Table of Contents
Defining Urinary Tract Infections (UTIs)
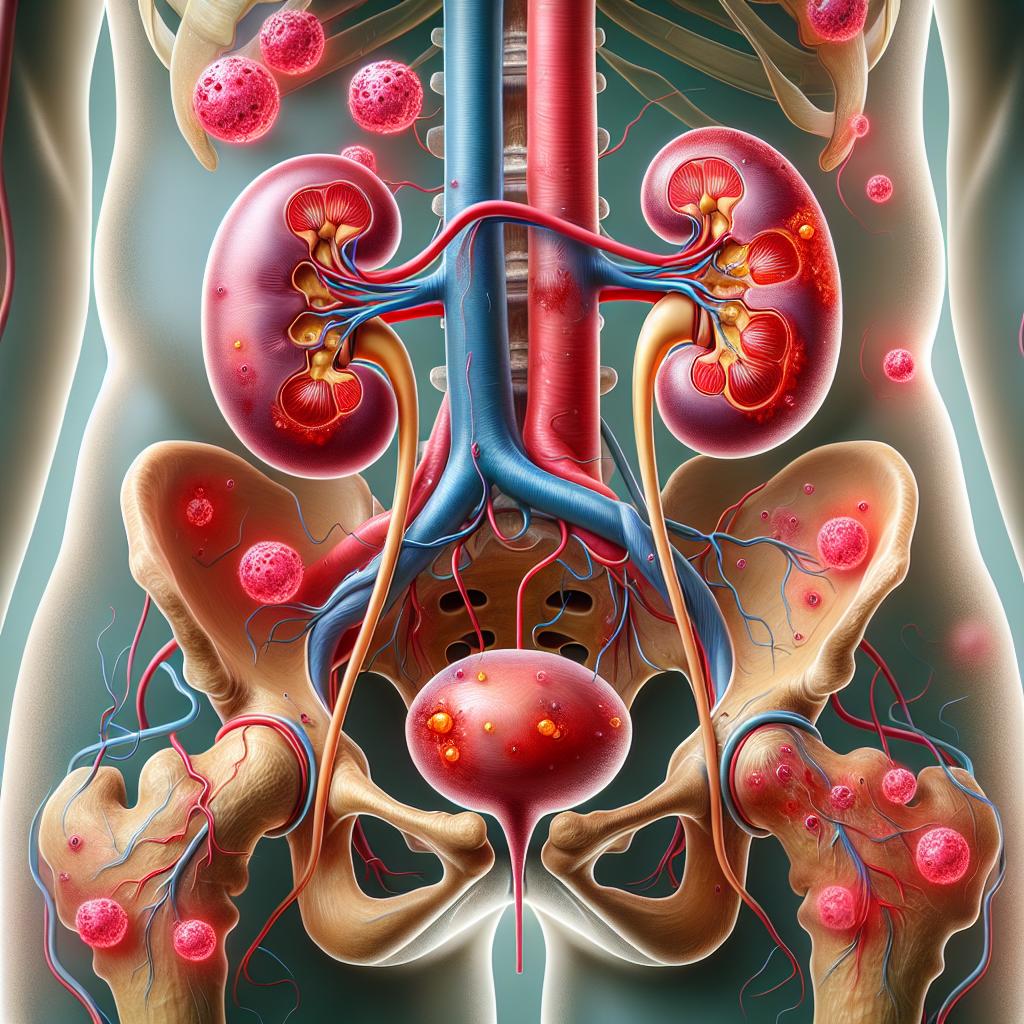
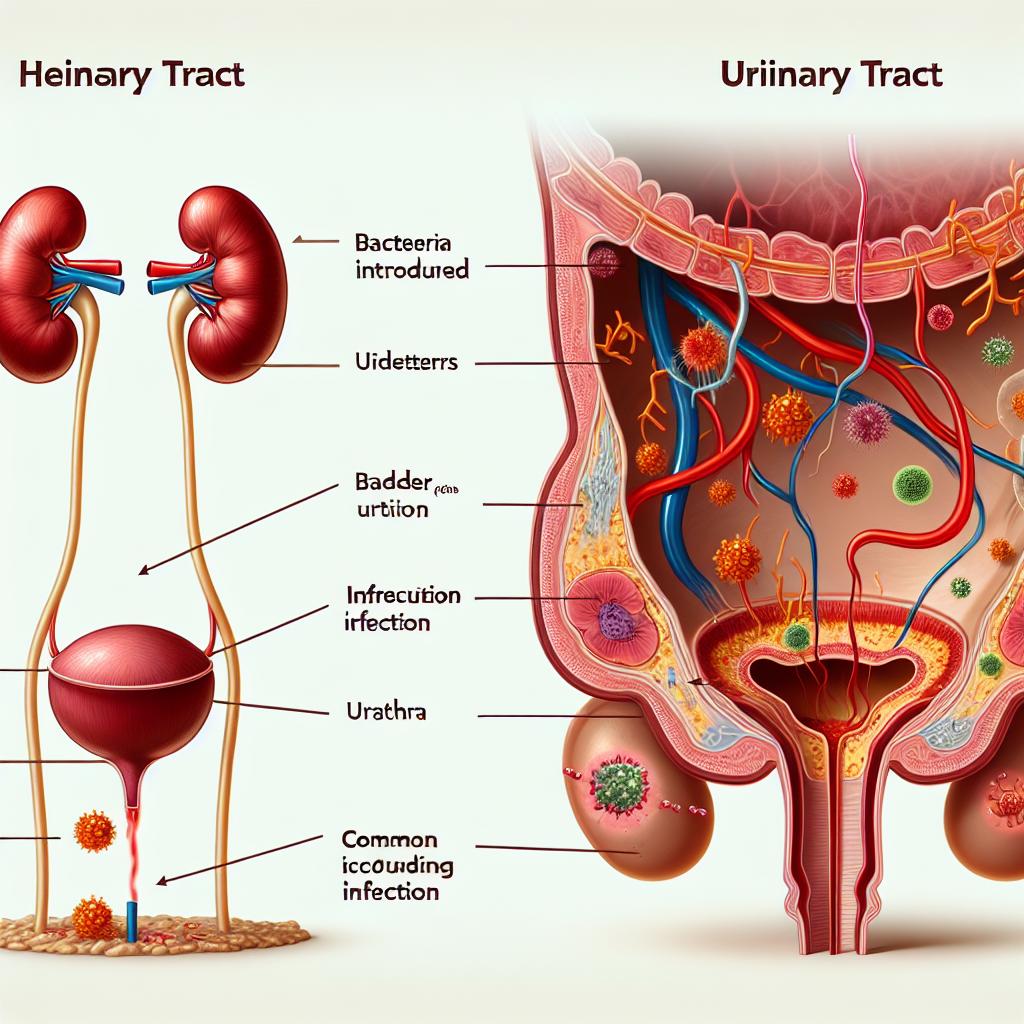
Urinary tract infections (UTIs) are infections that occur in any part of the urinary system, which includes the kidneys, ureters, bladder, and urethra. UTIs are among the most common bacterial infections, affecting millions of people annually. They can be classified into two major categories: uncomplicated and complicated UTIs. Uncomplicated Utis occur in healthy individuals with normal urinary tracts, while complicated UTIs arise in individuals with anatomical or functional abnormalities of the urinary tract. The primary causative agents of UTIs are bacteria, with Escherichia coli being the most prevalent pathogen responsible for approximately 80-90% of cases (Wagan et al., 2025).
The symptoms of UTIs can range from mild to severe and may include frequent urination, burning sensation during urination, cloudy urine, and pelvic pain. In some cases, UTIs can lead to more serious conditions if the bacteria spread to the kidneys, resulting in a kidney infection, also known as pyelonephritis. The recognition of UTIs is critical for effective management and treatment, and it often relies on clinical symptoms, urinalysis, and culture tests to confirm the diagnosis (Wagan et al., 2025).
