Table of Contents
Physiological Causes
Physiological proteinuria can occur due to the increased glomerular filtration rate (GFR) that is characteristic of pregnancy. The kidneys adapt to the increased metabolic demands of the mother and fetus, which may temporarily elevate protein levels in the urine. This is generally considered benign and resolves after delivery.
Pathological Causes
-
Preeclampsia: One of the most serious conditions associated with proteinuria, preeclampsia is characterized by hypertension and proteinuria after the 20th week of gestation. The condition can lead to severe complications for both mother and child if not managed appropriately (Jiang et al., 2022).
-
Gestational Diabetes Mellitus (GDM): GDM is another common condition during pregnancy, with studies suggesting a correlation between elevated protein levels and the incidence of this metabolic disorder (He et al., 2019).
-
Urinary Tract Infections (UTIs): UTIs are prevalent in pregnant women and can result in proteinuria. They require prompt diagnosis and treatment to prevent complications (McIntyre et al., 2019).
-
Chronic Kidney Disease (CKD): Women with pre-existing kidney conditions may experience exacerbation during pregnancy, leading to proteinuria. This necessitates close monitoring and potential intervention (Ostermann et al., 2020).
-
Other Conditions: Conditions like lupus or hypertension can also lead to proteinuria during pregnancy. Women with such pre-existing conditions need careful monitoring throughout their pregnancy (McIntyre et al., 2019).
Health Risks Associated with Protein in Urine
Proteinuria can be a sign of serious health issues that pose risks to both the mother and the fetus.
Risks of Preeclampsia
Preeclampsia poses significant risks such as:
- Maternal and fetal morbidity: Severe cases can lead to maternal seizures (eclampsia) and fetal growth restrictions (Chen et al., 2025).
- Long-term health consequences: Women who experience preeclampsia may have an increased risk of cardiovascular disease later in life (Lee et al., 2018).
Risks of Gestational Diabetes
- Immediate maternal health risks: Increased likelihood of hypertensive disorders and potential complications during delivery.
- Long-term risks for the child: Increased risk of obesity and type 2 diabetes later in life (Jiang et al., 2022).
Infections and Other Complications
Persistent proteinuria may indicate underlying infections or other health issues, leading to hospitalization or more invasive treatments (McIntyre et al., 2019).
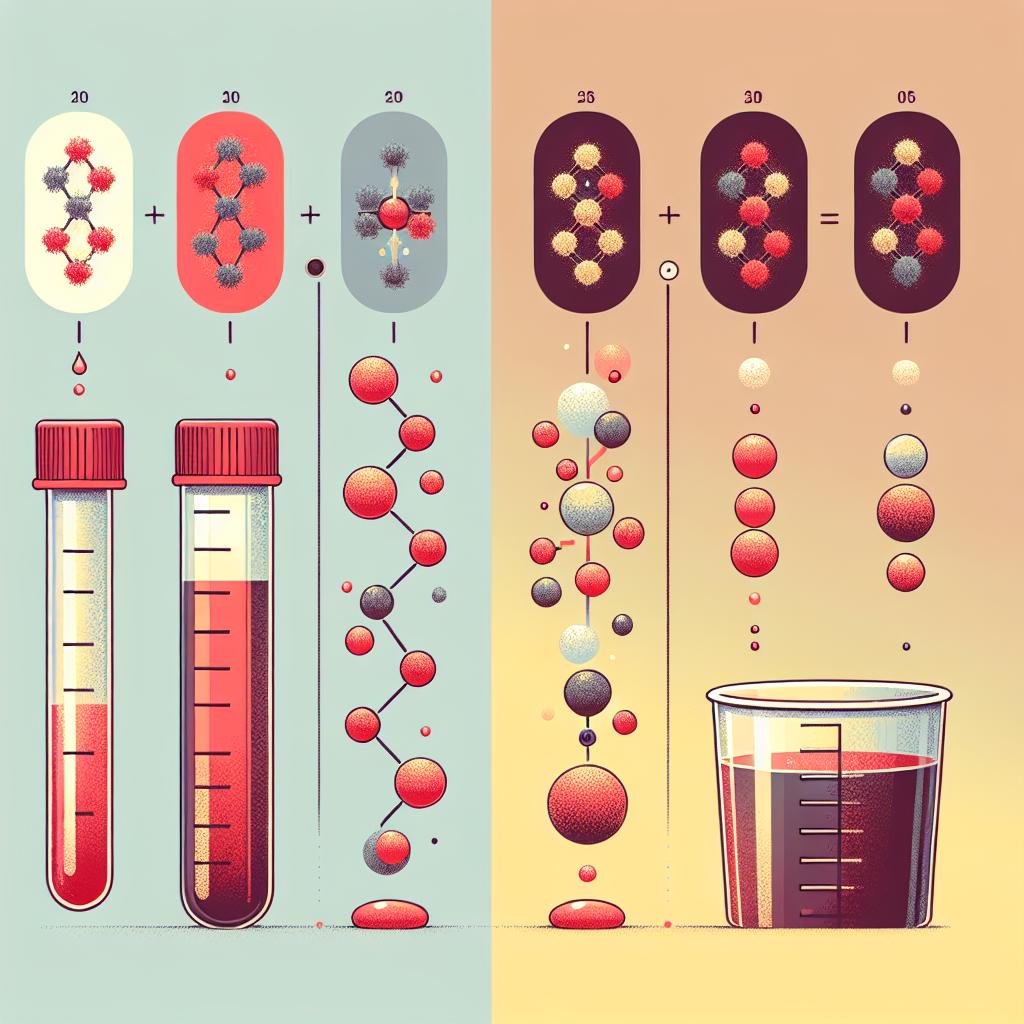
Diagnostic Tests for Proteinuria During Pregnancy
Accurate diagnosis of proteinuria in pregnancy involves several steps:
-
Urine Dipstick Test: This is a quick test performed during routine prenatal visits. A positive result on the dipstick indicates the presence of protein and warrants further investigation (Chen et al., 2025).
