Table of Contents
Trends in Glucose‐Lowering Medications Among Kidney Transplant Recipients with T2D
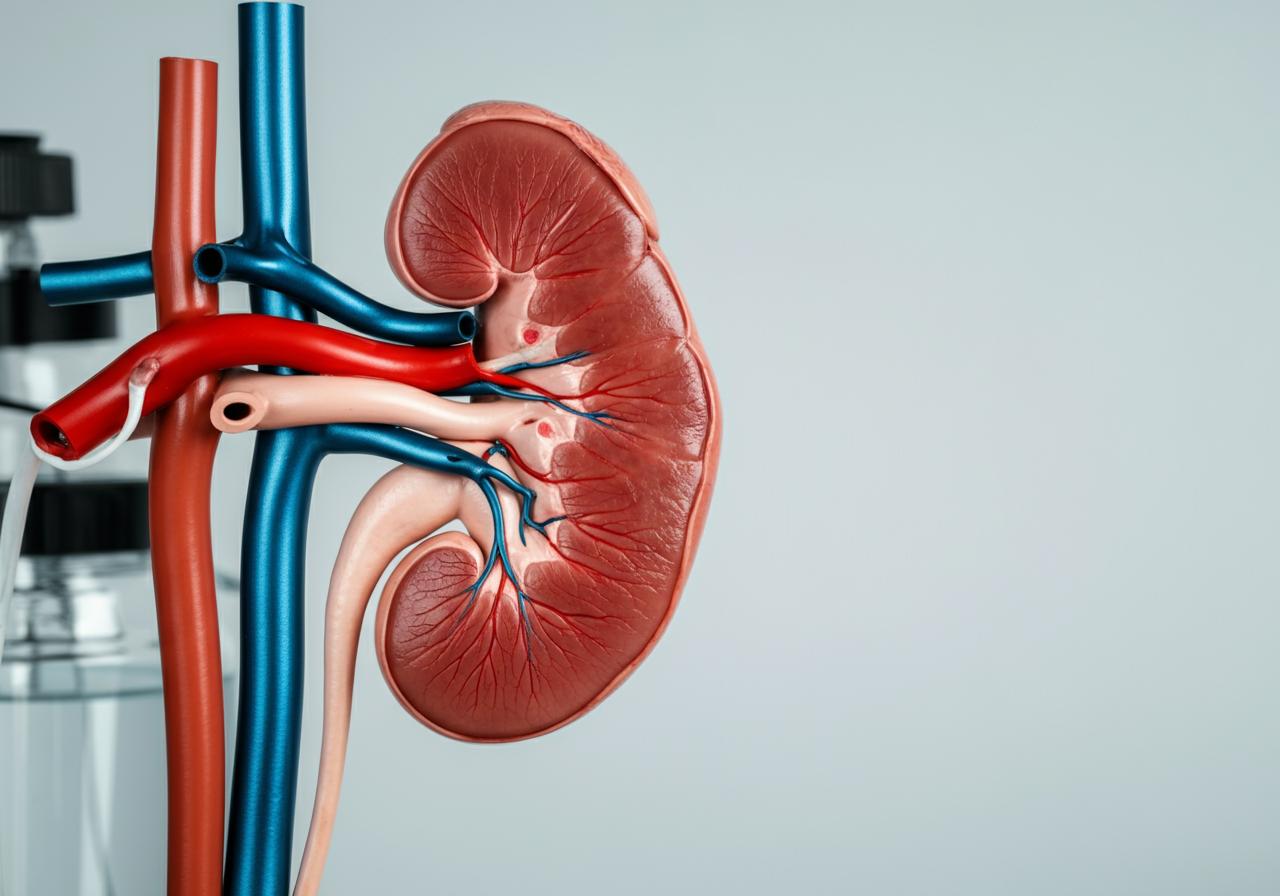
Kidney transplantation remains the preferred treatment to restore renal function in patients with end‐stage renal disease, and a significant proportion of these recipients suffer from type 2 diabetes. Maintaining optimal glycemic control in such patients is a formidable challenge as both pre‐existing and post‐transplant diabetes dramatically influence both graft survival and patient outcomes. Recent real‐world evidence from large U.S. health insurance claims databases shows that the utilization of glucose‐lowering medications (GLMs) in kidney transplant recipients with type 2 diabetes has undergone marked transformations over the past decade [6].
