Table of Contents
Definition and Significance of Mixed Flora in Urine
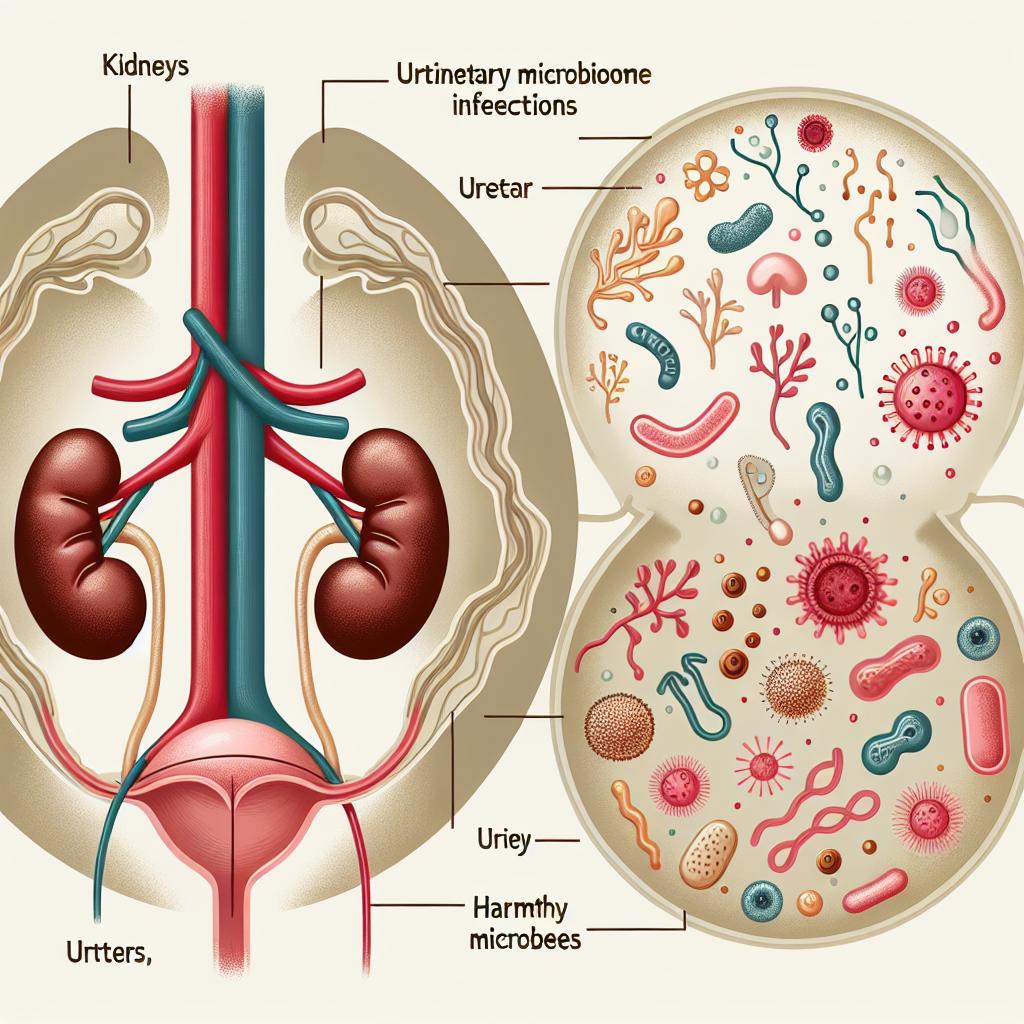
Mixed flora in urine refers to the presence of multiple types of microorganisms, including bacteria, fungi, and occasionally viruses, in a urine sample. This phenomenon often indicates a deviation from normal urinary microbiota, which typically consists of a limited range of species. In healthy individuals, urine is generally considered sterile; however, the detection of mixed flora can signify underlying health issues, particularly relating to urinary tract infections (UTIs) or other systemic conditions (Köhler et al., 2025).
