Table of Contents
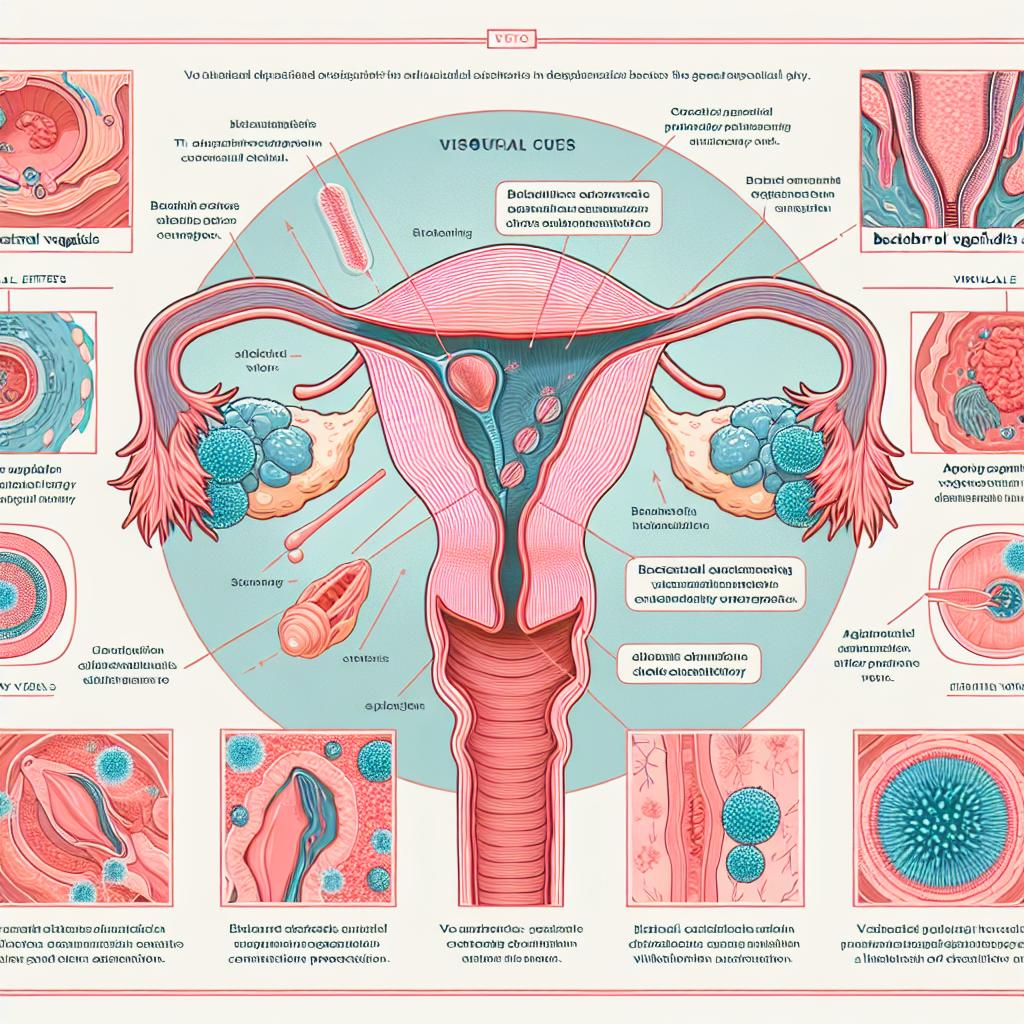
Overview of Bacterial Vaginosis (BV) and Urinary Tract Infections (UTIs)
Bacterial vaginosis (BV) and urinary tract infections (UTIs) are two common conditions affecting women’s reproductive health, often causing discomfort and distress. BV is characterized by an imbalance in the normal bacterial flora of the vagina, leading to symptoms such as unusual discharge and odor. It is the most prevalent cause of vaginal discharge in women of reproductive age, affecting nearly 30% of women in this demographic (Nicolle et al., 2019).