Understanding Kidney Infections and Their Causes
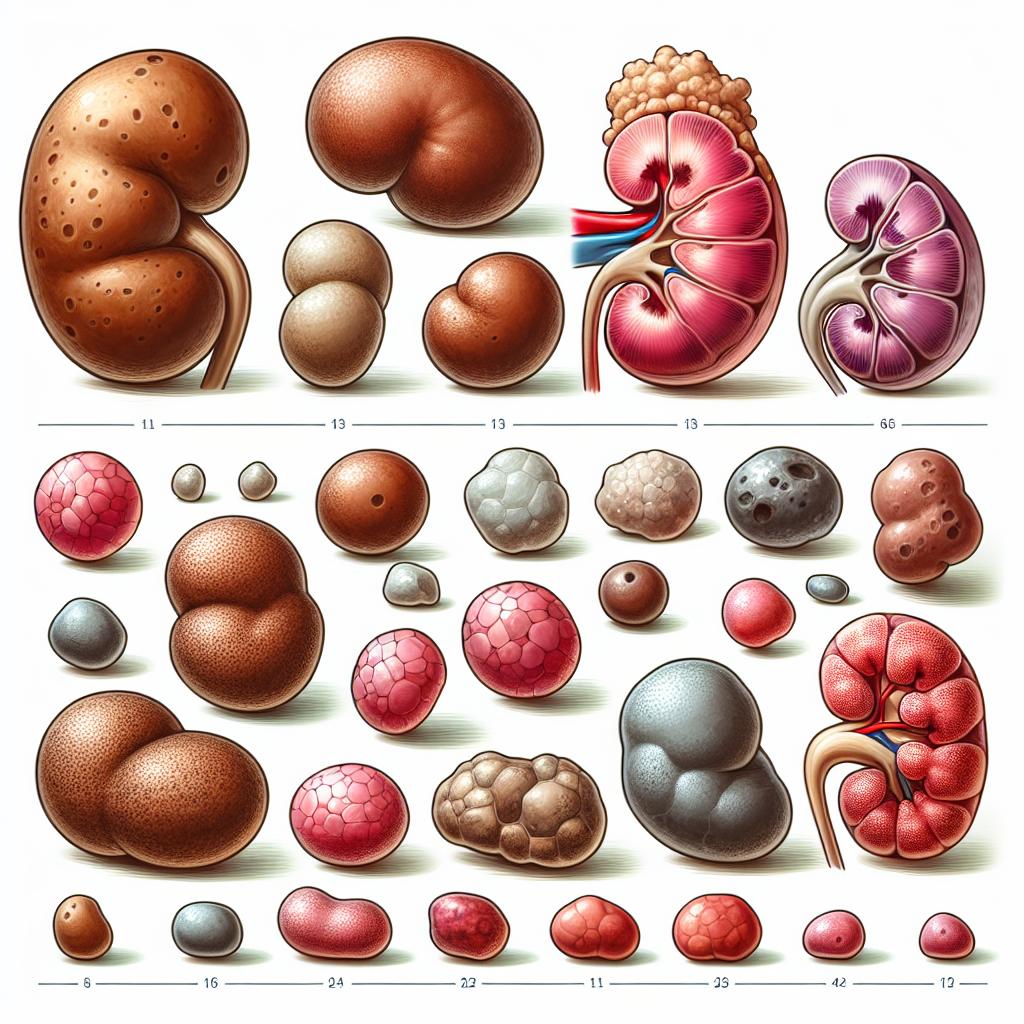
Kidney infections, or pyelonephritis, are a type of UTI that specifically affects the kidneys. They can arise when bacteria from the bladder ascend through the ureters to the kidneys. This condition is often more serious than a standard UTI and can lead to severe complications if not treated promptly. Factors contributing to the development of kidney infections include urinary obstructions, kidney stones, and conditions that impair the immune system (Kim et al., 2025).
The causes of kidney infections are similar to those of UTIs, predominantly involving E. coli. However, other bacteria such as Klebsiella, Proteus, and Enterobacter can also be responsible. Risk factors for kidney infections include female gender, urinary tract abnormalities, diabetes, and a history of urinary tract infections. Symptoms of kidney infections can include fever, chills, nausea, vomiting, and flank pain, which are often more severe than those experienced with lower urinary tract infections (Wagan et al., 2025).