The clinical significance of mixed flora is profound, as it poses challenges for diagnosis and treatment. The presence of multiple organisms complicates the identification of the causative pathogen, making it difficult to select appropriate antimicrobial therapies. Furthermore, understanding the implications of mixed flora in urine is essential for clinicians, as these findings can influence treatment regimens, patient management strategies, and prognostic assessments.
Common Causes of Mixed Flora Presence in Urine Samples
Several factors contribute to the presence of mixed flora in urine samples, including:
-
Urinary Tract Infections (UTIs): The most common cause of mixed flora in urine is a UTI, where an infection may be caused by multiple pathogens, particularly in complicated cases or recurrent infections. Infections may arise from various sources, including the introduction of bacteria from the gastrointestinal tract or external environments (Zhao et al., 2024).
-
Contamination: Contamination during urine collection is another frequent cause. Improper collection techniques can introduce bacteria from the skin or genital area into the urine sample, leading to the appearance of mixed flora (Li et al., 2022).
-
Recent Antibiotic Use: Antibiotic therapy can alter the urinary microbiome, allowing for opportunistic pathogens to proliferate. This disruption can lead to the emergence of mixed flora, as antibiotics may eliminate sensitive organisms while allowing resistant ones to thrive (Liu et al., 2024).
-
Chronic Health Conditions: Patients with chronic diseases, such as diabetes mellitus or immunosuppressive conditions, are at higher risk for developing mixed flora in the urine. These conditions can alter the normal urinary microbiome, making it more susceptible to infections (Duan et al., 2025).
-
Anatomical Abnormalities: Structural abnormalities in the urinary tract, such as strictures or obstructions, can predispose individuals to infections with mixed flora due to retained urine and bacterial growth (Miao et al., 2024).
Table 1: Common Causes of Mixed Flora in Urine
| Cause | Description |
|---|---|
| Urinary Tract Infections | Infections caused by multiple pathogens, typically bacteria. |
| Contamination | Introduction of bacteria during sample collection. |
| Recent Antibiotic Use | Disruption of normal flora, allowing resistant pathogens to thrive. |
| Chronic Health Conditions | Diseases that alter the urinary microbiome. |
| Anatomical Abnormalities | Structural issues leading to urine retention and bacterial growth. |
Impact of Mixed Flora on Urinary Tract Infections
The presence of mixed flora in urine significantly impacts the diagnosis and treatment of urinary tract infections. In cases where multiple pathogens are identified, the treatment becomes more complicated, as the effectiveness of standard antibiotic regimens may be compromised.
Diagnostic Challenges
Traditional diagnostic methods often rely on the identification of a single causative organism; however, the presence of mixed flora can obscure this process. Diagnostic tests may yield false negatives or positives, complicating the clinical picture and potentially leading to inappropriate treatment (Krisher et al., 2024).
Treatment Complications
The presence of mixed flora may necessitate broader antibiotic coverage or the use of combination therapies, which can lead to increased side effects and a higher risk of developing antibiotic resistance. Additionally, the emergence of resistant strains can prolong the duration of infection and complicate patient outcomes (Duan et al., 2025).
Increased Morbidity
Patients with mixed flora in urine are at an increased risk for recurrent infections, chronic UTIs, and even systemic complications. This higher morbidity emphasizes the need for thorough evaluation and tailored treatment strategies for affected individuals (Li et al., 2022).
