Table of Contents
Impact of pH of Urine on Overall Wellbeing
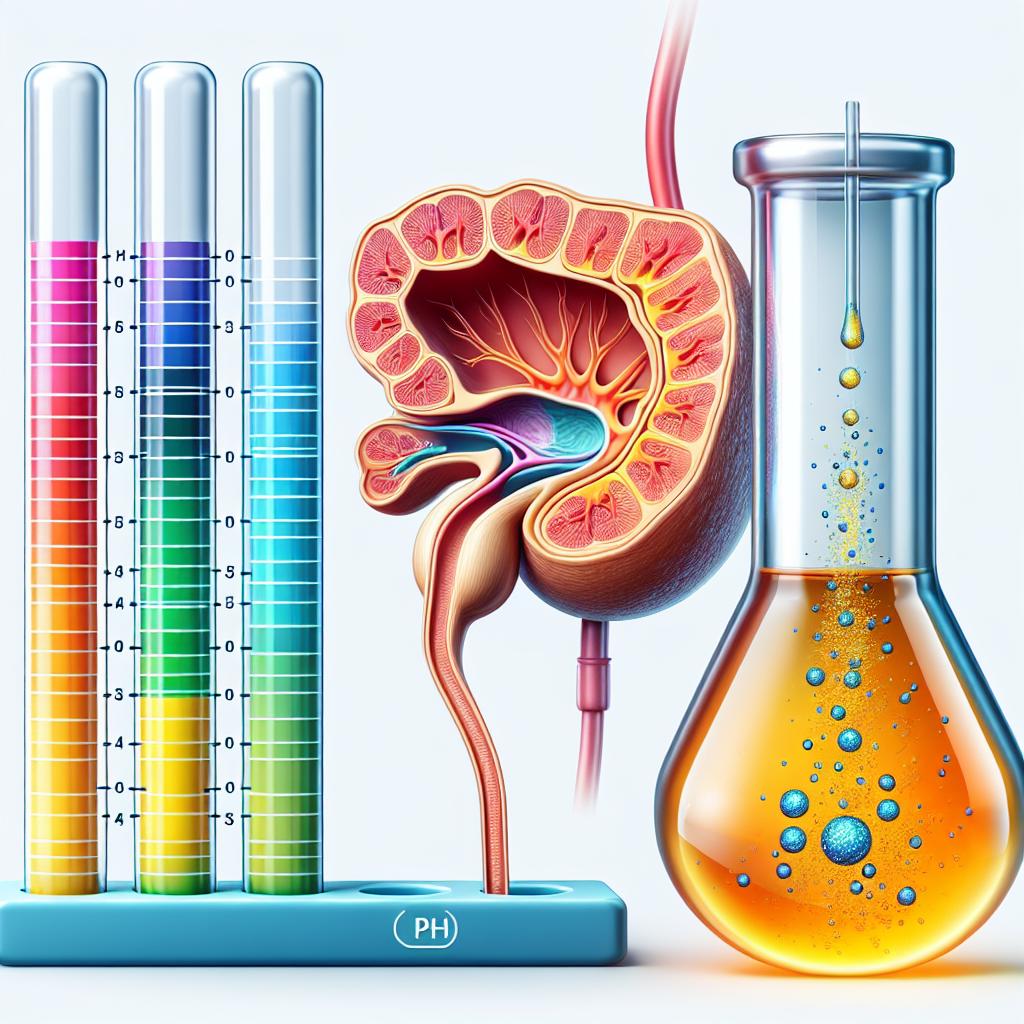
Urine ph is a reflection of the body’s acid–base status and is influenced by the metabolism of proteins, fats, and carbohydrates. The normal urine pH range typically falls between 4.5 and 8.0, with a slightly acidic pH being most common in healthy individuals. The balance of urine pH is critical because it affects the solubility of various substances in urine, which in turn influences the formation of kidney stones and the risk of urinary tract infections. When the urine pH becomes too acidified or too alkaline, it predisposes individuals to certain pathological conditions. For example, highly acidic urine may promote the formation of uric acid or cystine stones, while overly alkaline urine could favor the precipitation of calcium phosphate crystals. These imbalances can lead to discomfort, kidney damage, and chronic urinary issues that ultimately affect one’s overall health and quality of life.
There is emerging evidence that maintaining an optimal urine pH contributes not only to renal health but also to systemic wellbeing. A balanced acid–base environment in the body is essential for efficient metabolic function, proper enzymatic activities, and the maintenance of healthy tissues. Although much of the current research focuses on other biomarkers and fluid parameters in the diagnostic field ([2], [4], [5]), the clinical significance of urine pH remains an important parameter in evaluating patient health. By understanding how urine pH interacts with diet and metabolism, healthcare professionals are better equipped to provide personalized medical advice. This connection between urine pH and overall health supports the idea of using urine pH measurements as part of routine health assessments to identify early signs of metabolic disturbances.
