Table of Contents
Introduction to Urine Nitrite and Its Significance
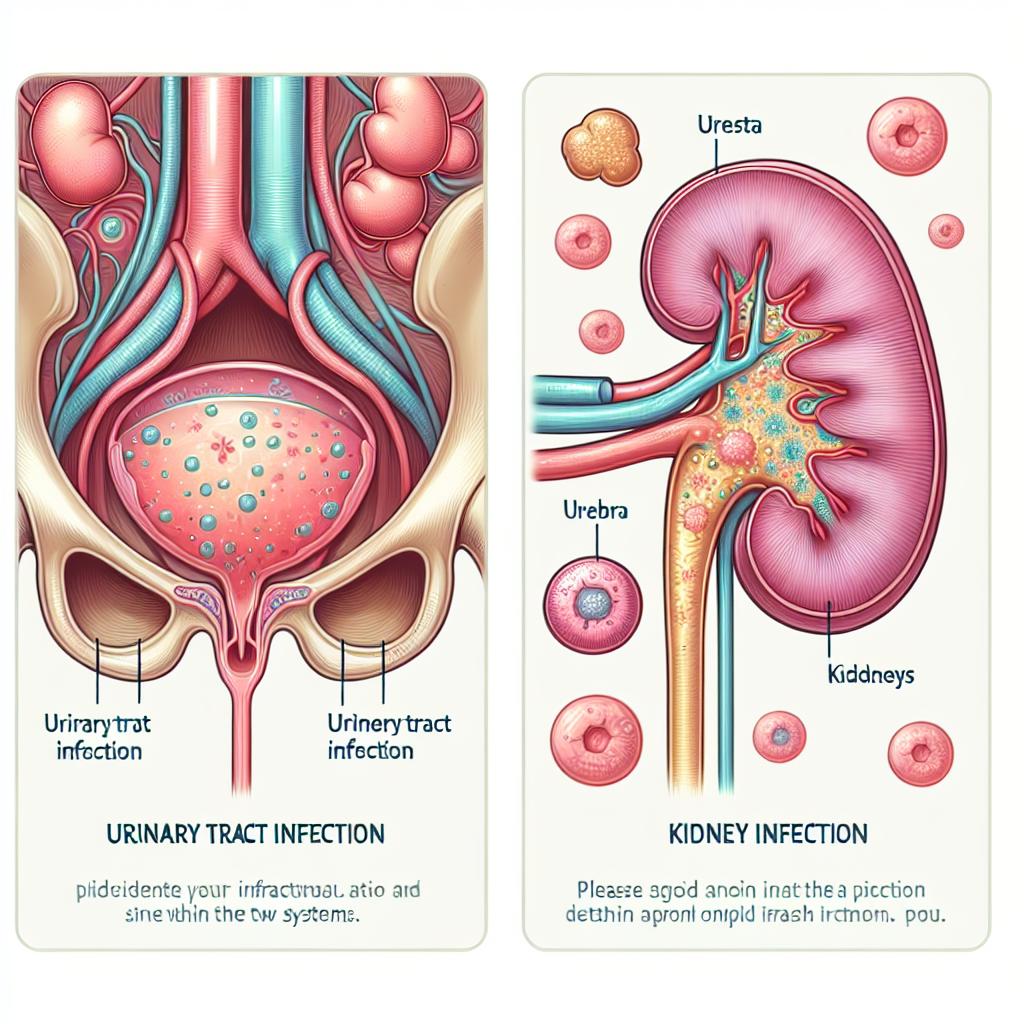
Urine nitrite is a critical biomarker in assessing urinary tract health, particularly in diagnosing urinary tract infections (UTIs). This compound forms when bacteria that reduce nitrate to nitrite are present in the urinary tract. The presence of nitrites can quickly indicate an ongoing infection, thus serving as an essential diagnostic tool for healthcare providers. Understanding the implications of urine nitrite levels in patients can enhance clinical outcomes and streamline treatment processes.