Symptoms That Differentiate UTI from Kidney Infection
While UTIs and kidney infections share some overlapping symptoms, certain clinical features can help differentiate between the two. UTIs primarily present with lower urinary symptoms, including:
- Frequent and urgent need to urinate
- Burning sensation while urinating
- Cloudy or strong-smelling urine
- Pelvic or lower abdominal pain
In contrast, kidney infections often present with additional systemic symptoms, which can include:
- High fever (often >101°F or 38.3°C)
- Chills and rigors
- Flank pain or back pain (located on one side of the body)
- Nausea and vomiting
- Fatigue
The presence of systemic symptoms, particularly fever and flank pain, suggests a more severe infection that may require immediate medical attention. In cases where kidney infections progress, patients may develop sepsis, characterized by a systemic inflammatory response to infection (Kim et al., 2025).
Diagnostic Methods for UTI versus Kidney Infection
Accurate diagnosis of UTIs and kidney infections is crucial for effective treatment. Diagnostic methods typically involve:
- Urinalysis: A standard test for both UTIs and kidney infections. It assesses urine for signs of infection such as the presence of white blood cells, red blood cells, and bacteria.
- Urine Culture: This test identifies specific bacteria responsible for the infection and determines their antibiotic sensitivity.
- Imaging Studies: In cases of suspected kidney infections, imaging studies such as ultrasound or CT scans may be utilized to identify complications like kidney stones or abscesses.
The distinction between a simple UTI and a kidney infection often hinges on the presence of systemic symptoms, and healthcare providers may implement additional tests, such as blood cultures and inflammatory markers, to assess the extent of the infection and guide treatment decisions (Kim et al., 2025).
Treatment Approaches for UTI and Kidney Infections
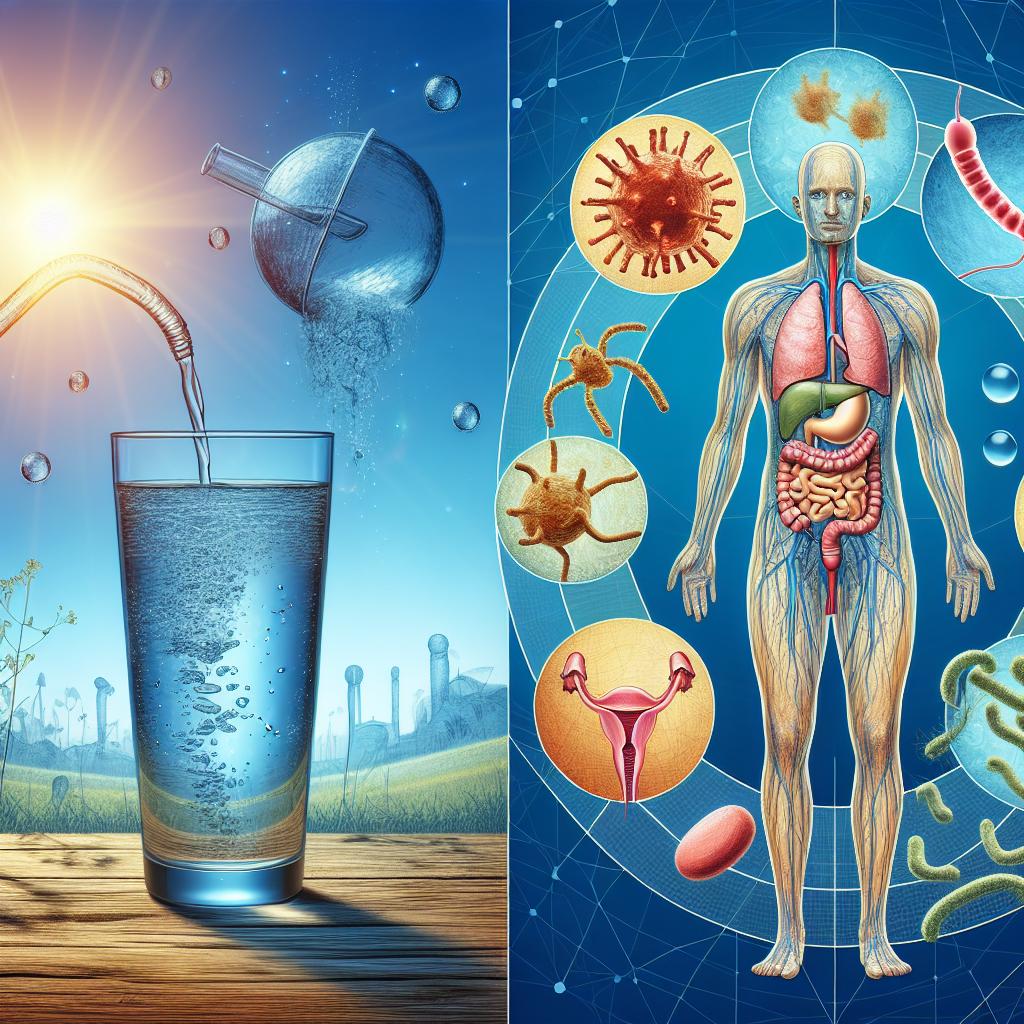
The treatment of UTIs typically involves the use of antibiotics, with the choice of medication depending on the bacteria identified in culture and the patient’s medical history. Commonly prescribed antibiotics for uncomplicated UTIs include trimethoprim-sulfamethoxazole, nitrofurantoin, and fosfomycin. Treatment durations can vary, with uncomplicated cases often requiring 3 to 7 days of therapy (Wagan et al., 2025).