Accurate Measurement Techniques for pH of Urine
Accurate measurement of urine pH is fundamental for effective clinical diagnosis and patient management. Over the years, a variety of methods have been developed to measure urine pH, each with its own merits, limitations, and sensitivity. The most common techniques include the use of pH indicator strips (litmus paper), pH meters with electrode sensors, and digital devices designed specifically for home or clinical use.
pH indicator strips remain a popular choice because they are cost‐effective, require minimal equipment, and provide rapid results. However, these strips may be subject to subjective interpretation, and their accuracy is dependent on the quality of the strips and proper storage conditions. In contrast, pH meters equipped with glass electrode sensors provide a highly accurate and quantitative analysis of urine pH. These electronic devices are favored in clinical laboratories due to their reproducibility, ease of calibration, and minimal operator‐dependent variability. Some advanced pH meters even offer data logging and integration with electronic health records, which is beneficial for longitudinal tracking of a patient’s acid–base status.
Innovative advancements in sensor technology continue to refine the measurement of urine pH, optimizing the detection limit and reducing potential interferences from proteins, electrolytes, and other urinary solutes. This is especially important in research and clinical diagnosis where small variations in pH could indicate underlying pathology. As technology evolves, researchers are exploring novel sensor materials and miniaturized platforms to develop portable and affordable devices that can accurately measure urine pH in real time. Accurate pH measurement is central in not only diagnosing conditions related to kidney and urinary tract health but also in monitoring the effectiveness of dietary or pharmacological interventions aimed at regulating systemic acid load ([2], [4], [5]).
Dietary Practices that Influence pH of Urine
Diet remains one of the most influential factors in regulating the pH of urine, with both the type and quantity of food consumed playing critical roles. A diet rich in fruits and vegetables tends to produce more alkaline urine due to the metabolism of organic anions such as citrate, malate, and bicarbonate precursors. Conversely, consumption of high amounts of animal proteins, especially those containing sulfur‐containing amino acids, can lead to a more acidic urine due to the generation of sulfuric acid as a metabolic end product.
For individuals aiming to optimize their urine pH, dietary modification is a practical and noninvasive method. Incorporating an increased proportion of vegetables, fruits, nuts, and legumes while reducing the consumption of red meat and processed foods can favorably modulate urine pH. In some cases, clinical nutritionists recommend specific dietary approaches such as the alkaline diet, which emphasizes the intake of foods that help raise urine pH, thereby countering the chronic acid load that may contribute to bone demineralization and kidney stone formation.
In addition to macronutrient composition, other dietary factors such as fluid intake, intake of citrate-rich foods (for example, lemons and oranges), and even certain dairy products may influence urine pH. It is crucial to note that the relationship between diet and urine pH can vary among individuals due to genetic variability, gut microbiota composition, and underlying metabolic differences. A well-balanced diet not only supports a healthier urine pH but also enhances overall hydration and metabolic function, thereby reducing the risk of associated health complications. Although many researchers have investigated the impact of various biomarkers in clinical diagnosis ([2], [4], [5]), the interplay between diet and urine pH remains an area of paramount importance for both preventive health and therapeutic interventions.
pH of Urine as a Biomarker in Clinical Diagnosis
Urine pH is an accessible biomarker that can provide clinicians with valuable information regarding an individual’s acid–base balance and overall metabolic state. Because urine collection is noninvasive and can be performed repeatedly over time, it is often used to monitor treatments for metabolic acidosis, renal tubular acidosis, urinary tract infections, and other conditions. Variations in urine pH can also signal systemic issues such as chronic kidney disease or contribute to the diagnostic workup in patients with suspected metabolic disorders.
For instance, persistently low urine pH may be associated with an increased risk of uric acid kidney stones, whereas consistently high urine pH may predispose individuals to calcium phosphate stone formation. In clinical practice, urine pH is often considered alongside other laboratory tests such as serum electrolytes, blood pH, and bicarbonate levels to construct a comprehensive picture of a patient’s metabolic status.
Furthermore, abnormalities in urine pH may serve as early indicators for conditions like urinary tract infections or even certain systemic diseases. Its role as a diagnostic tool is reinforced by its simplicity and the fact that it reflects changes in dietary intake, medication adherence, and the progression or resolution of disease processes. Although many studies have extended the investigation of biomarkers in different bodily fluids ([2], [4], [5]), urine pH remains an essential biomarker in the clinical setting due to its unique properties and ease of measurement. Advancing the integration of urine pH measurements into routine clinical screening could help identify metabolic imbalances earlier and improve the overall management of diseases influenced by acid–base status.
Approaches for Maintaining an Optimal pH of Urine
Maintaining an optimal urine pH is a multifaceted endeavor that involves lifestyle modifications, dietary adjustments, and careful management of underlying health conditions. A proactive approach to regulating urine pH begins with enhanced hydration, which helps dilute urinary solutes and facilitates the excretion of acids. Adequate fluid intake plays a crucial role in both preventing kidney stone formation and maintaining an appropriate acid–base balance.