Diagnostic Approaches for Identifying Mixed Flora in Urine
Diagnosing mixed flora in urine typically involves several steps:
-
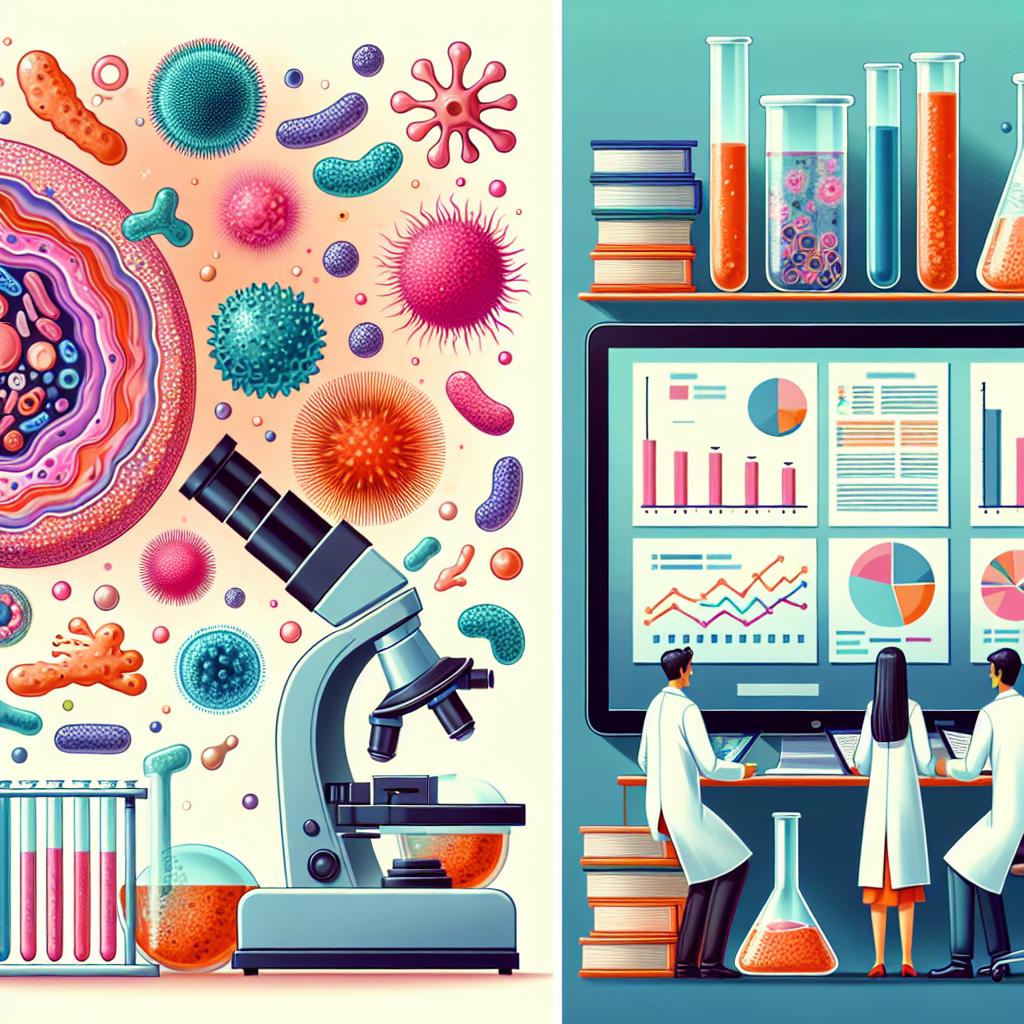
Urinalysis: Initial evaluation through urinalysis can indicate the presence of bacteria, white blood cells, and nitrites, which are suggestive of infection.
-
Culture and Sensitivity Testing: Culturing the urine sample on selective media allows for the growth and identification of specific microorganisms. This process may include quantitative cultures to determine the significance of the findings (Liu et al., 2024).
-
Molecular Techniques: Polymerase chain reaction (PCR) and other molecular techniques can be employed to identify a broader range of pathogens, including those that may not grow well in culture conditions. These techniques can provide rapid results and improve diagnostic accuracy (Zhao et al., 2024).
-
Advanced Microbiome Analysis: Next-generation sequencing (NGS) technologies can analyze the complete urinary microbiome, allowing for the identification of all present microorganisms, including those that are not typically detected through standard culture methods (Duan et al., 2025).
