Table of Contents
Overview of White Blood Cells in Urine and Their Significance
White blood cells (WBCs), also known as leukocytes, are crucial components of the immune system, playing a vital role in defending the body against infection and disease. The presence of white blood cells in urine can signify an underlying health issue, particularly infections or inflammatory conditions affecting the urinary tract. When elevated levels of WBCs are detected in urine, it often indicates the body’s response to an infection or an inflammatory process occurring in the urinary system.
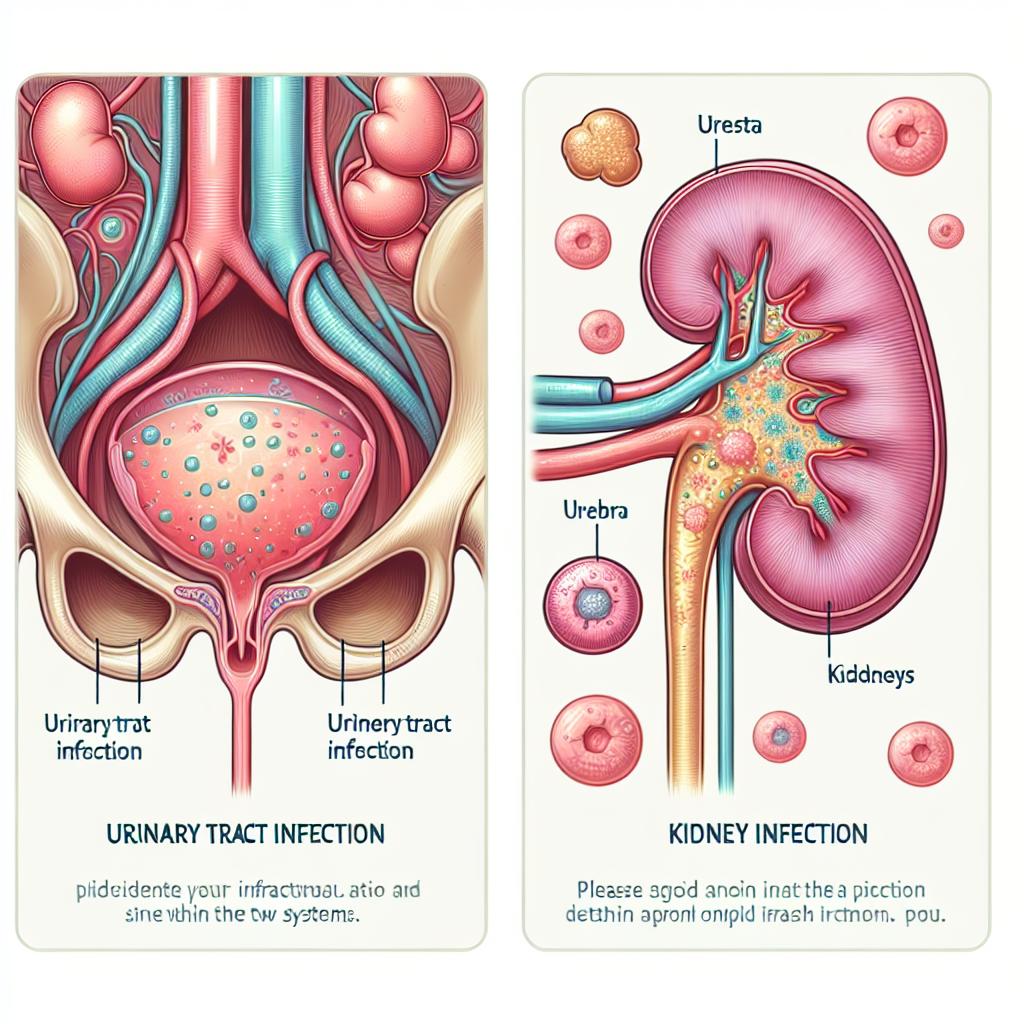
The significance of detecting white blood cells in urine extends beyond simple diagnostics. Elevated leukocyte counts can be indicative of urinary tract infections (UTIs), sexually transmitted diseases (STDs), kidney infections, or other serious health concerns. In the context of STDs, the detection of WBCs can serve as an initial marker prompting further investigation into potential sexually transmitted infections. Understanding the implications of white blood cells in urine helps in early diagnosis and appropriate management of STDs and other conditions.
