Table of Contents
Analyzing Protein in Urine: Techniques and Technologies
The analysis of protein in urine has evolved significantly with the advent of advanced technologies. Traditional methods such as dipstick tests and 24-hour urine collections are being complemented and, in some cases, replaced by innovative techniques that provide more accurate and timely results.
-
Mass Spectrometry: This technique allows for the precise quantification of various proteins in urine, which can help in differentiating between types of proteinuria. For instance, it can identify albuminuria versus non-albumin proteinuria, which is crucial for understanding the underlying pathology.
-
Immunoassays: These are commonly used for the detection of specific proteins such as albumin and globulins. The sensitivity and specificity of immunoassays have improved, enabling clinicians to detect proteinuria at lower thresholds.
-
Nanoparticle-Based Technologies: Recent advances in nanoparticle-based drug delivery systems are being explored for their potential in kidney imaging and treatment. These technologies can enhance the visibility of renal structures and facilitate targeted therapy for conditions associated with proteinuria (Li et al., 2023).
The integration of these technologies into clinical practice has the potential to revolutionize the management of proteinuria. For instance, the use of mass spectrometry in routine laboratories can enable early detection of diabetic nephropathy, allowing for timely intervention to prevent progression to end-stage renal disease.
Clinical Significance of Protein in Urine Images
The clinical significance of protein in urine images cannot be overstated. The presence of protein in urine is often a harbinger of significant underlying pathology, and its quantification can guide management decisions. Recent studies have highlighted the role of proteinuria as a prognostic marker in various conditions.
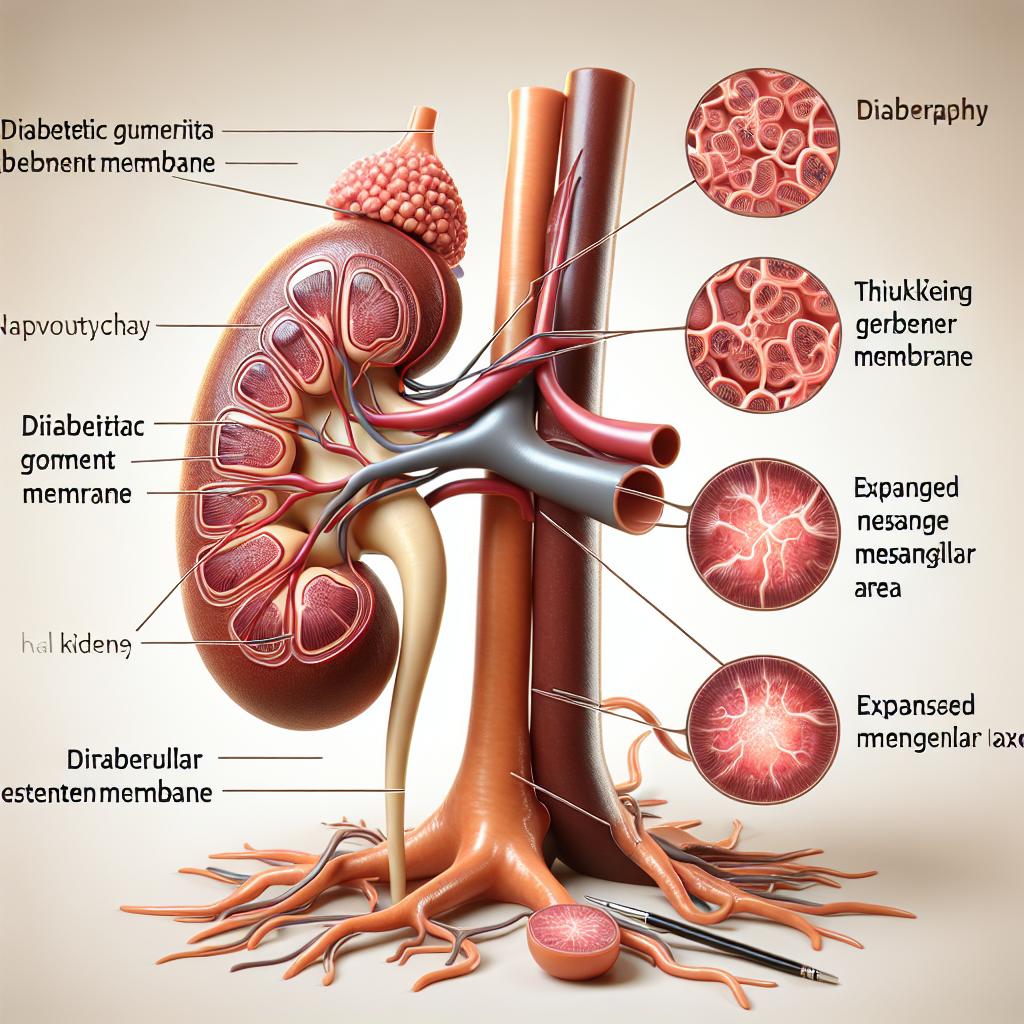
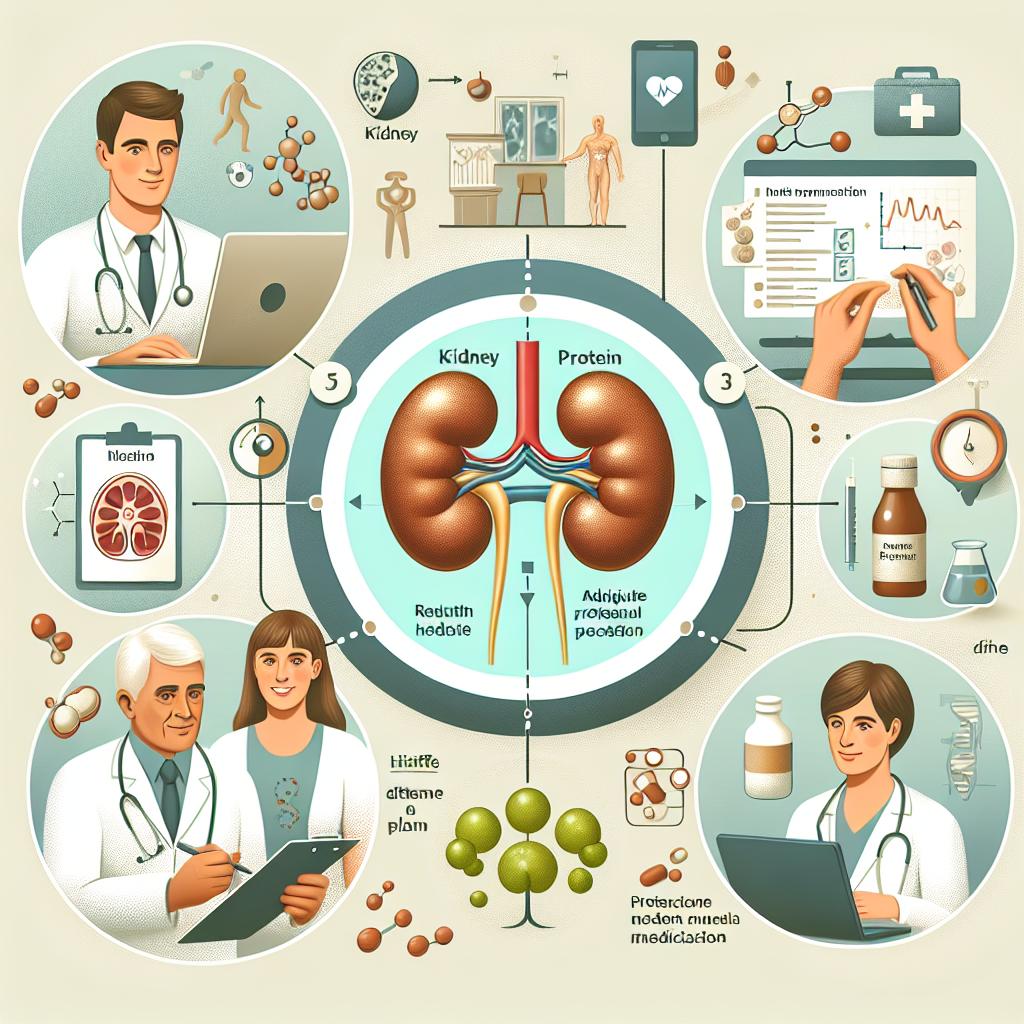
In diabetic nephropathy, for example, the degree of proteinuria is closely linked to disease progression. Patients with higher levels of proteinuria often experience more rapid declines in renal function, and imaging studies can help in monitoring these changes over time. Furthermore, the integration of imaging findings with clinical data can assist in stratifying patients based on risk and tailoring personalized treatment strategies.