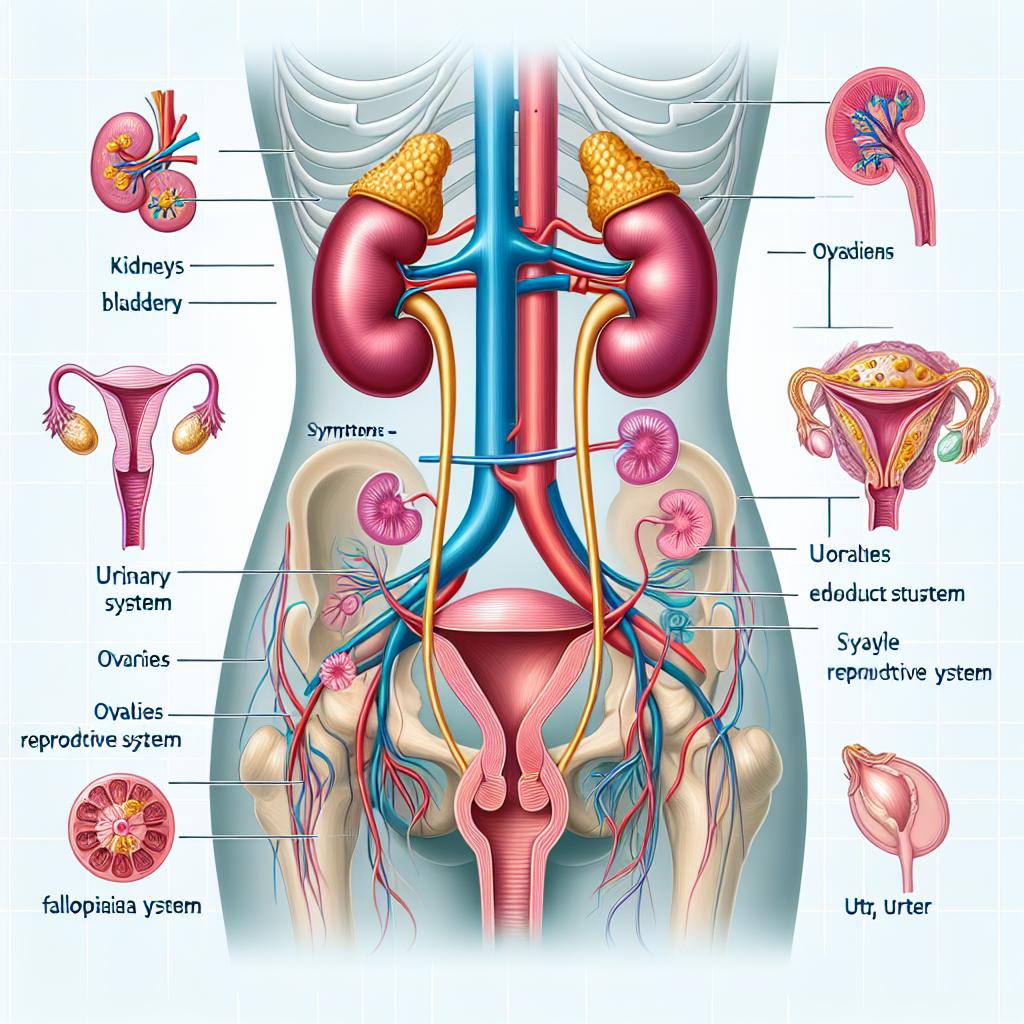
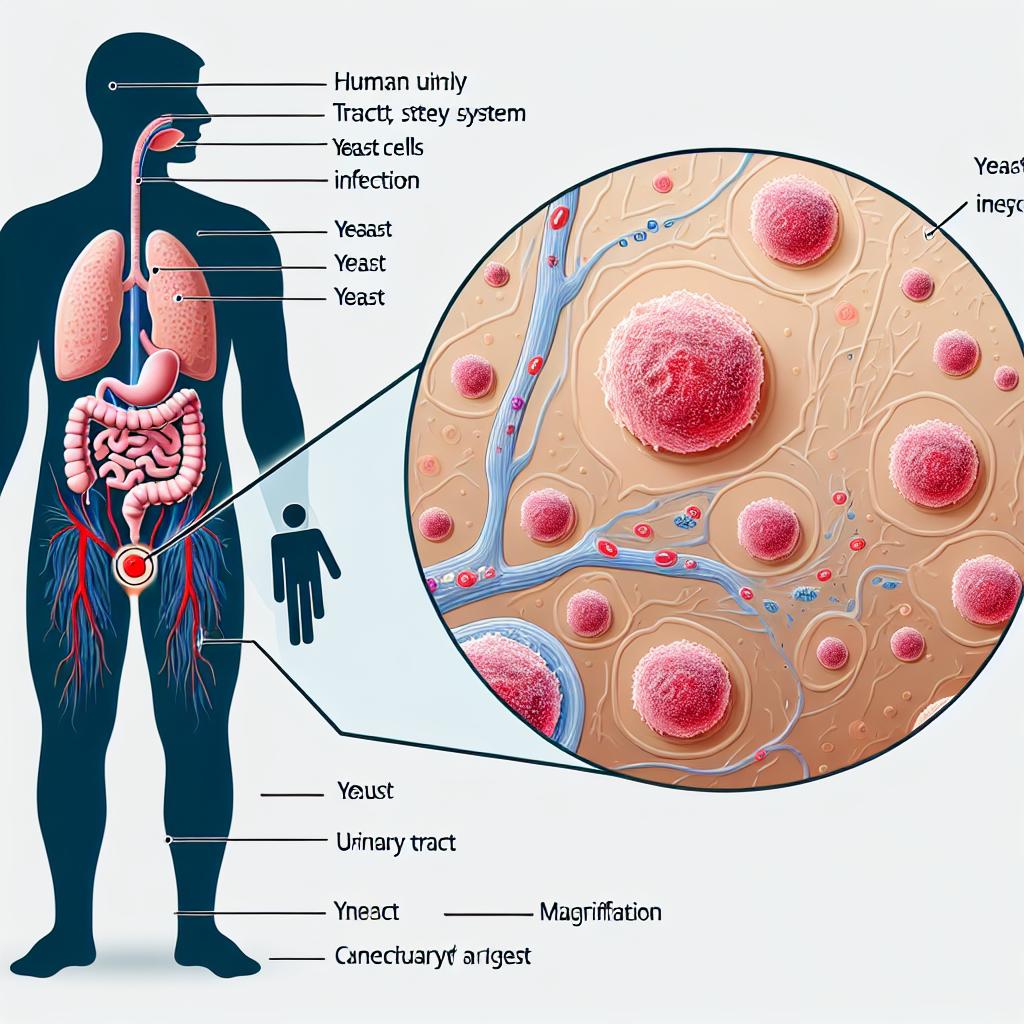
On the other hand, UTIs are infections that can affect any part of the urinary system, including the bladder, ureters, kidneys, and urethra, with the bladder being the most commonly affected site. UTIs disproportionately affect women, with studies indicating that nearly 60% of women will experience at least one UTI in their lifetime, and the recurrence rate is high, with 20-30% of women experiencing recurrent infections (Hooton, 2012).
Understanding the key differences between BV and UTIs is crucial for effective diagnosis and treatment. While both conditions may present with similar symptoms, they require distinct management strategies.
Common Symptoms of Bacterial Vaginosis and Urinary Tract Infections
Symptoms of Bacterial Vaginosis (BV)
The symptoms of BV can vary, but they often include:
- Unusual Vaginal Discharge: A thin, grayish-white discharge that may have a fishy odor, particularly after intercourse.
- Vaginal Irritation: Some women may experience itching or irritation in the vaginal area.
- Odor: A strong, fishy smell that becomes more noticeable after sexual intercourse or during menstruation.
- Asymptomatic Cases: Many women with BV do not experience any noticeable symptoms.
Symptoms of Urinary Tract Infections (UTIs)
The symptoms of UTIs are primarily related to urinary changes and may include:
- Dysuria: A burning sensation during urination.
- Increased Urinary Frequency: A frequent urge to urinate, often producing small amounts of urine.
- Urgency: A sudden and strong need to urinate.
- Suprapubic Pain: Discomfort or pain in the lower abdomen.
- Hematuria: Blood in the urine, which may appear pink or red.
- Flank Pain: Pain in the back or side, indicating a potential kidney infection.
Understanding these symptoms helps differentiate between BV and UTIs, guiding healthcare professionals toward appropriate treatment options.