In these patient populations, insulin remains the most frequently prescribed GLM. However, its utilization has been gradually declining over time. Data indicate that while insulin usage was historically in the range of 74%–75%, more contemporary trends show a decline to approximately 58% from 2014 to 2023. Concomitantly, the popularity of newer medication classes such as sodium‐glucose cotransporter‐2 inhibitors (SGLT2is) and glucagon-like peptide-1 receptor agonists (GLP1RAs) have increased significantly. For instance, any use of SGLT2 inhibitors in this population increased from a negligible 0.4% in early 2014 to 14.4% by the latter half of 2023. Initiation of these medications shows similar upward trends; the incident use of SGLT2is increased post-2019, while GLP1RA initiation also steadily increased following 2017. Importantly, when compared with insulin, the initiation rates for these newer agents have nearly caught up by the end of the study period. Such shifts likely reflect accumulating evidence in non‐transplant populations that demonstrates benefits beyond glycemic control, including cardiovascular and renal protection [6].
The exploration of these trends is not only a matter of statistical interest—it has significant clinical implications. As newer GLM classes become more prevalent, clinicians are evaluating patient characteristics to optimize therapy. Evidence suggests that kidney transplant recipients initiated on SGLT2is tend to have a higher burden of cardiovascular comorbidities and increased proteinuria, whereas those starting on GLP1RAs have a higher prevalence of obesity. These nuances in patient selection underscore a possible paradigm shift where the decision-making process extends beyond strict glycemic considerations to a more holistic view that addresses cardiovascular risk and metabolic health [6].
Below is an example table summarizing selected clinical characteristics among kidney transplant recipients with treated type 2 diabetes who initiated different GLM classes:
| Clinical Characteristic | All Patients | SGLT2i Initiators | GLP1RA Initiators | Insulin Initiators |
|---|---|---|---|---|
| Number of Patients | 33,913 | 1,009 | 2,149 | 13,641 |
| Mean Age (years) | 59.3 ± 10.95 | 61.1 ± 10.34 | 58.0 ± 10.01 | 58.6 ± 10.65 |
| Male (%) | 62.1% | 64.8% | 56.4% | 64.0% |
| Prevalence of Hypertension (%) | 91.1% | 94.0% | 92.6% | 92.6% |
| Obesity (BMI ≥30 kg/m²) (%) | 32.4% | 41.7% | 53.1% | 34.3% |
| Prevalence of Proteinuria (%) | 17.5% | 25.0% | 18.1% | 17.5% |
Table 1. Clinical characteristics of kidney transplant recipients with type 2 diabetes, by type of GLM initiator (data adapted from [6]).
These findings highlight that over time, as the evidence base for newer medications strengthens, prescribing patterns adjust in accordance with individual patient risk factors, paving the way for more personalized treatment approaches in transplant care.
Advances in Ureteral Stenting Techniques in Kidney Transplantation
Surgical innovations have a profound impact on patient outcomes and healthcare costs, particularly in the field of kidney transplantation where urological complications remain a significant concern. One area of focus has been the stenting technique used to support the ureteroneocystostomy—the surgical anastomosis between the transplanted ureter and the recipient’s bladder. Historically, the externalized Single‐J stent was commonly used; however, several studies have underscored considerable urological complications associated with its use, including urinary leakage and ureteral strictures. Recent evidence now supports the use of a short internal Double‐J stent, which has been shown to reduce the incidence of these complications by nearly half compared to the Single‐J approach [7].
A randomized controlled trial conducted at a major transplant center evaluated the safety and effectiveness of long‐term Double‐J stenting versus short‐term Single‐J stenting in kidney transplantation. In this trial, kidney transplant recipients were randomized to receive either an externalized Single‐J stent that was removed approximately nine days after surgery or an internal Double‐J stent that remained in place for three weeks. The study reported that urological complications—including the need for percutaneous nephrostomy placement due to urinary leakage or significant hydronephrosis—were markedly lower in the Double‐J group. Moreover, the enhanced protocol facilitated earlier hospital discharge, thereby reducing healthcare costs and patient burden associated with additional procedures like cystoscopic stent removal [7].
