Table of Contents
Overview of Leukocytes in Urine and Their Significance
Leukocytes, commonly known as white blood cells, play a crucial role in the immune system by defending the body against infections and diseases. The presence of leukocytes in urine, termed leukocyturia, can indicate several underlying health issues. In a healthy individual, urine typically contains few or no leukocytes. However, an increased number of leukocytes may suggest a urinary tract infection (UTI), kidney infection, or other inflammatory conditions in the urinary tract.
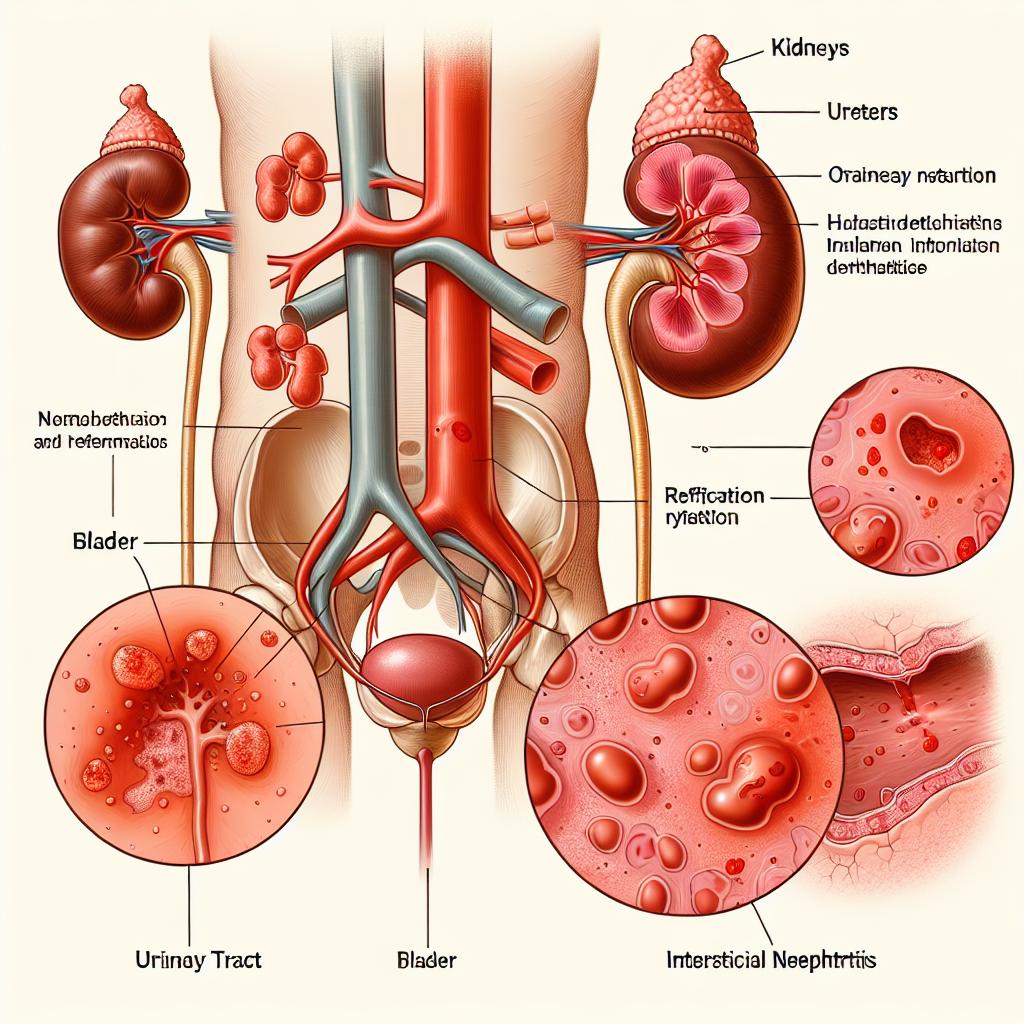
When leukocyturia occurs without the presence of nitrates, it raises specific concerns and necessitates a thorough evaluation. Nitrates are often produced by bacteria that cause UTIs. Therefore, the absence of nitrates in conjunction with leukocytes may suggest atypical infections, such as those caused by non-nitrate-reducing bacteria, or other non-infectious causes like interstitial nephritis or glomerulonephritis.
