitamin B12 intake and serum cobalamin levels in pediatric populations. Journal of Nutrition.