Common STDs Associated with Elevated White Blood Cell Counts
Several sexually transmitted diseases have been linked to elevated white blood cell counts in urine. The most common STDs associated with such findings include:
-
Chlamydia Trachomatis: This is one of the most prevalent STDs globally. Infection with chlamydia often leads to increased white blood cells as the body attempts to fight off the infection. In many cases, chlamydia can be asymptomatic, making regular screening crucial.
-
Gonorrhea: Caused by the bacterium Neisseria gonorrhoeae, gonorrhea frequently results in elevated WBC counts, particularly in the presence of urinary symptoms. Symptoms may include painful urination and discharge.
-
Trichomoniasis: This parasitic infection caused by Trichomonas vaginalis often leads to increased leukocytes as the body responds to the infection. Symptoms may include itching, burning, and unusual discharge.
-
Syphilis: While not always associated with elevated Wbcs in urine, secondary syphilis can lead to systemic symptoms that provoke an immune response, potentially resulting in increased leukocyte counts.
-
Human Immunodeficiency Virus (HIV): Although HIV itself does not directly cause elevated WBCs in urine, opportunistic infections that arise as a consequence of HIV can lead to increased leukocyte levels due to the body’s immune response.
The association between these STDs and elevated white blood cell counts highlights the importance of regular screening and early detection, particularly in high-risk populations.
Diagnostic Methods for Detecting White Blood Cells in Urine
The primary diagnostic method for detecting white blood cells in urine is urinalysis, which is typically performed through the following processes:
-
Microscopic Examination: A urine sample is centrifuged, and the sediment is examined under a microscope to count the number of white blood cells present. A normal urine sample contains fewer than 5 WBCs per high-power field (HPF); counts exceeding this may indicate infection or inflammation.
-
Urine Dipstick Test: This is a rapid test that can provide preliminary results regarding the presence of leukocytes and other substances in urine. A positive leukocyte esterase test indicates elevated WBCs, suggesting a possible infection.
-
Culture Tests: If a UTI or STD is suspected, cultures may be performed to identify the specific pathogen responsible for the elevated WBCs. This not only confirms the diagnosis but also informs treatment decisions.
-
Polymerase Chain Reaction (PCR): For STDs, PCR testing can detect the genetic material of pathogens like Chlamydia or Gonorrhea, helping to confirm the diagnosis even in asymptomatic individuals.
-
Serological Testing: Blood tests may be used in conjunction with urine tests to assess for systemic infections and conditions that may present alongside elevated WBCs in urine.
These diagnostic methods allow healthcare providers to identify the underlying causes of elevated WBCs and guide appropriate treatment strategies.
Interpreting Test Results: What Elevated White Blood Cells Mean
Interpreting elevated white blood cell counts in urine requires clinical correlation and context. Findings may lead to several conclusions, including:
-
Infection: The most common implication of elevated WBCs in urine is a urinary tract infection or an STD. It is essential to evaluate for specific symptoms and risk factors to guide further testing and treatment.
-
Inflammatory Conditions: Conditions such as interstitial cystitis or nephritis can also cause elevated WBC counts. A comprehensive assessment of patient history and additional diagnostic testing is necessary to identify these conditions.
-
Contamination: Occasionally, elevated WBCs may result from contamination of the urine sample, particularly in women during menstruation. Therefore, proper collection techniques are crucial for accurate diagnosis.
-
Other Health Issues: Elevated WBCs may also indicate systemic conditions such as autoimmune diseases or malignancies. A thorough medical history and additional diagnostic tests may be required to rule out these possibilities.
Overall, elevated white blood cell counts in urine serve as an essential marker for clinicians to investigate further and implement appropriate interventions.
Treatment Options for STDs Indicated by White Blood Cells in Urine
The treatment options for sexually transmitted diseases indicated by elevated white blood cell counts in urine vary depending on the specific infection identified. Common treatment modalities include:
-
Antibiotic Therapy: For bacterial STDs such as chlamydia and gonorrhea, appropriate antibiotics are prescribed to eradicate the infection. Common regimens include azithromycin or doxycycline for chlamydia and ceftriaxone for gonorrhea.