Understanding the significance of leukocytes in urine without nitrates is essential for accurate diagnosis and treatment. Healthcare providers often rely on urinalysis as a primary diagnostic tool. A standard urinalysis includes not only a visual and chemical examination but also a microscopic evaluation to assess the presence of leukocytes, red blood cells, bacteria, and other components. The interpretation of these findings can guide further diagnostic testing and management strategies.
Common Causes of Leukocytes in Urine Without Nitrates
The presence of leukocytes in urine without accompanying nitrates can be attributed to several conditions. Some of the most common causes include:
1. Non-bacterial Infections
- Viral infections of the urinary tract can lead to leukocyturia without the presence of nitrates. Such infections may be overlooked as they do not exhibit the typical bacterial signature found in UTIs.
2. Interstitial Nephritis
- This condition, characterized by inflammation of the kidney interstitium, can cause leukocytes to enter the urine. It may result from allergic reactions to medications, infections, or autoimmune diseases.
3. Glomerulonephritis
- Inflammation of the glomeruli can lead to the presence of leukocytes in urine. Glomerulonephritis may be caused by infections, autoimmune diseases, or systemic conditions like diabetes.
4. Kidney Stones
- The presence of kidney stones can irritate the urinary tract, leading to inflammation and an increased number of leukocytes in urine, even in the absence of nitrates.
5. Contamination
- Sometimes, urine samples may be contaminated during collection, leading to the presence of leukocytes. This is particularly common in women during menstruation.
6. Chronic Inflammatory Conditions
- Conditions such as lupus or other autoimmune diseases can lead to chronic inflammation of the urinary tract, resulting in leukocyturia without nitrates.
7. Post-surgical Effects
- Patients who have undergone urological surgeries may experience temporary leukocyturia due to inflammation or irritation of the urinary tract.
Diagnostic Approaches for Evaluating Leukocytes in Urine
When leukocytes are detected in urine without nitrates, a comprehensive approach is needed for diagnosis:
1. Urinalysis
- Initial screening through urinalysis provides crucial information regarding the presence of leukocytes, nitrates, proteins, and blood. A high leukocyte count with normal nitrite levels can be indicative of non-bacterial infections or other conditions.
2. Urine Culture
- A urine culture is critical for determining the presence of pathogens. A negative culture despite high leukocyte levels may prompt further investigation into non-bacterial causes.
3. Imaging Studies
- Ultrasound or CT scans may be recommended to evaluate for structural abnormalities, kidney stones, or signs of infection that may not be evident through urinalysis alone.
4. Blood Tests
- Blood tests can help assess kidney function and identify any systemic conditions, such as autoimmune disorders or infections.
5. Cystoscopy
- In some cases, a cystoscopy may be indicated to directly visualize the bladder and urethra, allowing for a more detailed examination of potential sources of inflammation or infection.
Implications of Leukocytes Presence in Urine Analysis
The presence of leukocytes in urine without nitrates can have several implications:
1. Increased Risk of Misdiagnosis
- Without the typical nitrate presence, clinicians may initially misdiagnose a UTI or overlook other potential conditions. This can lead to inappropriate treatment and further complications.
2. Need for Comprehensive Evaluation
- The findings necessitate a broader evaluation, including potential imaging and specialized tests to rule out serious conditions.
3. Treatment Delay
- A lack of definitive diagnosis may delay appropriate treatment, potentially worsening the patient’s condition, especially in instances of kidney inflammation or infection.