Urinary tract infections are among the most common bacterial infections affecting individuals, significantly impacting quality of life. Given the high prevalence of these infections, the role of urine nitrite as a diagnostic marker is increasingly vital. It not only assists in confirming the diagnosis of a UTI but also helps in differentiating bacterial infections from other urinary conditions that may mimic UTI symptoms.
Role of Urine Nitrite in Diagnosing Urinary Tract Infections
Clinical guidelines widely recognize urine nitrite testing as part of the diagnostic process for UTIs. The conversion of nitrate to nitrite typically occurs in the presence of specific bacteria, such as Escherichia coli, which are commonly associated with UTIs. The ability to detect nitrites in urine samples provides a rapid and cost-effective method for diagnosing infections, thereby facilitating timely treatment (Ainslie et al., 2016).
A systematic review highlighted the accuracy of pyuria and nitrite tests in diagnosing pediatric UTIs, emphasizing the reliability of urine nitrite as a diagnostic marker (Ainslie et al., 2016). The nitrite test is especially useful in outpatient settings where quick decision-making is crucial.
The sensitivity and specificity of urine nitrite tests are influenced by various factors, including the duration of urinary retention, diet, and hydration levels. For instance, a patient with a high nitrate diet may yield a false-positive result if urine is not retained long enough for bacteria to convert nitrate to nitrite (Leacy et al., 2020). This underscores the importance of understanding the patient’s context when interpreting test results.
Understanding the Mechanisms Behind Urine Nitrite Formation
The formation of urine nitrite involves a biochemical process where bacteria in the urinary tract convert nitrates, largely derived from dietary sources, into nitrites. This process is facilitated by bacterial enzymes known as nitrate reductases. The efficiency of this conversion can vary based on the type of bacteria present, the patient’s hydration status, and the timing of the urine sample collection.
In general, nitrates are abundant in vegetables such as spinach, beets, and celery. When these foods are consumed, nitrates are absorbed into the bloodstream and subsequently filtered by the kidneys into the urine. If bacteria capable of reducing nitrate to nitrite are present, nitrites accumulate in the urine, which can then be detected by dipstick assays or other laboratory methods.
Moreover, the presence of nitrites is not exclusive to UTIs; it can also indicate other urinary pathologies. Understanding the specific bacterial species responsible for nitrite production can provide deeper insights into the infection’s nature and guide appropriate antibiotic therapy (Leacy et al., 2020).
Factors Influencing Urine Nitrite Levels in Patients
Several factors influence urine nitrite levels, including hydration status, diet, and the presence of bacteria. Individuals with inadequate fluid intake may have concentrated urine, leading to higher concentrations of nitrites. Conversely, excessive fluid intake can dilute urine, potentially resulting in lower nitrite concentrations.
Diet plays a substantial role in determining nitrate levels in urine. Consuming a diet rich in nitrates can enhance nitrite levels, while a low-nitrate diet may lead to undetectable nitrites even in the presence of a UTI. Furthermore, certain medications and supplements may interfere with urine chemistry, affecting nitrite test results.
The time of day and the length of time urine is retained in the bladder also play critical roles. Nitrites are usually detectable in urine that has been held for a few hours, allowing sufficient time for bacterial action on dietary nitrates. Hence, practitioners often advise patients to collect midstream urine samples for accurate testing (Leacy et al., 2020).
Clinical Implications of Urine Nitrite Testing in Healthcare
The clinical implications of urine nitrite testing are profound. The rapid identification of UTIs allows for prompt initiation of antibiotic therapy, significantly improving patient outcomes. Moreover, nitrite testing can help reduce unnecessary antibiotic prescriptions by providing a reliable method for confirming bacterial infections.
In recent years, the integration of urine nitrite testing into routine urinalysis protocols has become standard practice in many healthcare settings. This integration is particularly beneficial in primary care, emergency departments, and outpatient clinics where quick diagnostics are essential.
Furthermore, understanding the limitations of urine nitrite tests is crucial for healthcare providers. False negatives can occur if the patient has recently urinated or if the bacteria present do not produce nitrite. Therefore, urine nitrite testing should be interpreted in conjunction with clinical symptoms and other diagnostic findings to ensure accurate diagnosis and treatment (Leacy et al., 2020).