Table 2: Diagnostic Approaches for Mixed Flora
| Method | Description |
|---|---|
| Urinalysis | Initial evaluation for signs of infection. |
| Culture and Sensitivity | Identification and susceptibility testing of pathogens. |
| Molecular Techniques | Use of PCR to identify microorganisms not easily cultured. |
| Advanced Microbiome Analysis | NGS technologies for comprehensive microbial profiling. |
Effective Management Strategies for Mixed Flora in Urine
Managing mixed flora in urine requires a multifaceted approach, tailored to the specific circumstances of the patient. Effective management strategies may include:
-
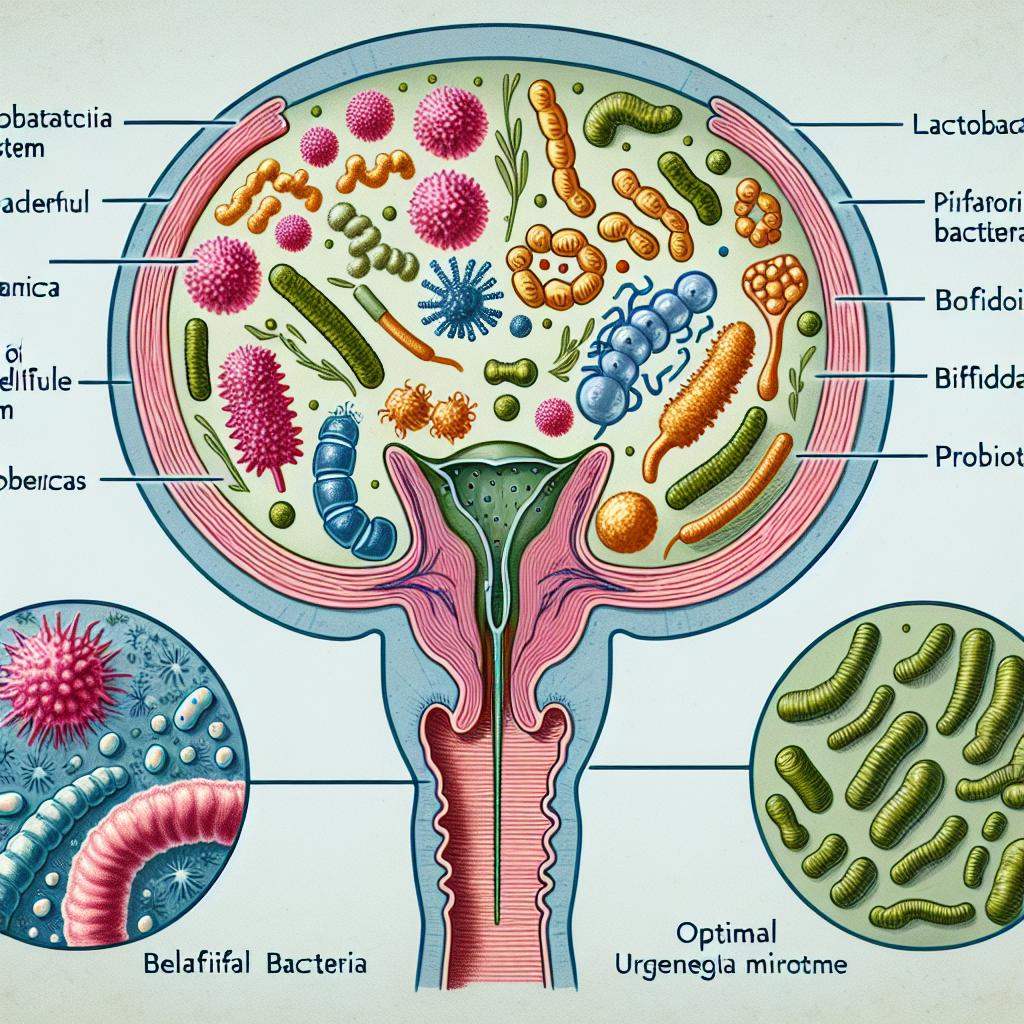
Tailored Antibiotic Therapy: Based on culture and sensitivity results, clinicians should select appropriate antibiotics that target the identified pathogens. In cases of polymicrobial infections, combination therapy may be warranted (Miao et al., 2024).
