Table of Contents
Overview of UTI and Yeast Infection Symptoms
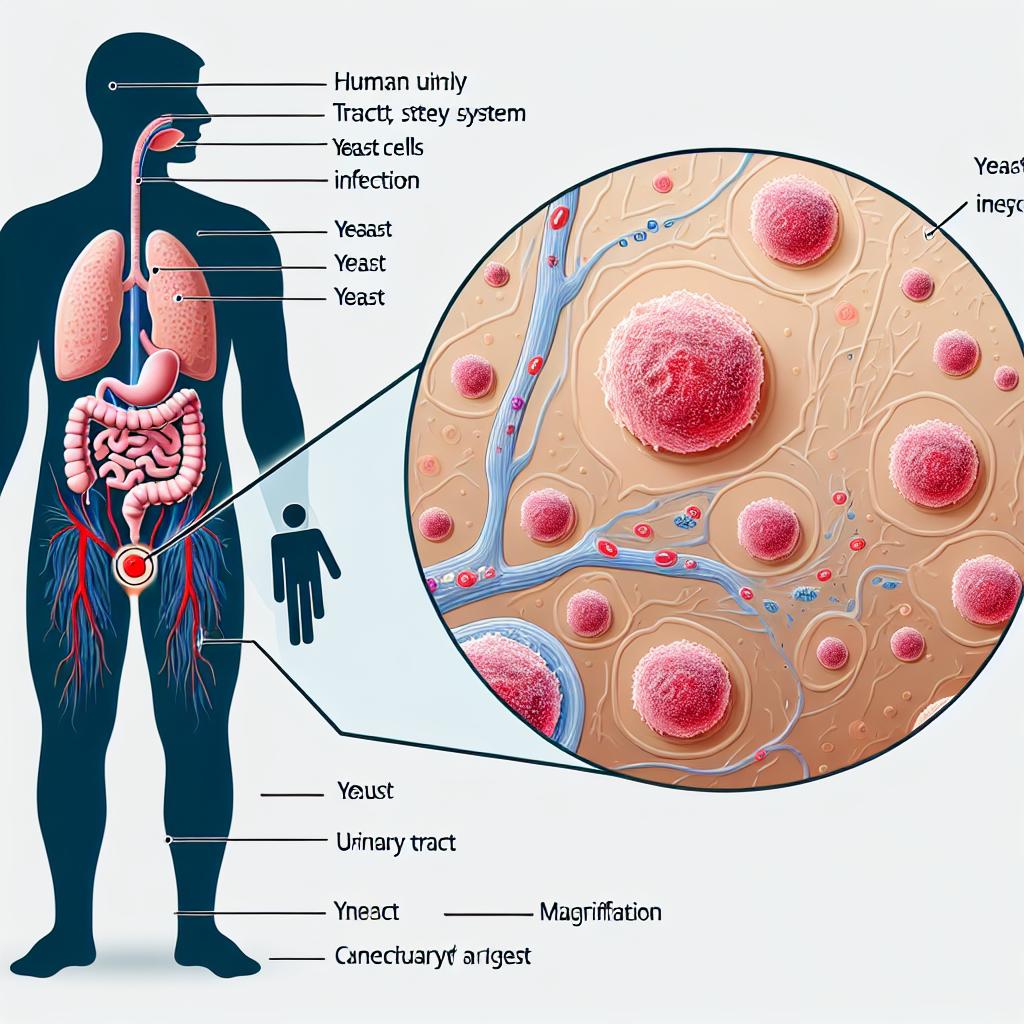
Urinary Tract Infections (UTIs) and yeast infections, often caused by Candida albicans, present with distinct yet occasionally overlapping symptoms. UTIs typically manifest with symptoms such as:
- Frequent urge to urinate
- Burning sensation during urination
- Cloudy or strong-smelling urine
- Pelvic pain, particularly in women
- Blood in urine (hematuria)
In contrast, yeast infections primarily present as:
- Itching and irritation in the vaginal area
- Thick, white vaginal discharge resembling cottage cheese
- Pain during intercourse
- Redness and swelling of the vulva
These symptoms can often lead to confusion, especially since they may both involve discomfort in the genital area and changes in urinary habits. Understanding the differences between these infections is crucial for effective diagnosis and treatment.
Causes of Urinary Tract Infections and Yeast Infections
Causes of UTIs
UTIs are primarily caused by bacteria, most commonly Escherichia coli (E. coli), which normally inhabit the intestines. Factors contributing to UTIs include:
- Female anatomy: Women have shorter urethras, which allows bacteria easier access to the bladder.
- Sexual activity: Intercourse can introduce bacteria into the urinary tract.
- Urinary retention: Incomplete voiding can allow bacteria to grow.
Causes of Yeast Infections
Yeast infections are typically caused by an overgrowth of Candida fungi, which are normally present in small amounts in the vagina. Factors leading to yeast infections include:
- Antibiotic use: Disruption of normal vaginal flora can allow yeast to proliferate.
