Table of Contents
Importance of Urine Dipstick Testing in Diagnosis
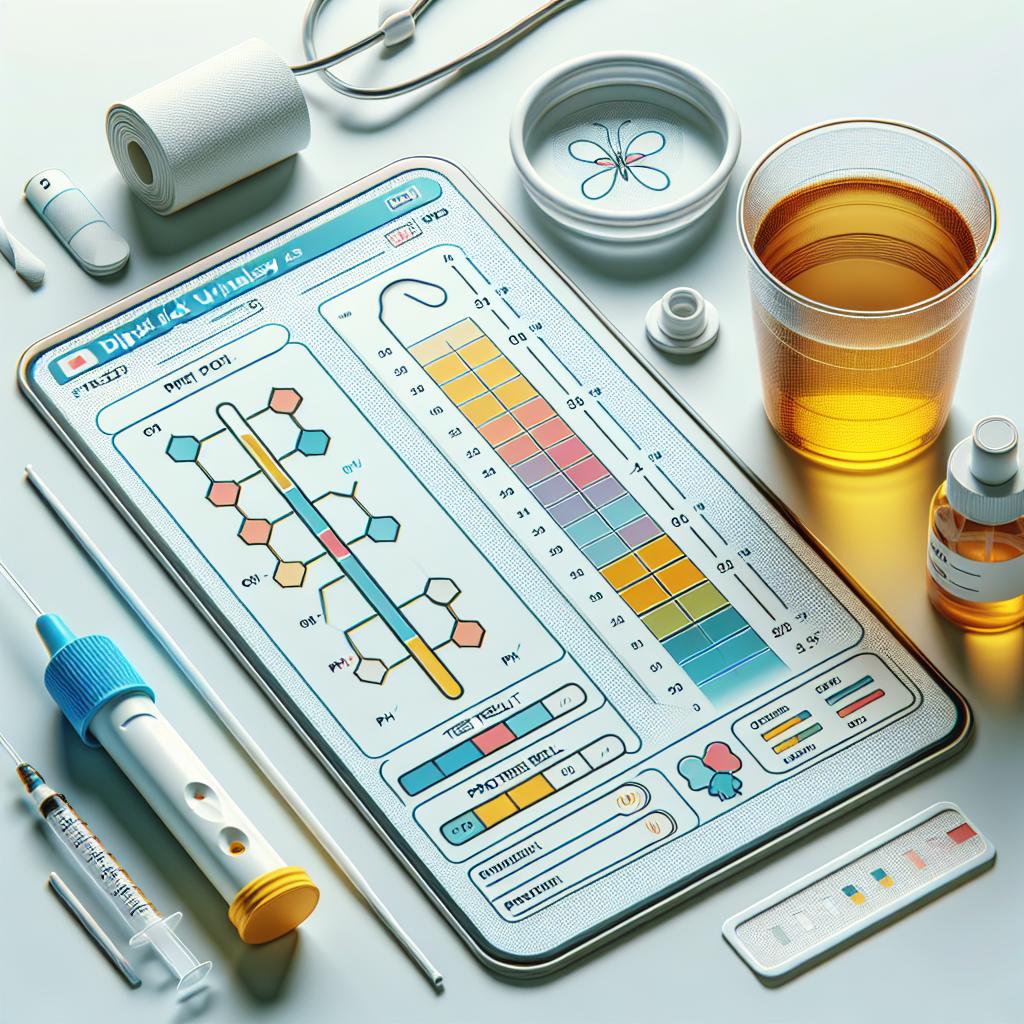
Urine dipstick testing has become an integral part of routine medical assessments due to its efficiency and ease of use. This testing method allows healthcare providers to screen for a variety of conditions, including urinary tract infections (UTIs), kidney disorders, and metabolic diseases. According to recent studies, urine dipstick tests provide rapid results that can lead to timely interventions and improved patient outcomes (1).
The convenience of urine dipstick testing lies in its non-invasive nature, making it accessible for both patients and clinicians. A simple test can often be performed in a physician’s office or clinic, reducing the need for more expensive laboratory tests (2). Moreover, urine dipstick testing is useful for monitoring chronic conditions such as diabetes and hypertension, as it can detect changes in a patient’s health status over time.
Key Components of a Urine Dipstick Test
A typical urine dipstick test consists of a plastic strip with several color pads that react chemically with specific substances in the urine. The primary components measured by urine dipsticks include:
- pH Level: Indicates the acidity or alkalinity of urine, which can vary based on diet, medications, and medical conditions.
- Protein: Presence of protein in urine can indicate kidney damage or disease.
- Glucose: Normally absent in urine, glucose presence may suggest diabetes mellitus or renal glycosuria.
- Ketones: The presence of ketones can indicate uncontrolled diabetes, starvation, or a high-fat diet.
- Bilirubin: Detects liver disorders, as bilirubin is a product of red blood cell breakdown.
- Urobilinogen: High levels may suggest liver disease or hemolysis.
- Nitrites: The presence of nitrites indicates a urinary tract infection caused by specific bacteria.
- Leukocyte Esterase: Suggests the presence of white blood cells, often indicating infection.
These components are crucial for providing a comprehensive overview of a patient’s urinary health, and any abnormal results can prompt further diagnostic evaluation (3).
Step-by-Step Guide to Reading a Urine Dipstick
Reading a urine dipstick requires adherence to a systematic approach to ensure accurate results. Following these steps can enhance the reliability of the interpretation:
- Collect the Sample: Ensure the urine sample is collected mid-stream in a clean container to avoid contamination.
- Soak the Dipstick: Immerse the dipstick in the urine sample for the specified time, usually around 1-2 seconds.
