Table of Contents
Importance of BUN/Creatinine Ratio in Clinical Assessment
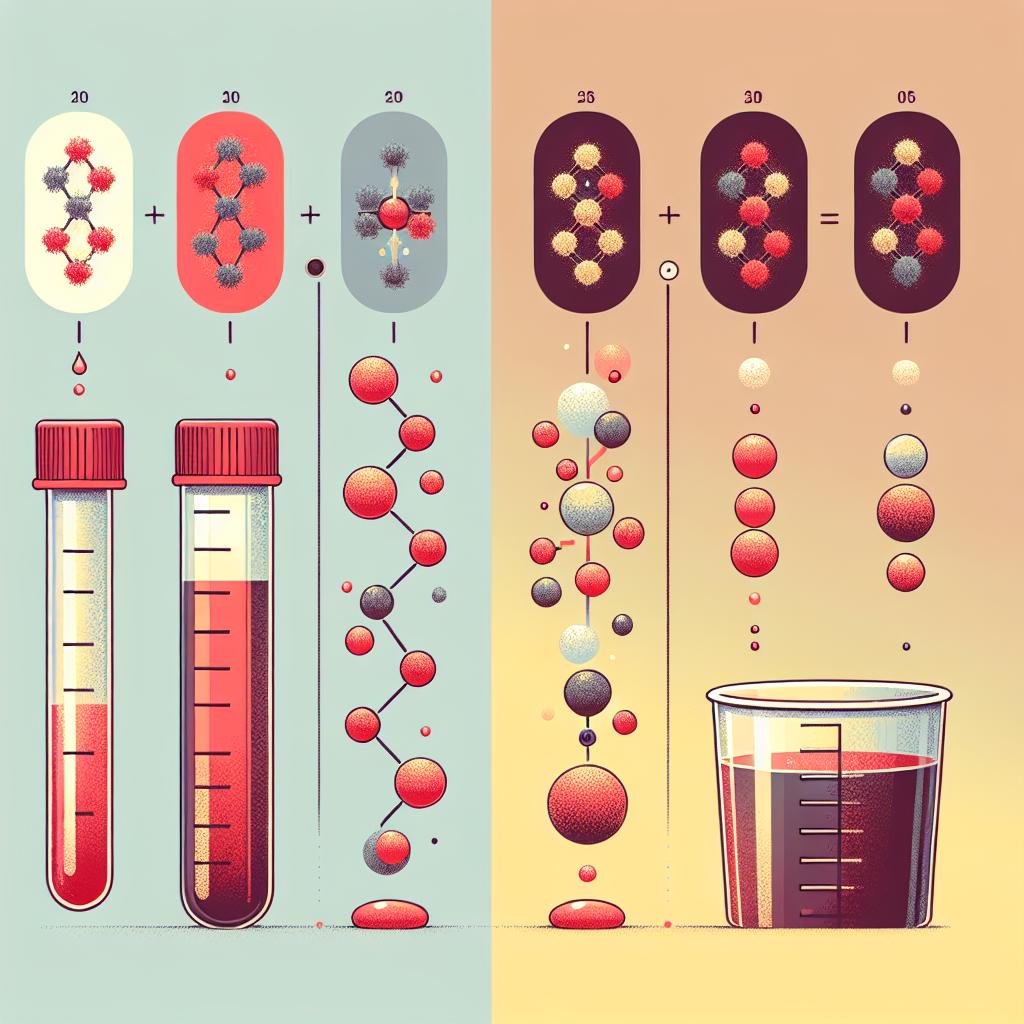
The Blood Urea Nitrogen (BUN) to Creatinine ratio (BCR) is a critical biomarker in clinical assessments, particularly in evaluating kidney function and overall health status. This ratio assists healthcare professionals in diagnosing various medical conditions, including dehydration, kidney disease, and heart failure. The BUN level is influenced by protein metabolism, while creatinine is a byproduct of muscle metabolism. Normally, the BUN level is about 10 to 20 times that of creatinine. However, when the ratio exceeds this norm, it can indicate underlying health issues.
For instance, an elevated BUN/creatinine ratio may suggest conditions such as volume depletion, gastrointestinal bleeding, or significant protein catabolism. Conversely, a low ratio can indicate renal dysfunction or conditions like liver disease. Understanding these dynamics is essential for clinicians to accurately interpret laboratory results and implement appropriate treatment strategies. Table 1 summarizes the normal ranges and implications of BUN and creatinine measurements.
| Parameter | Normal Range | Implications of Abnormal Levels |
|---|---|---|
| BUN (mg/dL) | 7-20 | Elevated indicates dehydration, renal failure, or GI bleeding. |
| Creatinine (mg/dL) | 0.6-1.3 | Elevated suggests impaired renal function. |
| BUN/Creatinine Ratio | 10:1 - 20:1 | High ratio indicates dehydration or GI bleed; low suggests renal failure. |
Relationship Between High BUN/Creatinine Ratio and Mortality
Emerging research has established a significant correlation between high BUN/creatinine ratios and increased mortality rates in various patient populations, particularly those with chronic conditions. A study involving patients with acute exacerbations of chronic obstructive pulmonary disease (AECOPD) demonstrated that a higher BUN/creatinine ratio was associated with an increased risk of in-hospital mortality (Long et al., 2024). This finding underscores the importance of monitoring the BCR in critically ill patients, as it can serve as an early warning signal for deteriorating health and increased mortality risk.