The following table summarizes some key differences in outcomes between the two stenting approaches:
| Outcome | Single‐J Stenting | Double‐J Stenting |
|---|---|---|
| Urological Complication Rate | ~17.3% (externalized stents) | ~5.4% (internal stents) |
| Average Hospital Stay | Longer by approximately 2 days | Shorter hospital stay |
| Requirement for PCN Placement | Higher (~14.5%) | Lower (~1.5% as estimated) |
| Need for Additional Procedures | Removal via external catheter (additional hospital visit) | Removal via outpatient cystoscopy |
Table 2. Comparative outcomes of Single‐J versus Double‐J stenting in kidney transplantation (data adapted from [7]).
These findings suggest that transitioning to long‐term Double‐J stenting can improve post‐transplant outcomes by diminishing the frequency of urological complications. The reduction in complications not only translates into improved graft function and patient satisfaction but also underscores the cost‐effectiveness of this approach—a critical consideration in today’s healthcare systems.
Innovations in Infection Prevention: Chlorhexidine Bathing in the ICU
Hospital‐acquired infections (HAIs) remain a leading cause of morbidity and mortality worldwide, particularly among critically ill patients. In the intensive care unit (ICU), where the risk is compounded by high device utilization, rigorous infection control measures are paramount. One intervention that has gained considerable attention is the implementation of daily bathing with 2% chlorhexidine gluconate (CHG). CHG is a broad‐spectrum antiseptic agent that acts primarily by disrupting bacterial cell membranes, causing leakage of intracellular components and eventual bacterial death [8].
An interventional study conducted in a 20-bed ICU demonstrated that switching from conventional soap-water bathing to daily 2% CHG bathing resulted in a significant reduction in overall HAI incidence rates. During the baseline period, the overall HAI rate was measured at 3.43 per 1000 patient-days, which dropped dramatically to 0.58 per 1000 patient-days during the intervention period. Although a slight rise to 1.59 per 1000 patient-days was observed in the post-intervention period, the beneficial effects of CHG remain significant. In addition, the incidence of CAUTIs and CLABSIs decreased markedly. Beyond the reduction in infection rates, routine CHG bathing was also associated with a reduction in the isolation of multidrug-resistant organisms from clinical specimens such as sputum, urine, and blood [8].
The success of CHG bathing in the ICU is likely multifactorial. First, CHG formulations appear to maintain residual antimicrobial activity for up to 24 hours, ensuring sustained reduction in skin microbial load. Second, its use in conjunction with an appropriate cleaning solution that does not contain interfering anionic surfactants optimizes its antiseptic effect. Third, standardized protocols and dedicated staff training ensure high adherence to the intervention, a critical factor in replicating these positive outcomes across other settings [8].
A summary table below highlights the incidence rates of key infections before and after implementation of 2% CHG bathing in the ICU:
| Infection Category | Baseline (2018) | Intervention (2019) | Post-Intervention (2020) |
|---|---|---|---|
| Overall HAI (per 1000 patient-days) | 3.43 (23 events) | 0.58 (4 events)* | 1.59 (11 events)# |
| Urinary Tract Infections (per 1000 catheter-days) | 2.09 (14 events) | 0.43 (3 events)* | 0.87 (6 events) |
| Bloodstream Infections (per 1000 line-days) | 1.19 (8 events) | 0.14 (1 event)* | 0.72 (5 events) |
*Table 3. Incidence rates of selected HAIs in the ICU before, during, and after the CHG bathing intervention (data adapted from [8]).
- *p < 0.05 compared with baseline.
These impressive reductions in infection rates reinforce the value of incorporating CHG bathing into standard ICU care protocols and provide a strong template for similar initiatives in other healthcare settings.
Emerging Threat of Carbapenem-Resistant Hypervirulent Klebsiella pneumoniae
Carbapenem-resistant hypervirulent Klebsiella pneumoniae (CR-hvKp) has emerged as a formidable threat in clinical microbiology with serious implications for public health. This pathogen is characterized by both an enhanced capacity for virulence and extensive resistance to carbapenem antibiotics—a combination that greatly complicates treatment decisions. A recent systematic review and meta-analysis synthesized available evidence on CR-hvKp isolates from various geographical regions across the globe. The analysis revealed that resistance rates were alarmingly high: for imipenem, resistance rates approached 49%; for meropenem, upwards of 53.2%; and for ertapenem, around 38.2% [4].