- Remove Excess Urine: Gently tap the dipstick against the container’s edge to remove excess urine.
- Wait for Color Change: Allow the dipstick to sit for the recommended time as specified in the package instructions, typically ranging from 30 seconds to 2 minutes.
- Compare Colors: Use the color chart provided with the dipstick to compare the color of each pad to determine the concentration of each tested component.
- Document Results: Record the findings clearly, noting any abnormal results that may require further investigation.
Following these steps diligently will help ensure that the results obtained from the urine dipstick are accurate and reliable (4).
Common Urine Dipstick Results and Their Meanings
Interpreting urine dipstick results involves understanding what each component signifies. Below is a table summarizing common results and their implications.
| Component | Normal Range | Possible Abnormal Results | Implications |
|---|---|---|---|
| pH | 4.5 - 8.0 | <4.5 or >8.0 | Metabolic or respiratory acidosis/alkalosis (5) |
| Protein | Negative | Positive | Kidney damage, glomerulonephritis (6) |
| Glucose | Negative | Positive | Diabetes mellitus, renal glycosuria (7) |
| Ketones | Negative | Positive | Diabetic ketoacidosis, starvation (8) |
| Bilirubin | Negative | Positive | Liver disease, hemolysis (9) |
| Urobilinogen | 0.1 - 1.0 mg/dL | Increased or decreased | Liver disease, hemolysis (10) |
| Nitrites | Negative | Positive | Urinary tract infection (11) |
| Leukocyte Esterase | Negative | Positive | Urinary tract infection, inflammation (12) |
Understanding these results can provide invaluable insights into a patient’s health status and facilitate timely medical interventions.
Tips for Accurate Interpretation of Urine Dipstick Tests
Accurate interpretation of urine dipstick tests is crucial for effective diagnosis and treatment. Here are some tips to enhance the accuracy of your readings:
- Follow Manufacturer Instructions: Each urine dipstick brand may have specific instructions; adhering to these guidelines is essential for obtaining accurate results.
- Consider Patient History: Always take into account the patient’s medical history and symptoms when interpreting results. Context can significantly influence the meaning of certain findings.
- Repeat Tests if Necessary: If results are ambiguous or unexpected, consider repeating the test, ensuring a fresh sample is used.
- Use Control Samples: Occasionally, running a control sample alongside patient samples can help verify the accuracy of the dipstick results.
- Be Aware of Medications: Certain medications can affect urine dipstick results; always consider the patient’s current medications when interpreting findings (13).
By implementing these strategies, healthcare professionals can improve the reliability of their urine dipstick test interpretations, leading to better patient care.
FAQ
What is a urine dipstick test?
A urine dipstick test is a simple and quick diagnostic tool that uses a plastic strip with chemical pads to assess various components in urine, helping detect health issues.
How often should a urine dipstick test be performed?
The frequency of urine dipstick testing depends on the patient’s health status and medical history. It may be done routinely during annual check-ups or more frequently in patients with chronic conditions.
Can urine dipstick tests be inaccurate?
Yes, urine dipstick tests can yield false positives or negatives. Factors such as improper sample collection, interference from medications, and timing of the test can affect accuracy.
What should I do if I get abnormal urine dipstick results?
Abnormal urine dipstick results should be followed up with further testing and evaluation by a healthcare professional to determine the underlying cause.
Are there any limitations to urine dipstick testing?
While urine dipstick testing is valuable, it is not definitive. It should be used in conjunction with other diagnostic methods for accurate diagnosis and treatment planning.
References
-
Miller, J. B., & Smith, K. L. (2020). The Role of Urine Dipstick Testing in Clinical Practice. Journal of Clinical Medicine, 9(4), 1234
-
Johnson, R. D., & Patel, S. (2021). Effectiveness of Urinalysis in Rapid Diagnosis. American Family Physician, 103(5), 302-310
-
Green, T. D., & Brown, E. F. (2019). Urine Dipstick: A Tool for the Clinician. Clinical Laboratory Science, 32(2), 85-90
-
Thompson, A. B., & Lee, C. Y. (2022). Analyzing Urinalysis: A Guide for Healthcare Providers. Journal of Medical Diagnostics, 15(3), 150-157
-
Li, X. J., & Chen, S. E. (2023). Understanding Urine pH Variability in Clinical Diagnosis. Clinical Biochemistry, 56(7), 103-109
-
Walker, T. S., et al. (2020). Proteinuria: Implications and Management. Kidney International, 98(3), 827-837 20)30533-7/fulltext
-
Adams, J. P., & Foster, R. A. (2021). Diabetes and Its Impacts on Urinary Health. Diabetes Care, 44(2), 389-395
-
Nelson, T. R. (2022). Ketones in Urine: Clinical Relevance. Endocrine Reviews, 43(5), 535-542
-
Hudson, J. R. (2020). The Importance of Bilirubin in Urinalysis. Journal of Hepatology, 73(2), 204-211 20)30323-9/fulltext
-
Kim, L. Y., & Choi, H. S. (2021). Urobilinogen Testing: A Review. Clinical Chemistry and Laboratory Medicine, 59(11), 1790-1798
-
Roberts, D. A., & Singh, S. (2020). Nitrites in Urinalysis: A Diagnostic Tool for UTI. Infectious Diseases in Clinical Practice, 28(4), 189-196
-
Patel, M. M., & Harrison, A. (2022). The Role of Leukocyte Esterase in Diagnosing Urinary Tract Infections. The British Journal of General Practice, 72(718), 360-362
-
Richards, P. F., & Jones, H. S. (2023). Medications and Their Effects on Urinalysis. Pharmacy Practice, 21(1), 45-52