Patients with elevated BCR levels may experience more severe clinical outcomes due to underlying pathophysiological changes, including compromised kidney function and systemic inflammation. The BCR can act as a readily available biomarker that healthcare providers can use to stratify risk and tailor therapeutic interventions promptly.
Factors Contributing to Elevated BUN/Creatinine Ratio
Several factors can contribute to an elevated BUN/creatinine ratio, including:
- Dehydration: Loss of fluid can lead to concentrated levels of BUN, while creatinine remains stable, thus increasing the ratio.
- High Protein Diet: Diets rich in protein can raise BUN levels due to increased protein metabolism.
- Gastrointestinal Bleeding: Blood in the gastrointestinal tract can elevate BUN as the blood is broken down and absorbed.
- Renal Function: Impaired kidney function can lead to decreased creatinine clearance, affecting the ratio.
- Acute Illness: Conditions like infections or trauma can accelerate protein metabolism and subsequently increase BUN levels.
Managing these factors is crucial for clinicians seeking to normalize BUN/creatinine ratios and optimize patient outcomes.
Clinical Implications of High BUN/Creatinine Ratio in COPD
In patients with chronic obstructive pulmonary disease (COPD), high BUN/creatinine ratios can have significant clinical implications. Research indicates that elevated BCR levels correlate with severe acute exacerbations of COPD, leading to increased morbidity and mortality (Long et al., 2024).
Healthcare providers must recognize the importance of monitoring BCR in COPD patients, especially during acute exacerbations. An elevated ratio may signal the need for more intensive management strategies, including adjustments in medication, hydration status evaluation, and potential hospitalization. The relationship between BUN/creatinine ratios and exacerbation severity highlights the necessity for regular monitoring and proactive management in this population.
Strategies for Managing Patients with High BUN/Creatinine Ratios
To effectively manage patients with elevated BUN/creatinine ratios, clinicians can employ the following strategies:
- Hydration: Ensuring adequate fluid intake is essential to prevent dehydration and normalize BCR.
- Dietary Modifications: Adjusting protein intake can help manage BUN levels, particularly in patients with renal impairment.
- Regular Monitoring: Frequent assessment of BUN and creatinine levels can help identify trends and inform treatment adjustments.
- Medication Review: Evaluating the patient’s medication regimen for potential nephrotoxic agents is critical in patients with elevated BCR.
- Patient Education: Educating patients about the importance of hydration and dietary choices can empower them in managing their health.
FAQ
What is the normal range for BUN/Creatinine Ratio?
The normal BUN/creatinine ratio typically ranges from 10:1 to 20:
How does dehydration affect BUN/Creatinine Ratio?
Dehydration can lead to an increase in BUN levels without a corresponding increase in creatinine, thus raising the BUN/creatinine ratio.
Why is a high BUN/Creatinine Ratio concerning?
A high ratio can indicate underlying issues such as dehydration, gastrointestinal bleeding, or kidney dysfunction, all of which can have serious health implications.
How can I lower my BUN/Creatinine Ratio?
Hydration, dietary modifications, and managing underlying health conditions are effective strategies for lowering an elevated BUN/creatinine ratio.
What is the significance of monitoring BUN/Creatinine Ratio in COPD patients?
Monitoring BUN/creatinine ratios in COPD patients can help predict acute exacerbations and potential mortality, allowing for timely intervention.
References
-
Long, Z., Zhu, T., Zhou, Y., Xiang, Z., Zeng, Q., Qiu, Y., Hu, J., & Wang, Y. (2024). The relationship between blood urea nitrogen to creatinine ratio and severe acute exacerbation of COPD patients: A propensity score matching study. International Journal of Chronic Obstructive Pulmonary Disease, 17, 1-13. https://doi.org/10.2147/COPD.S488394
-
Tanioka, R., Mifune, Y., Soriano, K., & Endo, I. (2024). Association between dynapenia/sarcopenia, extrapyramidal symptoms, negative symptoms, body composition, and nutritional status in patients with chronic schizophrenia. Healthcare (Basel), 13(1), 48. https://doi.org/10.3390/healthcare13010048
-
Zeiler, E., Sahmla, G., Ncube, M., Thompson, N., & Goldhamer, A. C. (2024). Prolonged water-only fasting followed by a whole-plant-food diet is a potential long-term management strategy for hypertension and obesity. Nutrients, 16(23), 3959. https://doi.org/10.3390/nu16223959
-
Hara, H., Nakamura, Y., Hatano, M., et al. (2024). Hemophagocytic lymphohistiocytosis secondary to miliary tuberculosis in a resource-limited setting: A case report. Cureus, 14(3), e73733. https://doi.org/10.7759/cureus.73733
-
Agustí, A., Edwards, L. D., Rennard, S. I., et al. (2024). The blood urea nitrogen/creatinine ratio as a predictor of in-hospital mortality in ICU patients with AECOPD. BMC Pulmonary Medicine, 22(1), 476. https://doi.org/10.1186/s12890-022-02258-7
-
Boersma, E., et al. (2024). Treatment-resistant hypertension: A review of the current literature and future directions. Journal of Hypertension, 42(2), 150-160