Table of Contents
What is UTI and How Does it Relate to Blood in Urine?
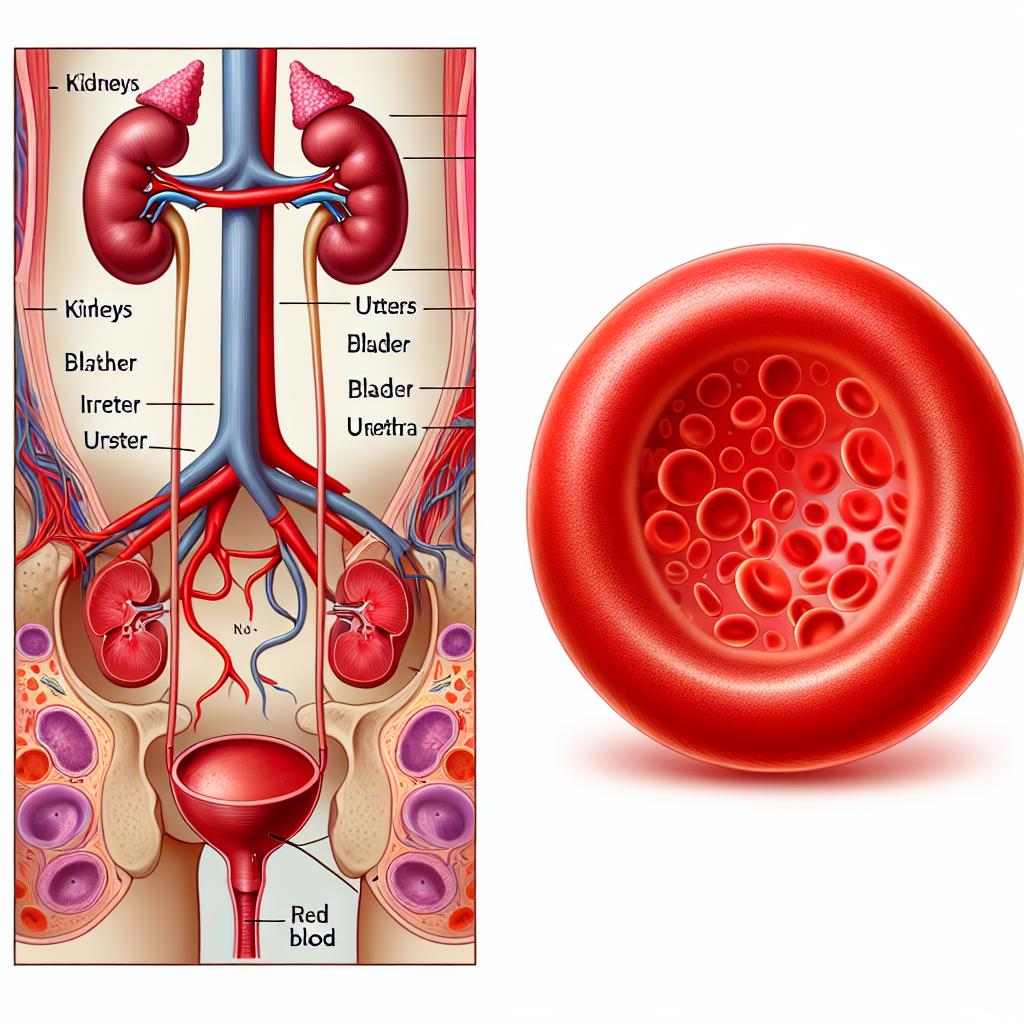
A urinary tract infection (UTI) occurs when bacteria enter the urinary tract, leading to inflammation and infection. UTIs can affect any part of the urinary system, including the kidneys, ureters, bladder, and urethra. The presence of blood in urine, known as hematuria, can often accompany a UTI and may indicate an underlying complication or severity of the infection.