Additionally, proteinuria is frequently associated with cardiovascular diseases. Research indicates that patients with proteinuria are at a higher risk for cardiovascular events, emphasizing the need for comprehensive cardiovascular risk assessment in these patients (Zhang et al., 2022). Imaging techniques that can visualize both renal and cardiovascular systems provide an invaluable tool for understanding the interplay between these two domains.
Table 2: Clinical Implications of Proteinuria
| Clinical Condition | Implications of Proteinuria |
|---|---|
| Diabetic Nephropathy | Accelerated renal decline |
| Cardiovascular Disease | Increased risk of events |
| Hypertension | Indicator of underlying vascular damage |
Overall, the clinical significance of protein in urine images lies in their ability to provide holistic insights into patient health, guiding interventions that can improve outcomes.
Future Directions in Proteinuria Imaging and Research
The future of proteinuria imaging and research is poised for exciting advancements. Emerging technologies and methodologies are being explored to enhance our understanding of proteinuria and its implications.
-
Artificial Intelligence (AI): AI and machine learning algorithms are being developed to analyze imaging data more efficiently. These technologies can assist in identifying patterns and predicting disease outcomes based on imaging findings.
-
Biomarker Discovery: Ongoing research is focused on identifying novel biomarkers associated with proteinuria. These biomarkers could lead to more targeted therapies and improved monitoring of disease progression.
-
Personalized Medicine: The integration of imaging with genetic and molecular profiling could pave the way for personalized treatment approaches. By understanding individual patient profiles, clinicians can tailor interventions that are more effective and less invasive.
As research in this area continues to evolve, the clinical application of these findings will undoubtedly enhance patient care and outcomes in those with proteinuria.
FAQ
What does the presence of protein in urine indicate?
The presence of protein in urine, or proteinuria, may indicate kidney damage or disease, as well as other systemic conditions like diabetes or hypertension.
How is proteinuria diagnosed?
Proteinuria is commonly diagnosed through dipstick tests, 24-hour urine collections, and more advanced techniques such as mass spectrometry and immunoassays.
What are the implications of proteinuria on overall health?
Proteinuria can be a marker of significant health issues, including kidney disease and increased cardiovascular risk, necessitating comprehensive management.
What new technologies are being used to analyze protein in urine?
Emerging technologies include mass spectrometry, immunoassays, and nanoparticle-based systems, improving the accuracy and efficiency of protein analysis.
What is the future of proteinuria research?
Future research may focus on AI applications, biomarker discovery, and personalized medicine approaches to enhance the understanding and management of proteinuri
References
- Li, X., & Zhang, Y. (2023). Recent advances and prospects of nanoparticle-based drug delivery for diabetic ocular complications. Retrieved from https://doi.org/10.7150/thno.108691
- Zhang, L., & Chen, H. (2022). Clinical value of [18F]AlF-Thretide PET/CT and early-time-point PET acquisition in the detection and staging of prostate cancer. Retrieved from https://doi.org/10.7150/thno.103667
- Wang, J., & Liu, T. (2025). REDD1-dependent GSK3β signaling in podocytes promotes canonical NF-κB activation in diabetic nephropathy. Retrieved from https://doi.org/10.1016/j.jbc.2025.108244
- Kim, S., & Park, J. (2025). The inflammatory endotype in osteoarthritis: Reflections from the 2024 OARSI clinical trials symposium (CTS) with a special emphasis on feasibility for clinical development. Retrieved from https://doi.org/10.1016/j.ocarto.2025.100572
- Chen, Y., & Huang, M. (2025). CHAC1 Mediates Endoplasmic Reticulum Stress‐Dependent Ferroptosis in Calcium Oxalate Kidney Stone Formation. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11905043/