-
24-Hour Urine Collection: This is the gold standard for quantifying proteinuria. It involves collecting all urine produced in a 24-hour period to measure the total protein excretion (Jiang et al., 2022).
-
Serological Tests: These tests may be performed to assess for conditions such as GDM or preeclampsia. They include blood pressure measurements, serum creatinine, and liver function tests (McIntyre et al., 2019).
-
Ultrasound: In cases of suspected kidney disease or complications related to preeclampsia, ultrasound imaging may be used to evaluate kidney structure and function (Ostermann et al., 2020).
Table 1: Common Diagnostic Tests for Proteinuria
| Test Type | Purpose |
|---|---|
| Urine Dipstick Test | Quick screening for protein presence |
| 24-Hour Urine Collection | Quantitative measurement of proteinuria |
| Blood Pressure Measurements | Assess for hypertension, a sign of preeclampsia |
| Serological Tests | Evaluate for GDM and kidney function |
| Ultrasound | Assess kidney structure and function |
Management Strategies for Proteinuria in Pregnant Women
Management of proteinuria during pregnancy depends on the underlying cause and severity. Here are some general strategies:
Monitoring
Regular monitoring of blood pressure and protein levels is essential for women diagnosed with preeclampsia or those at risk. This includes frequent visits to healthcare providers to track changes in health status.
Lifestyle Modifications
- Dietary Changes: A low-sodium diet may help manage hypertension associated with proteinuria (Lee et al., 2018).
- Physical Activity: Moderate exercise may be recommended, provided there are no contraindications (Chen et al., 2025).
Medical Management
- Antihypertensive Medications: Medications such as methyldopa or labetalol may be prescribed to manage elevated blood pressure in preeclampsia (McIntyre et al., 2019).
- Insulin Therapy: For women diagnosed with GDM, insulin therapy may be required to maintain glucose levels within a normal range (He et al., 2019).
Delivery Planning
In cases of severe preeclampsia or other complications, early delivery may be necessary to protect the health of both mother and child. This decision is typically made by a healthcare provider based on the severity of the condition and gestational age (Ostermann et al., 2020).
FAQ
What does protein in urine mean during pregnancy?
Protein in urine can indicate various conditions, including preeclampsia, gestational diabetes, or urinary tract infections. It is essential to follow up with your healthcare provider for further evaluation.
How is proteinuria diagnosed during pregnancy?
Proteinuria is typically diagnosed through urine dipstick tests during routine check-ups, followed by 24-hour urine collection for quantification if necessary.
What are the potential risks of proteinuria during pregnancy?
Proteinuria can signify serious conditions such as preeclampsia, which can lead to complications for both mother and child if left untreated.
How is proteinuria managed in pregnant women?
Management may involve regular monitoring, lifestyle changes, and medical treatments depending on the underlying cause and severity of proteinuri
Should I be concerned if I have protein in my urine during pregnancy?
Yes, it is essential to discuss any findings of proteinuria with your healthcare provider to determine the appropriate next steps and ensure the health of you and your baby.
References
- Chen, X., Deng, Y., Fu, C., Yang, X., Gao, L. (2025). A physical activity counseling intervention to promote health among pregnant women: a study protocol of randomized clinical trial. https://doi.org/10.1186/s12884-025-07268-x
- He, Z., Xie, H., Liang, S., Tang, Y., Ding, W., Wu, Y. (2019). Influence of different diagnostic criteria on gestational diabetes mellitus incidence and medical expenditures in China. J Diabetes Investig
- Jiang, L., Tang, K., Magee, L. A., von Dadelszen, P., Ekeroma, A., Li, X. (2022). A global view of hypertensive disorders and diabetes mellitus during pregnancy. Nat Rev Endocrinol. https://doi.org/10.1038/s41574-022-00734-y
- McIntyre, H. D., Catalano, P., Zhang, C., Desoye, G., Mathiesen, E. R., Damm, P. (2019). Gestational diabetes mellitus. Nat Rev Dis Primers. https://doi.org/10.1038/s41572-019-0098-8
- Ostermann, M., Liu, K. (2020). Pathophysiology of AKI. Best Pract Res Clin Anaesthesiol. https://doi.org/10.1016/j.bpa.2017.09.001
- Lee, K. W., Ching, S. M., Ramachandran, V., Yee, A., Hoo, F. K., Chia, Y. C. (2018). Prevalence and risk factors of gestational diabetes mellitus in Asia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. https://doi.org/10.1186/s12884-018-2131-4