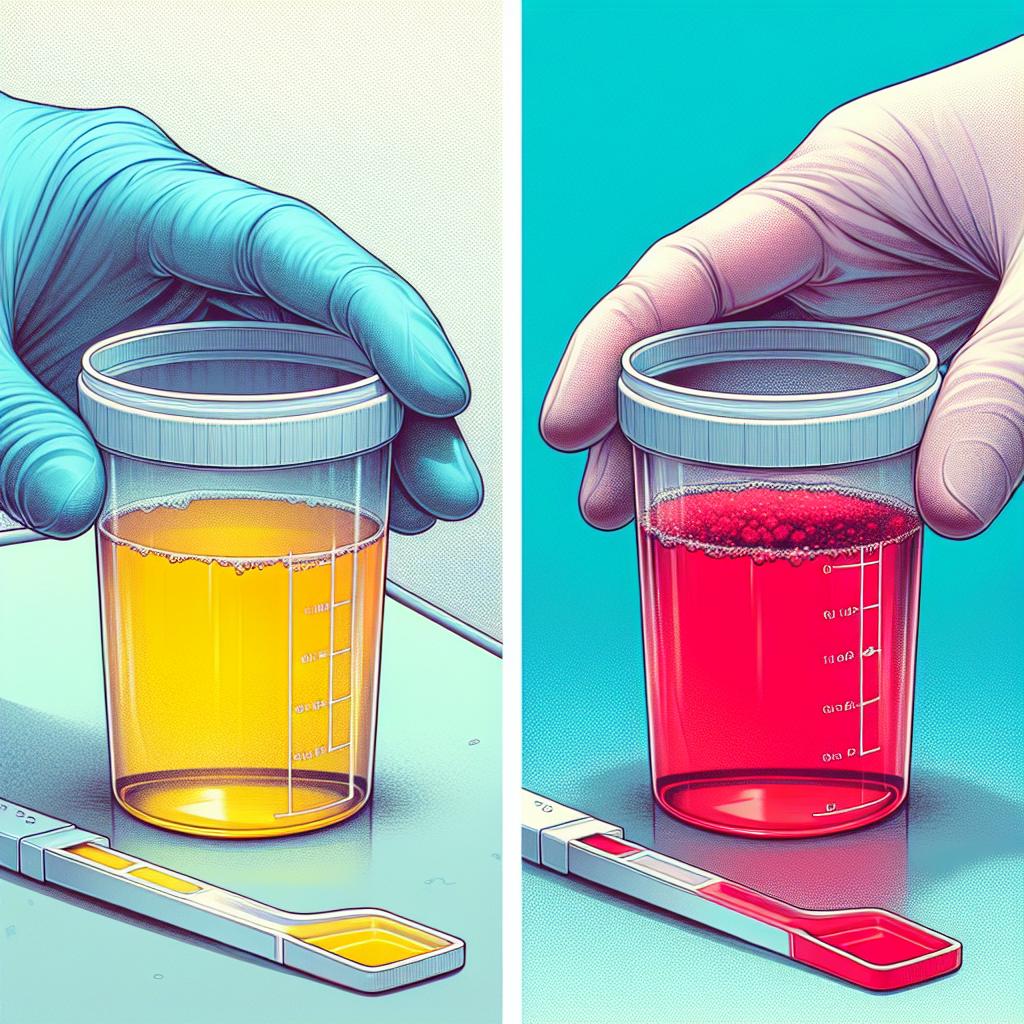
Hematuria can manifest as two types: gross hematuria, where blood is visible to the naked eye, and microscopic hematuria, where blood is only detectable through urine tests. Understanding the relationship between UTIs and hematuria is crucial, as it may signal the need for more aggressive treatment or investigation into other potential causes of bleeding, such as kidney stones or tumors.
Common Symptoms of UTI with Blood in Urine
The symptoms of a UTI can vary significantly depending on the severity and the specific area of the urinary tract affected. Common symptoms associated with UTIs include:
- A strong, persistent urge to urinate
- A burning sensation during urination
- Frequent urination with only small amounts of urine being passed
- Cloudy or strong-smelling urine
- Pelvic pain or pressure
- Fatigue and malaise
When hematuria is present, additional signs may include visible blood in the urine or a pink, red, or cola-colored appearance of the urine. This symptom can be alarming and often prompts individuals to seek immediate medical attention.
Causes of Blood in Urine Associated with UTIs
Several factors can contribute to the presence of blood in urine during a UTI. These include:
- Infection Severity: Increased inflammation and damage to the urinary tract lining caused by bacterial infection can lead to bleeding.
- Urinary Tract Obstruction: Kidney stones or other obstructions can irritate the urinary tract, causing bleeding alongside infection.
- Trauma: In some cases, trauma to the urinary tract during catheterization or strenuous activities can cause blood to appear in the urine.