In contrast, kidney infections often necessitate more aggressive treatment. Patients may require hospitalization, especially if they present with severe symptoms or complications. Intravenous (IV) antibiotics are commonly administered initially, transitioning to oral antibiotics once the patient shows improvement. The typical duration of treatment for kidney infections ranges from 10 to 14 days. Additionally, supportive care may include hydration and pain management (Kim et al., 2025).
Summary Table: Comparison of UTI and Kidney Infection
| Feature | UTI | Kidney Infection |
|---|---|---|
| Primary Symptoms | Dysuria, frequency, urgency | Flank pain, fever, chills |
| Causative Organisms | Mostly E. coli | E. coli, Klebsiella, others |
| Diagnostic Methods | Urinalysis, urine culture | Urinalysis, urine culture, imaging |
| Treatment | Oral antibiotics | IV antibiotics, possible hospitalization |
| Duration of Treatment | 3-7 days | 10-14 days |
FAQ
What are the common causes of UTIs?
The most common cause of UTIs is Escherichia coli (E. coli). Other bacteria, such as Klebsiella and Proteus, can also cause UTIs.
How are kidney infections diagnosed?
Kidney infections are diagnosed through urinalysis, urine culture, and sometimes imaging studies like ultrasound or CT scans.
Can a UTI lead to a kidney infection?
Yes, if a UTI is left untreated, the bacteria can ascend to the kidneys, causing a kidney infection.
What are the risk factors for developing a kidney infection?
Risk factors include female gender, urinary tract abnormalities, kidney stones, diabetes, and a history of UTIs.
How are UTIs typically treated?
UTIs are usually treated with antibiotics. The choice of antibiotic depends on the bacteria identified in the urine culture.
References
-
Kim, T., Son, E., So, M. W., Jeon, D., Yeo, H. J., Lee, S. E., & Yun, S. (2025). Predicting Healthcare-Associated Infection in Patients with Pneumonia via QuantiFERON®-Monitoring. Infection and Drug Resistance. https://doi.org/10.2147/IDR.S499765
-
Wagan, A. A., Paras, P., & Faris, A. N. (2025). Lower urinary tract symptoms and hematuria in Rheumatoid arthritis (LUTH-RA) study. Pakistan Journal of Medical Sciences. https://doi.org/10.12669/pjms.41.3.8316