Diagnosis Methods for Bacterial Vaginosis and Urinary Tract Infections
Diagnosis of Bacterial Vaginosis (BV)
Diagnosis of BV is typically made based on the clinical criteria known as Amsel’s criteria, which include:
- Vaginal pH: A vaginal pH greater than 4.5.
- Microscopic Examination: The presence of clue cells (vaginal epithelial cells covered with bacteria) during a wet mount examination.
- Whiff Test: A fishy odor released upon the addition of KOH to the vaginal discharge.
- Discharge Characteristics: A thin, grayish discharge.
Diagnosis of Urinary Tract Infections (UTIs)
Diagnosis of UTIs often involves:
- Urinalysis: A dipstick test to check for nitrites and leukocyte esterase, which indicate infection.
- Urine Culture: A more definitive test that identifies the specific bacteria causing the infection and determines antibiotic susceptibility.
- Clinical Symptoms: A history of urinary symptoms, such as dysuria and increased urinary frequency, aids in diagnosis.
Early diagnosis of both conditions is critical, as it allows for timely intervention and can prevent complications.
Treatment Options for Bacterial Vaginosis and Urinary Tract Infections
Treatment for Bacterial Vaginosis (BV)
Treatment for BV typically includes:
- Antibiotics: Metronidazole or clindamycin are commonly prescribed, either orally or as a vaginal gel. These antibiotics help restore the normal balance of bacteria in the vagina.
- Probiotics: Some studies suggest that probiotics may help restore vaginal flora, although more research is needed to confirm their effectiveness.
Treatment for Urinary Tract Infections (UTIs)
Treatment for UTIs generally involves:
- Antibiotics: Trimethoprim-sulfamethoxazole, nitrofurantoin, and fosfomycin are common first-line treatment options, depending on local resistance patterns.
- Hydration: Drinking plenty of fluids can help flush bacteria from the urinary system.
- Pain Relief: Over-the-counter pain relievers like phenazopyridine may help alleviate discomfort.
It is essential to complete the entire course of antibiotics for both BV and UTIs, even if symptoms resolve early, to prevent recurrence and resistance.
Prevention Strategies for Bacterial Vaginosis and Urinary Tract Infections
Prevention of Bacterial Vaginosis (BV)
Preventive measures for BV include:
- Maintain Vaginal Health: Avoid douching or using scented products in the genital area, which can disrupt the natural flora.
- Safe Sex Practices: Use condoms to reduce the risk of introducing new bacteria.
- Probiotics: Consider probiotics or yogurt with live cultures to help maintain a healthy vaginal microbiome.
Prevention of Urinary Tract Infections (UTIs)
To prevent UTIs, individuals can:
- Stay Hydrated: Drink plenty of water to help flush out the urinary system.
- Urinate After Intercourse: This can help eliminate bacteria that may have been introduced during sex.
- Avoid Irritants: Limit the use of feminine hygiene products that could irritate the urethra.
- Cranberry Products: Some studies suggest that cranberry juice or supplements may reduce the risk of recurrent UTIs.
Implementing these strategies can significantly lower the risk of developing BV and UTIs.
FAQ Section
What are the main differences between BV and UTI?
BV is a vaginal condition resulting from an imbalance of bacteria, while UTIs affect the urinary system, often caused by bacteria entering the bladder. Symptoms, causes, and treatments differ significantly between the two.
Can BV lead to UTIs?
Yes, BV may increase the risk of developing UTIs due to the changes in vaginal flora that can facilitate bacterial entry into the urinary tract.
How are BV and UTIs diagnosed?
BV is diagnosed through clinical criteria such as vaginal pH and microscopic examination, while UTIs are diagnosed through urinalysis and urine culture.
What are the best treatments for BV and UTIs?
BV is treated with antibiotics like metronidazole, whereas UTIs are commonly treated with antibiotics such as nitrofurantoin or trimethoprim-sulfamethoxazole.
How can I prevent BV and UTIs?
Maintaining proper hygiene, staying hydrated, and avoiding irritants can help prevent both conditions.
References
- Nicolle, L. E., et al. (2019). Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clinical Infectious Diseases
- Hooton, T. M. (2012). Urinary tract infections: The importance of an effective diagnosis and management. Nature Reviews Urology, 9(10), 533-543