- Underlying Conditions: Conditions such as glomerulonephritis or tumors can also lead to hematuria, complicating the clinical picture of a UTI.
It is imperative to conduct thorough evaluations to determine the exact etiology of hematuria, especially in cases with recurrent infections or significant blood presence.
Diagnosing UTI: Tests and Procedures for Blood in Urine
Diagnosing a UTI with associated hematuria typically involves several tests and procedures:
- Urinalysis: A routine urinalysis can reveal the presence of bacteria, blood, and white blood cells in the urine, which are indicative of infection.
- Urine Culture: A urine culture helps identify the specific bacteria causing the infection, which aids in tailoring antibiotic therapy effectively.
- Imaging Studies: In cases of recurrent UTIs or significant hematuria, imaging studies such as ultrasound or CT scans may be warranted to rule out anatomical abnormalities, stones, or tumors.
- Cystoscopy: This procedure involves inserting a small camera into the bladder through the urethra to visually inspect for abnormalities.
Table 1 summarizes common diagnostic tests and their purposes.
| Test | Purpose |
|---|---|
| Urinalysis | Detects infection markers (bacteria, blood, WBCs) |
| Urine Culture | Identifies specific pathogens and their antibiotic sensitivities |
| Imaging Studies | Visualizes urinary tract structures and identifies obstructions or tumors |
| Cystoscopy | Direct visualization of the bladder for abnormalities |
Effective Treatments for UTI and Managing Blood in Urine
Treatment of UTIs typically involves antibiotics, with the choice of antibiotic guided by urine culture results. Common antibiotics for urinary tract infections include:
- Nitrofurantoin: Effective for uncomplicated UTIs.
- Trimethoprim-sulfamethoxazole: Commonly used, but resistance is increasing.
- Fosfomycin: A single-dose option for uncomplicated UTIs.
In cases where hematuria is significant or recurrent, management strategies may include:
- Hydration: Increasing fluid intake can help flush out the urinary system and may reduce irritation.
- Pain Management: Analgesics such as phenazopyridine can alleviate discomfort associated with UTIs.
- Preventive Measures: Strategies may involve lifestyle modifications, such as proper hygiene, urinating after intercourse, and possibly prophylactic antibiotics for recurrent cases.
In more complicated cases, such as those involving kidney stones or other structural issues, surgical intervention may be necessary to address the underlying cause of hematuria.
FAQ
What should I do if I suspect I have a UTI?
If you experience symptoms of a UTI, such as painful urination, frequent urge to urinate, or blood in your urine, it is essential to consult a healthcare provider for evaluation and treatment.
Can a UTI cause serious complications?
Yes, untreated UTIs can lead to serious complications, including kidney infections (pyelonephritis), sepsis, and permanent kidney damage. Prompt treatment is crucial.
How can I prevent UTIs?
Preventive measures include drinking plenty of fluids, practicing good hygiene, urinating before and after sexual intercourse, and avoiding irritants such as harsh soaps and douches.
Is blood in urine always a sign of a UTI?
No, while hematuria can occur with UTIs, it can also be caused by other conditions such as kidney stones, glomerulonephritis, or tumors. It’s important to seek medical advice for proper diagnosis.
References
-
Hoyt, B. M., Messacar, K., Sick-Samuels, A. C., Jaggi, P., Hamilton, S. L., & Parker, S. K. (2024). Opportunities for collaboration: the synergy between antimicrobial and diagnostic stewardship in pediatrics. Antimicrobial Stewardship & Healthcare Epidemiology. https://doi.org/10.1017/ash.2024.464
-
Pant, P., Chihara, S., Krishnamoorthy, V., Treggiari, M. M., Messina, J. A., Privratsky, J. R., & Ohnuma, T. (2025). Association of causative pathogens with acute kidney injury in adult patients with community-onset sepsis. Critical Care Explorations
-
Popova, E., Tkachev, S., Shapoval, A., Karpenko, A., Lee, Y., Chislov, P., Ershov, B., & Galechyan, G. (2025). Kidney stones as minerals: How methods from geology could inform urolithiasis treatment. Journal of Clinical Medicine. https://doi.org/10.3390/jcm14030997
-
Raghunathan, K., et al. (2024). Pediatric kidney transplant recipients are at an increased risk for dysbiosis. Frontiers in Microbiology. https://doi.org/10.3389/fmicb.2025.1499813