From a dietary standpoint, individuals are encouraged to adjust their nutrient intake according to their specific health needs. For those with a tendency toward acidic urine, increasing the consumption of alkaline-forming foods such as leafy greens, fruits, and certain legumes can be beneficial. At the same time, reducing the ingestion of high-protein, sulfur-rich foods can help mitigate excessive acid production. In some instances, physicians might also recommend supplementation with alkaline agents such as potassium citrate, particularly for patients who are prone to kidney stone formation or have a diagnosis of renal tubular acidosis.
Beyond diet and hydration, regular monitoring and personalized healthcare are essential for maintaining optimal urine pH. Health professionals may advise periodic measurement of urine pH in patients with known metabolic abnormalities or those undergoing specific dietary regimens. Incorporating pH monitoring into a comprehensive wellness program not only supports immediate clinical decision-making but also encourages long-term behavioral adjustments that promote overall health. The integration of noninvasive diagnostic tools into routine practice has been bolstered by recent advancements in sensor technology ([2], [4], [5]), which allow for real-time assessments and enhance patient engagement in self-monitoring.
Another important aspect is understanding individual variability and ensuring that any intervention is tailored to the patient. Factors such as age, sex, comorbidities, and even genetic predispositions may affect one’s baseline urine pH and the response to dietary interventions. Personalized medicine approaches, including the use of mobile health applications that sync with digital pH meters, are emerging as innovative ways to provide patients and clinicians with accurate and actionable data on urine pH. Such data-driven approaches empower individuals to make informed decisions about their nutrition and lifestyle while allowing healthcare providers to adjust treatment protocols as needed.
Frequently Asked Questions (FAQ)
What is the normal range for urine pH?
The normal urine pH typically ranges from 4.5 to 8.0, with a slightly acidic pH being common in healthy individuals. Variations outside this range may indicate metabolic disorders or dietary imbalances.
How can I accurately measure my urine pH at home?
The most common methods include using pH indicator strips or digital pH meters. ph strips are inexpensive and provide quick results, while digital pH meters provide more precise readings and are often used in clinical settings.
Which foods can help maintain an optimal urine pH?
Foods that promote a more alkaline urine include fruits, vegetables, nuts, and legumes. Reducing intake of high-protein and sulfur-containing foods such as red meats can help prevent excessive acidification.
Why is urine pH important in clinical diagnosis?
Urine pH is a useful biomarker for assessing acid–base balance, which in turn affects renal function and the risk of kidney stone formation. It provides clinicians with insights into metabolic health and can help in monitoring diseases like metabolic acidosis and urinary tract infections.
What lifestyle changes can support optimal urine pH?
Adequate hydration, a balanced diet rich in alkaline-forming foods, and routine monitoring of urine pH are important. Additionally, managing underlying health conditions and, if necessary, incorporating supplements like potassium citrate under medical supervision can also be beneficial.
Can urine pH be used to monitor the effectiveness of dietary changes?
Yes. Because urine pH directly reflects changes in dietary intake and metabolism, it can be an effective parameter to track the effectiveness of dietary interventions aimed at balancing the body’s acid load.
References
- Chen, J., et al. (2025). Effects of increasing levels of rubber seed cake on growth performance, nutrient digestion metabolism, serum biochemical parameters, and rumen microbiota of Hu sheep. https://doi.org/10.1186/s12917-025-04503-7
- Wang, Z., et al. (2025). Trendelenburg position is a reasonable alternative to passive leg raising for predicting volume responsiveness in mechanically ventilated patients in the ICU. https://doi.org/10.1186/s13054-025-05301-1
- [Author Unknown]. (n.d.). Effect of the Sugar Present in the Culture Medium on the Preservation of Human RPE Cell Suspensions. https://pubmed.ncbi.nlm.nih.gov/11798337/
- [Author Unknown]. (n.d.). Mastic Kidney: A Rare Radiological Feature. https://doi.org/10.7759/cureus.77014
- Yıldız, F., LeBaron, T. W., & Alwazeer, D. (2025). A comprehensive review of molecular hydrogen as a novel nutrition therapy in relieving oxidative stress and diseases: Mechanisms and perspectives. https://doi.org/10.1016/j.bbrep.2025.101933
- [Author Unknown]. (n.d.). Detection of AdeAB, TetA, and TetB efflux pump genes in clinical isolates of tetracycline-resistant Acinetobacter baumannii from patients of Suez Canal University Hospitals. https://doi.org/10.1186/s12866-024-03735-1
- Chen, J. (2025). Development of a machine learning model related to explore the association between heavy metal exposure and alveolar bone loss among US adults utilizing SHAP: a study based on NHANES 2015–2018. https://doi.org/10.1186/s12889-025-21658-y
- Khayatan, D., Barzegar, P. E. F., Fatima, A., Sattar, T., Zahid, A., Batool, S. A., Jabbar, M., Mureed, M., Haider, F., Butt, A. J., Hanif, S., & Seifalian, A. (2024). Advancements in lung regeneration: from bench to bedside. https://doi.org/10.1186/s12967-024-05954-6