Table 1: Clinical Implications of Urine Nitrite Testing
| Clinical Area | Implication |
|---|---|
| Diagnosis of UTIs | Rapid detection of bacterial infections |
| Antibiotic Stewardship | Reduces unnecessary antibiotic prescriptions |
| Patient Outcomes | Timely treatment leads to improved recovery rates |
| Routine Screening | Standard practice in primary care and emergency settings |
Conclusion: The Importance of Monitoring Urine Nitrite Levels
Monitoring urine nitrite levels is a vital aspect of urinary tract health management. Its role in diagnosing UTIs can streamline patient care through rapid and effective treatment strategies. Recognizing the factors that influence urine nitrite levels enables healthcare providers to interpret test results accurately and make informed clinical decisions.
As research progresses, further understanding of urine nitrite’s significance in different populations and its potential application in other urinary conditions will enhance its utility in clinical practice. Consequently, continued emphasis on urine nitrite testing can lead to improved patient outcomes and more efficient healthcare delivery.
FAQ Section
What is urine nitrite?
Urine nitrite is a compound formed when certain bacteria convert nitrates in urine to nitrites, serving as a marker for urinary tract infections.
How is urine nitrite tested?
Urine nitrite is typically tested using dipstick assays during routine urinalysis.
Can urine nitrite levels be influenced by diet?
Yes, a diet rich in nitrates can elevate urine nitrite levels, while low-nitrate diets may result in undetectable levels.
What factors can lead to false-negative urine nitrite results?
False negatives can occur if the patient has recently urinated or if the associated bacteria do not produce nitrite.
Why is urine nitrite testing important in clinical settings?
It allows for rapid diagnosis and treatment of UTIs, improving patient outcomes and reducing unnecessary antibiotic prescriptions.
References
-
Ainslie, P. N., Hoiland, R. L., & Bailey, D. M. (2016). Lessons from the laboratory; integrated regulation of cerebral blood flow during hypoxia
-
Leacy, J. K., Zouboules, S. M., Mann, C. R., et al. (2020). Neurovascular coupling remains intact during incremental ascent to high altitude (4240 m) in acclimatized healthy volunteers. Frontiers in Physiology, 9, 1691. https://doi.org/10.3389/fphys.2018.01691
-
Outcomes associated with asymptomatic bacteriuria management in elderly patients hospitalized with a ground-level fall. (2024). American Society for Microbiology. https://doi.org/10.1017/ash.2024.493
-
Risk factors for urological infection after laparoscopic ureterolithotomy. (2023). PubMed Central. https://pubmed.ncbi.nlm.nih.gov/11909557/
-
Serum metabolic profiling analysis of chronic gastritis and gastric cancer by untargeted metabolomics. (2023). PubMed Central. https://pubmed.ncbi.nlm.nih.gov/11918594/
-
Clopidogrel protects against gentamicin-induced nephrotoxicity through targeting oxidative stress, apoptosis, and coagulation pathways. (2024). Journal of Medicinal Chemistry. https://doi.org/10.1007/s00210-024-03380-5
-
Antiphospholipid syndrome presenting as isolated renal vein thrombosis: a case report and review of the literature. (2024). BMC Nephrology. https://doi.org/10.1186/s13256-025-05117-1
-
Hepatoprotective effect of royal jelly on dibutyl phthalate-induced liver injury in rats. (2024). PubMed Central. https://pubmed.ncbi.nlm.nih.gov/11910981/
-
Proinflammatory cytokines, oxidative stress, and organ function as biomarkers of soman (GD) chronic neurotoxicity. (2024). Nature Scientific Reports. https://doi.org/10.1038/s41598-025-94190-z
-
(Q)SAR Approaches to Predict the Extent of Nitrosation in Pharmaceutical Compounds. (2023). PubMed Central. https://pubmed.ncbi.nlm.nih.gov/11921035/