Beyond these quantitative metrics, the spread of CR-hvKp is mediated by the propagation of carbapenemase genes such as bla_VIM, bla_NDM, bla_OXA-48, and bla_KPC. In this meta-analysis, the pooled prevalence of these genes among hvKp isolates was estimated at 19.1% for bla_VIM, 22.0% for bla_NDM, 43.4% for bla_OXA-48, and 58.8% for bla_KPC. These findings suggest a heterogeneous and dynamic genetic landscape that favors rapid adaptation and spread across different regions. Such widespread dissemination signifies not only an increasing burden of resistant infections but also a dire need to implement robust infection control measures and to accelerate the development of novel antimicrobial therapies [4].
Table 4 below summarizes the pooled prevalence of carbapenem resistance among hvKp isolates and the distribution of key resistance genes as reported in the meta-analysis:
| Parameter | Pooled Prevalence (%) | Key Resistance Genes |
|---|---|---|
| Imipenem Resistance | 49.0 | |
| Meropenem Resistance | 53.2 | |
| Ertapenem Resistance | 38.2 | |
| bla_VIM Gene | 19.1 | bla_VIM |
| bla_NDM Gene | 22.0 | bla_NDM |
| bla_OXA-48 Gene | 43.4 | bla_OXA-48 |
| bla_KPC Gene | 58.8 | bla_KPC |
Table 4. Summary of carbapenem resistance parameters among hypervirulent K. pneumoniae isolates (data adapted from [4]).
The emergence of CR-hvKp underscores the necessity for ongoing global surveillance, stringent infection control practices, and the development of rapid diagnostic tools so as to contain the spread of these dangerous pathogens.
Leveraging Artificial Intelligence for Precision ADR Prediction
In the realm of pharmacovigilance, accurate and timely prediction of adverse drug reactions (ADRs) is crucial for optimizing patient safety. Traditional approaches have sometimes struggled to take into account the heterogeneous nature of patient data as well as the complex interplay of multiple medications. Recently, a novel scaling framework using heterogeneous graph neural networks (GNNs) has been introduced to predict patient-level ADRs with remarkable precision. This method, termed PreciseADR, aggregates data from diverse sources including patient demographics, previous medical history, medication records, and even drug-drug co-occurrence relationships. By integrating these heterogeneous inputs into a unified graph-based representation, the model successfully identifies patterns and predicts ADRs that might otherwise go undetected [5].
The architecture of the PreciseADR framework is composed of multiple layers that perform heterogeneous graph aggregation, along with patient node augmentation to integrate individual-level characteristics. A focal component of this architecture is the attention mechanism that assesses the importance of different nodes (such as drugs, diseases, and reported ADRs) when computing the overall risk for a given patient. This is complemented by the incorporation of contrastive learning techniques such as the InfoNCE loss that encourages the model to distinguish between similar and dissimilar representations. The combination of these advanced machine learning methodologies results in improved predictive performance relative to traditional deep learning or frequency-based models. In experiments, PreciseADR achieved a notable increase in the area under the curve (AUC) and improved Hit@10 metrics compared to baseline methods, highlighting the tremendous potential for AI in enhancing patient safety and guiding clinical decisions [5].
Advances in this domain not only demonstrate substantial improvements in predictive accuracy but also pave the way for personalized risk stratification for ADRs. By leveraging such precision models, healthcare providers can adjust therapies according to individual profiles, thereby reducing the incidence of severe drug reactions and ultimately enhancing the overall safety and quality of care.
Conclusion
Collectively, the research studies discussed in this article epitomize the multifaceted nature of modern advancements in clinical therapeutics and infection prevention. Trends in the utilization of glucose-lowering medications underscore an evolving paradigm in post-transplant diabetic care, with newer agents such as SGLT2 inhibitors and GLP-1 receptor agonists gradually supplanting traditional insulin therapy in select patient populations. Simultaneously, innovations in surgical stenting techniques have led to better outcomes in kidney transplantation, reducing complications and enhancing cost-efficiency.
Infection prevention measures in the ICU, particularly through the daily application of 2% chlorhexidine bathing, have resulted in substantial reductions in HAIs—a critical advancement given the high vulnerability of ICU patients to nosocomial infections. At the same time, the emergence of multidrug-resistant pathogens such as carbapenem-resistant hypervirulent Klebsiella pneumoniae serves as a stark reminder of the challenges that remain in combating infectious diseases globally.