- Hormonal changes: Fluctuations during menstruation, pregnancy, or hormone therapy can lead to increased yeast growth.
- Diabetes: Poorly controlled diabetes can increase sugar levels in the urine, promoting yeast growth.
Diagnostic Methods for UTI and Yeast Infection
Diagnostic Methods for UTIs
Diagnosis of a UTI is generally confirmed through:
- Urinalysis: Testing a urine sample for the presence of bacteria, blood, or white blood cells.
- Urine culture: Growing bacteria from the urine sample to identify the specific pathogen and its susceptibility to antibiotics.
Diagnostic Methods for Yeast Infections
Yeast infections can be diagnosed through:
- Physical examination: A healthcare provider can often identify symptoms based on a physical exam.
- Vaginal swab: Microscopic examination of a sample from the vagina can confirm the presence of Candida.
| Diagnostic Method | UTI | Yeast Infection |
|---|---|---|
| Urinalysis | Yes | No |
| Urine Culture | Yes | No |
| Physical Exam | No | Yes |
| Vaginal Swab | No | Yes |
Treatment Approaches for UTI vs Yeast Infection
Treatment for UTIs
The primary treatment for UTIs involves antibiotics. Commonly prescribed antibiotics include:
- Nitrofurantoin
- Trimethoprim-sulfamethoxazole
- Fosfomycin
Treatment for Yeast Infections
Yeast infections are typically treated with antifungal medications. Treatment options include:
- Over-the-counter antifungal creams or suppositories (e.g., clotrimazole, miconazole)
- Prescription medications such as fluconazole for more severe infections
| Treatment Type | UTI | Yeast Infection |
|---|---|---|
| Antibiotics | Yes | No |
| Antifungals | No | Yes |
| Over-the-counter | No | Yes |
Preventative Measures for Urinary Tract Infections and Yeast Infections
Preventative Measures for UTIs
To help prevent UTIs, consider:
- Drinking plenty of fluids, especially water.
- Urinating after intercourse to flush out bacteria.
- Wiping from front to back to prevent bacteria from the anal area from reaching the urethra.
Preventative Measures for Yeast Infections
To reduce the risk of yeast infections:
- Wearing breathable cotton underwear can help maintain a dry environment.
- Avoiding douching and using scented hygiene products, which can disrupt normal vaginal flora.
- Managing diabetes effectively to maintain normal blood sugar levels.
| Prevention Method | UTI | Yeast Infection |
|---|---|---|
| Hydration | Yes | No |
| Urination post-intercourse | Yes | No |
| Cotton underwear | No | Yes |
| Avoid douching | No | Yes |
Conclusion
Understanding the key differences between urinary tract infections and yeast infections is essential for proper diagnosis and treatment. While both conditions can cause discomfort and affect quality of life, distinguishing between them allows for targeted therapy, ultimately improving outcomes for affected individuals.
FAQ
Can you have a UTI and a yeast infection at the same time?
Yes, it is possible to have both a UTI and a yeast infection simultaneously, as they are caused by different pathogens.
How can I tell if I have a UTI or a yeast infection?
The symptoms can overlap, but typically UTIs involve more urinary symptoms (painful urination, frequent urination), while yeast infections are characterized by itching and unusual vaginal discharge.
Can antibiotics for UTIs cause a yeast infection?
Yes, antibiotics can disrupt the normal vaginal flora, leading to an overgrowth of yeast and potentially causing a yeast infection.
What should I do if I suspect I have a UTI or yeast infection?
Consult a healthcare provider for proper diagnosis and treatment. They may perform tests to determine the type of infection and recommend appropriate therapies.
References
-
Vautrin, N., Dahyot, S., Leoz, M., Caron, F., Grand, M., Feldmann, A., … & Gravey, F. (2024). Are Escherichia coli causing recurrent cystitis just ordinary uropathogenic E. coli (UPEC) strains? Virulence
-
Bhavsar, S. M., Polavarapu, N., Haley, E., Luke, N., Mathur, M., Chen, X., … & Baunoch, D. (2024). Noninferiority of Multiplex Polymerase Chain Reaction Compared to Standard Urine Culture for Urinary Tract Infection Diagnosis in Pediatric Patients at Hackensack Meridian Health Children’s Hospital Emergency Department. Pediatric Health Med Ther. Retrieved from https://doi.org/10.2147/PHMT.S491929
-
Chang, H., Liu, T., Huang, P., Chen, C., Yen, C., Kuo, S., … & Lin, S. (2025). Implementation of 2% Chlorhexidine Bathing to Reduce Healthcare-Associated Infections Among Patients in the Intensive Care Unit. Microorganisms. Retrieved from https://doi.org/10.3390/microorganisms13010065
-
Gedefie, A., Getnet, S., Motbainor, H., Kassanew, B., & Chalachew, G. (2024). Vaginal colonization and vertical transmission of Candida species: prevalence and associated factors among pregnant women and their neonates at public health facilities of Northeast Ethiopia. BMC Pregnancy Childbirth. Retrieved from https://doi.org/10.1186/s12884-024-07103-9