4. Monitoring of Chronic Conditions
- For patients with known chronic conditions, ongoing leukocyturia without nitrates may indicate disease exacerbation or complication, necessitating closer monitoring and possible adjustment of treatment plans.
Management and Treatment Options for Urinary Leukocytes
The management of leukocytes in urine without nitrates depends on the underlying cause. Treatment strategies may include:
1. Antibiotic Therapy
- If a bacterial infection is suspected, appropriate antibiotics should be initiated based on culture sensitivity results.
2. Anti-inflammatory Medications
- In cases of interstitial nephritis or other inflammatory conditions, corticosteroids or non-steroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce inflammation.
3. Surgical Intervention
- Patients with kidney stones or structural abnormalities may require surgical intervention to remove obstructions or correct anatomical issues.
4. Supportive Care
- Hydration and supportive care are important, especially in the case of acute infections or inflammatory conditions.
5. Monitoring and Follow-up
- Regular follow-up is necessary to monitor the resolution of symptoms and ensure effective treatment of the underlying condition.
Table 1: Common Causes of Leukocyturia Without Nitrates
| Cause | Description |
|---|---|
| Non-bacterial infections | Viral infections affecting the urinary tract |
| Interstitial nephritis | Inflammation of kidney interstitium |
| Glomerulonephritis | Inflammation of kidney glomeruli |
| Kidney stones | Irritation and inflammation caused by stones |
| Contamination | Sample contamination during collection |
| Chronic inflammatory conditions | Ongoing inflammation from autoimmune diseases |
| Post-surgical effects | Inflammation following urological surgeries |
FAQ Section
What does the presence of leukocytes in urine mean?
The presence of leukocytes in urine typically indicates an inflammatory response, often related to infections like UTIs, kidney infections, or other urinary tract disorders.
Why are nitrates significant in urine analysis?
Nitrates are produced by certain bacteria that typically cause UTIs. Their absence alongside leukocytes may indicate non-bacterial infections or other conditions.
How is leukocyturia diagnosed?
Diagnosis typically involves urinalysis, urine culture, imaging studies, and possibly blood tests to assess kidney function and rule out other conditions.
What are the treatment options for leukocyturia?
Treatment depends on the underlying cause and can include antibiotics, anti-inflammatory medications, supportive care, and possibly surgical intervention for anatomical issues.
When should I consult a doctor regarding leukocytes in urine?
If you notice symptoms like frequent urination, pain during urination, or any other concerning symptoms, it is important to consult a healthcare provider for evaluation.
References
- Alexander Wahba, Gudrun Kunst, Filip De Somer. (2024). EACTS/EACTAIC/EBCP Guidelines on cardiopulmonary bypass in adult cardiac surgery. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11826095/
- Revol-Cavalier, J., Quaranta, A., Newman, J. W., Hamberg, M., & Wheelock, C. E. (2024). The Octadecanoids: Synthesis and Bioactivity of 18-Carbon Oxygenated Fatty Acids in Mammals, Bacteria, and Fungi
- Tanasa (Acretei), M.-V., Negreanu-Pirjol, T., Olariu, L., Negreanu-Pirjol, B.-S., Lepadatu, A.-C., Anghel (Cireasa), L., & Rosoiu, N. (2025). Bioactive Compounds from Vegetal Organs of Taraxacum Species (Dandelion) with Biomedical Applications: A Review. Retrieved from https://doi.org/10.3390/ijms26020450
- Jomova, K., Alomar, S. Y., Nepovimova, E., Kuca, K., & Valko, M. (2024). Heavy metals: toxicity and human health effects. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11755068/
- Glover, S., Illyuk, J., Hill, C., McGuinness, B., McKnight, A. J., & Hunter, R. F. (2025). A systematic review of associations between the environment, DNA methylation, and cognition. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11776599/
- Jomova, K., & Valko, M. (2024). Heavy metals: toxicity and human health effects. Retrieved from https://doi.org/10.1007/s00204-024-03903-2