Advances in data science, particularly through the use of heterogeneous graph neural networks for precision ADR prediction, offer a glimpse into the future of patient-centered care. These artificial intelligence-driven solutions not only improve the predictive performance of ADR risk but also support the customization of therapeutic strategies based on individual patient profiles. As healthcare systems aspire to become more precise and efficient, the convergence of clinical research, surgical innovation, advanced infection control, and AI-based solutions will be central to achieving optimal patient outcomes.
In conclusion, the integrated insights from these diverse studies foster a deeper understanding of contemporary clinical challenges while inspiring new approaches to treatment and prevention. By continuing to harness the power of cutting-edge methodologies and multidisciplinary research, clinicians and researchers can drive forward the evolution of healthcare, ultimately leading to better, safer, and more individualized patient care.
Frequently Asked Questions (FAQ)
What are the key trends in the use of glucose‐lowering medications among kidney transplant recipients?
Recent data indicate a decline in insulin usage and a corresponding increase in the utilization and initiation of newer agents such as SGLT2 inhibitors and GLP‐1 receptor agonists among kidney transplant recipients with type 2 diabetes. These trends are driven by emerging evidence of cardiovascular and renal benefits associated with the newer medications.
How does Double-J stenting improve outcomes in kidney transplantation compared to Single-J stenting?
Double‐J stenting, which remains in place for a longer duration (typically three weeks), significantly reduces urological complications, such as urinary leakage and ureteral strictures, compared to the more traditional externalized Single‐J stenting. Additionally, it facilitates earlier hospital discharge and reduces the need for extra procedures, thereby offering cost-effective benefits.
What impact does 2% chlorhexidine bathing have on healthcare-associated infections in the ICU?
Implementation of daily 2% chlorhexidine bathing in the ICU has been shown to substantially lower the incidence rates of HAIs, including catheter-associated urinary tract infections and central line-associated bloodstream infections. It achieves this by reducing the skin microbial load and sustaining antimicrobial activity for up to 24 hours.
Why is carbapenem-resistant hypervirulent Klebsiella pneumoniae such a significant threat?
Carbapenem-resistant hypervirulent K. pneumoniae is problematic because it combines both high virulence and extensive resistance to carbapenem antibiotics. The organism often carries multiple carbapenemase genes, making it difficult to treat and control. Its widespread dissemination across different geographical regions further exacerbates the public health risk.
How do heterogeneous graph neural networks improve ADR prediction?
Heterogeneous graph neural networks such as the PreciseADR framework integrate diverse data sources—including patient demographics, medical history, and drug-drug interactions—into a unified graph representation. This enables the model to capture complex relationships and improve the prediction of adverse drug reactions at the individual level, thereby allowing for personalized treatment strategies.
Where can I find more detailed information or the original studies referenced in this article?
All references cited in this article are listed in the Reference section at the end, with full unbroken URL links available for each source.
References
- Decoding machine learning in nursing research: A scoping review of effective algorithms. (2025). Journal of Nursing Scholarship. https://pubmed.ncbi.nlm.nih.gov/11771615/
- A rare case of pyelonephritis with methicillin-resistant Staphylococcus aureus (MRSA) bacteremia complicated by renal vein thrombosis. (2025). Cureus. https://doi.org/10.7759/cureus.76832
- Sacral and implantable tibial neuromodulation for the management of overactive bladder: A systematic review and meta-analysis. (2025). Advances in Therapy. https://doi.org/10.1007/s12325-024-03019-0
- Systematic review and meta-analysis on the carbapenem-resistant hypervirulent Klebsiella pneumoniae isolates. (2025). BMC Pharmacology & Toxicology. https://doi.org/10.1186/s40360-025-00857-8
- Precision adverse drug reactions prediction with heterogeneous graph neural network. (2025). Journal of Nursing Scholarship. https://pubmed.ncbi.nlm.nih.gov/11775569/
- Utilization trends of glucose-lowering medications among adult kidney transplant recipients with type 2 diabetes in the United States. (2025). Journal of Clinical Medicine. https://doi.org/10.3390/jcm14020651
- Long-term Double-J stenting is superior to short-term Single-J stenting in kidney transplantation. (2025). PLOS ONE. https://doi.org/10.1371/journal.pone.0317991
- Implementation of 2% chlorhexidine bathing to reduce healthcare-associated infections among patients in the intensive care unit. (2025). Microorganisms. https://doi.org/10.3390/microorganisms13010065