-
Antibiotic Stewardship: Implementing antibiotic stewardship programs can help reduce the prevalence of resistant strains and ensure more effective treatment of infections. This approach emphasizes the judicious use of antibiotics based on clinical guidelines and patient-specific factors (Li et al., 2022).
-
Educating Patients: Patient education on the importance of proper hygiene, fluid intake, and the risks of antibiotic misuse is essential for preventing future infections and managing existing conditions (Duan et al., 2025).
-
Monitoring and Follow-Up: Regular monitoring of patients with recurrent infections or chronic conditions is vital for timely intervention and adjustment of treatment plans as necessary. This can help prevent complications associated with mixed flora (Köhler et al., 2025).
-
Alternative Therapies: Exploring alternative therapies such as probiotics or bacteriophage therapy may provide additional options for managing recurrent UTIs caused by mixed flora. These strategies can help restore a balanced urinary microbiome and reduce the likelihood of future infections (Zhao et al., 2024).
Table 3: Management Strategies for Mixed Flora
| Strategy | Description |
|---|---|
| Tailored Antibiotic Therapy | Selection of antibiotics based on sensitivity testing. |
| Antibiotic Stewardship | Programs to optimize antibiotic use and reduce resistance. |
| Educating Patients | Informing patients about hygiene and antibiotic risks. |
| Monitoring and Follow-Up | Regular assessments to adjust treatment plans as needed. |
| Alternative Therapies | Exploring probiotics and bacteriophage therapy as adjunct treatments. |
FAQ
What does the presence of mixed flora in urine indicate? Mixed flora usually indicates a urinary tract infection or contamination during sample collection. It may also suggest underlying health issues or complications.
How is mixed flora diagnosed? Diagnosis typically involves urinalysis, culture and sensitivity testing, molecular techniques, and advanced microbiome analysis.
What are the treatment options for mixed flora in urine? Treatment options include tailored antibiotic therapy, antibiotic stewardship, patient education, monitoring, and alternative therapies such as probiotics or bacteriophage therapy.
Can mixed flora in urine lead to serious health complications? Yes, mixed flora can increase the risk of recurrent infections, chronic UTIs, and systemic complications, necessitating careful management.
References
-
Köhler, P., Ribeiro, A., Honarpisheh, M., von Rauchhaupt, E., Lorenz, G., Li, C., Martin, L., Steiger, S., Lindenmeyer, M., Schmaderer, C., Anders, H.-J., Thomasova, D., Lech, M. (2025). Podocyte A20/TNFAIP3 Controls Glomerulonephritis Severity via the Regulation of Inflammatory Responses and Effects on the Cytoskeleton. Retrieved from https://doi.org/10.3390/cells14050381
-
Zhao, X., Liu, H., Wang, Y., Zhang, F. (2024). Isolation and characterization of phage vB_SalM_SPJ41 and the reduction of risk of antibiotic-resistant Salmonella enterica contamination in two ready-to-eat foods. Retrieved from https://doi.org/10.3390/antibiotics12020364
-
Duan, X., Lv, X., Wang, X., Zhang, Y., Hu, Y., Li, H., Zhou, Y. (2025). Impact of immune cell metabolism on membranous nephropathy and prospective therapy. Retrieved from https://doi.org/10.1038/s42003-025-07816-3
-
Li, P., Ma, W., Shen, J., Zhou, X. (2022). Characterization of novel bacteriophage vB_KpnP_ZX1 and its depolymerases with therapeutic potential for K57 Klebsiella pneumoniae infection. Retrieved from https://doi.org/10.3390/pharmaceutics14091916
-
Liu, Q., Zhang, Y., Miao, H., Qu, Y. (2024). Novel Biomarkers in Membranous Nephropathy. Retrieved from https://doi.org/10.3389/fimmu.2022.845767