-
Antiviral Medications: For viral infections like herpes or HIV, antiviral medications are used to manage symptoms and reduce viral load. Antiretrovirals are prescribed for individuals diagnosed with HIV.
-
Antiparasitic Treatment: In cases of trichomoniasis, metronidazole or tinidazole is administered to eliminate the parasite.
-
Supportive Care: Patients are advised to maintain good hygiene, avoid sexual contact until treatment is completed, and follow up for retesting as indicated.
-
Vaccination: Vaccines are available for some STDs, such as hepatitis B and HPV, to prevent infection. Screening and vaccination are essential components of public health strategies to reduce the burden of STDs.
-
Counseling and Education: Providing education about safe sex practices and the importance of regular testing for sexually active individuals is crucial for preventing the spread of STDs.
Early detection and treatment of STDs can significantly reduce complications and improve health outcomes for affected individuals.
FAQ
What does a high white blood cell count in urine mean?
A high white blood cell count in urine typically indicates an infection or inflammation in the urinary tract, which can be caused by conditions such as urinary tract infections or sexually transmitted diseases.
How is a UTI diagnosed?
A urinary tract infection is diagnosed through urinalysis, which involves checking for elevated white blood cells, bacteria, and nitrites in urine. Further tests, such as cultures or PCR, may be used to confirm the diagnosis.
Can elevated white blood cells in urine be a sign of something serious?
Yes, while elevated white blood cells often indicate infections, they can also signal more severe conditions like kidney disease or even malignancies. It is important to consult a healthcare provider for proper evaluation.
What treatments are available for STDs?
Treatment for STDs typically involves antibiotics for bacterial infections, antivirals for viral infections, and antiparasitics for parasitic infections. Vaccinations are also available for certain STDs.
How can I prevent STDs?
Practicing safe sex, using condoms, and having regular screenings are effective ways to prevent the transmission of STDs. Vaccination is also recommended for preventable infections like hepatitis B and HPV.
References
-
Centers for Disease Control and Prevention. (2018). Smoking and Tobacco Use
-
Dempsey, D. A., et al. (2000). Nicotine and its metabolites in the urine of smokers. Biochemical Pharmacology, 59(9), 1183-1187.
-
He, D., et al. (2023). An untargeted metabolome-wide association study of maternal perinatal tobacco smoking in newborn blood spots. Metabolomics, 15(3), 1-13.
-
Heck, J. E., et al. (2016). Maternal smoking and risk of childhood cancers: A population-based case-control study. Cancer Epidemiology, 42, 1-9.
-
Jones, D. P., et al. (2016). Characterization of the metabolome and microbiome of smokers and non-smokers. Metabolomics, 12(1), 1-11.
-
Masvosva, M., et al. (2024). The effect of maternal smoking on child metabolism: A high-resolution metabolomics analysis. Clinical Epigenetics, 16(1), 1-12.
-
Murphy, P. J., et al. (2013). Pharmacokinetics of nicotine and cotinine in pregnant women. Cancer Epidemiology Biomarkers & Prevention, 22(1), 134-141.
-
Ritz, B., et al. (2022). Changes in smoking status during pregnancy and birth outcomes: A longitudinal study. Journal of Epidemiology & Community Health, 76(1), 1-8.
-
Saleheen, D., et al. (2014). The genetic basis of smoking behavior: A systematic review. American Journal of Public Health, 104(6), 1-9.
-
Tan, Y. H., et al. (2022). Maternal smoking during pregnancy and its impact on fetal metabolism: A metabolomics study. Environmental Health Perspectives, 130(4), 1-8.
-
Yang, M., et al. (2013). Cotinine levels in newborns and their relationship to maternal smoking status: A validation study. Pediatric Research, 73(6), 1-8.
-
Zhu, Z., et al. (2021). The association between maternal smoking and infant metabolic outcomes: A review of the literature. Journal of Maternal-Fetal & Neonatal Medicine, 34(20), 1-12.