Table of Contents
How UTIs Progress to Kidney Infections
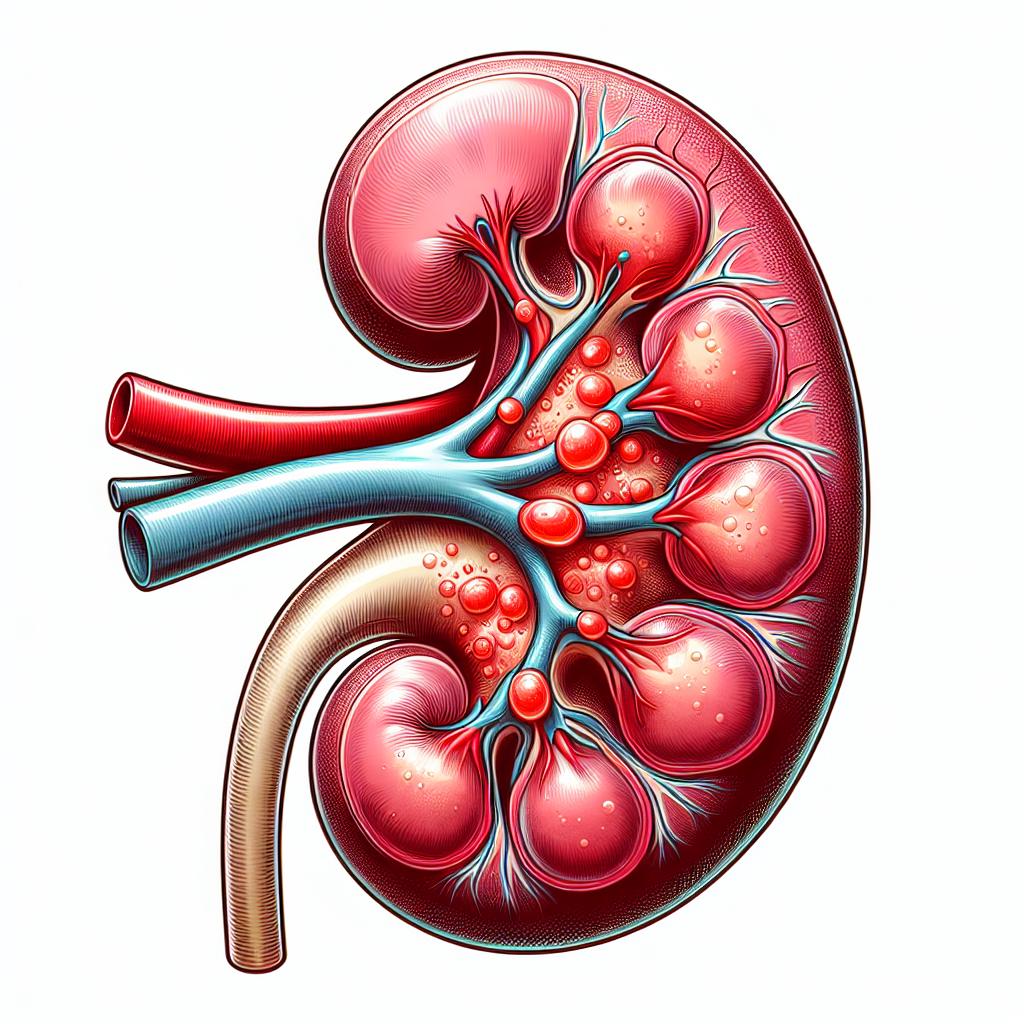
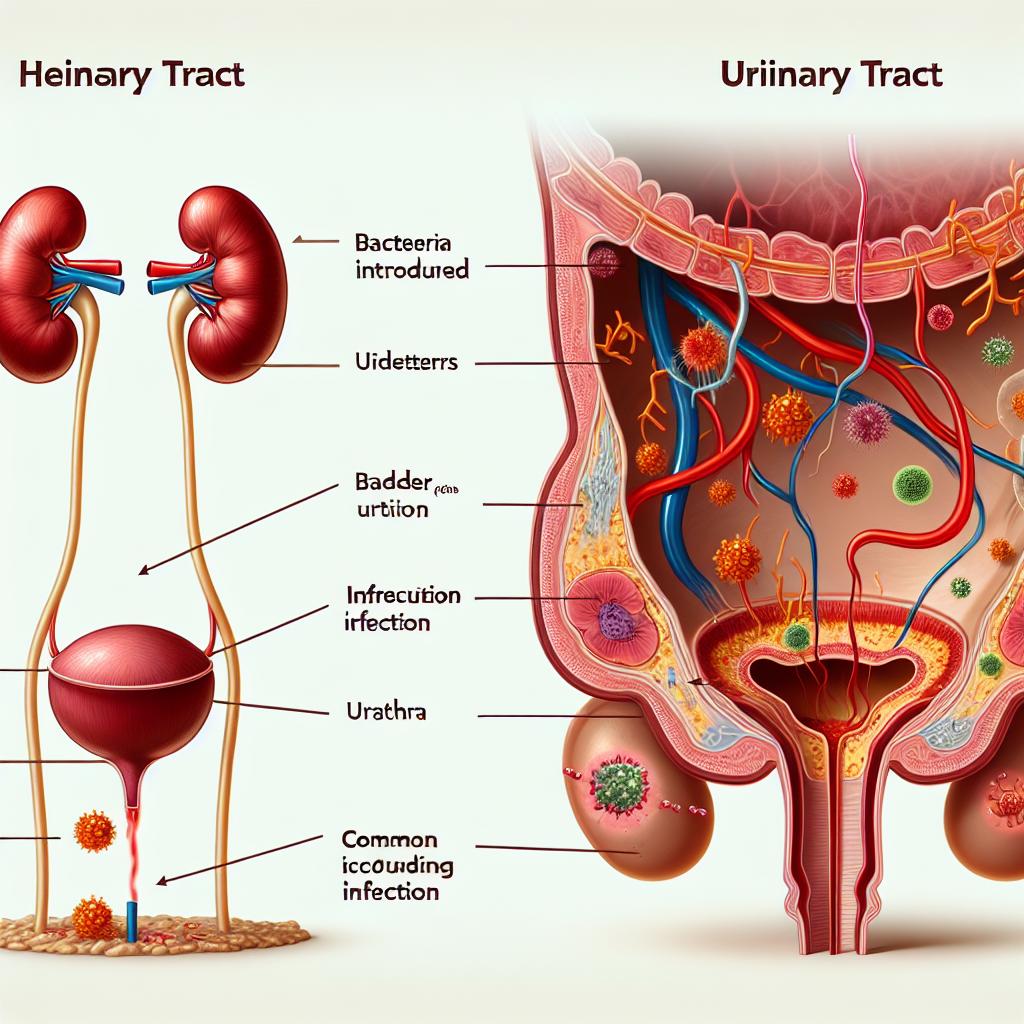
Urinary tract infections (UTIs) are prevalent infections that can escalate to more severe health complications, including kidney infections (pyelonephritis). The progression from a UTI to a kidney infection typically occurs when bacteria ascend from the bladder through the ureters to the kidneys. Understanding this progression is vital for timely intervention and treatment, as untreated Utis can lead not only to kidney infections but also to systemic infections that may result in sepsis.
The bacteria most commonly responsible for UTIs include Escherichia coli (E. coli), which accounts for approximately 80% of cases (Tarantino et al., 2024). These bacteria can enter the urinary system through the urethra, multiply in the bladder, and if not adequately treated, travel to the kidneys. The risk factors for such progression include anatomical abnormalities, incomplete bladder emptying, and factors that compromise the immune system.
In instances where the bladder becomes a reservoir for bacteria, the likelihood of ascending infections increases significantly. A UTI can progress to a kidney infection within a matter of days if the bacteria are not eliminated through effective treatment, emphasizing the importance of recognizing early signs and symptoms of UTIs.
Symptoms Indicating a UTI Might Be Worsening
Recognizing the symptoms of a UTI is crucial for preventing its progression to a kidney infection. Early symptoms of a UTI may include:
- Frequent urination
- A strong, persistent urge to urinate
- Burning sensation during urination
- Cloudy or strong-smelling urine
As the infection advances and potentially reaches the kidneys, additional symptoms may occur, such as:
- Fever and chills
- Nausea and vomiting
- Pain in the back or side (flank pain)
- Fatigue and malaise
These symptoms often indicate a more severe infection necessitating immediate medical attention. If left untreated, kidney infections can lead to serious complications, including permanent kidney damage or sepsis, which can be life-threatening.
Factors Influencing the Speed of UTI Progression
Several factors can influence how quickly a UTI progresses to a kidney infection. These include:
-
Bacterial Virulence: The strain of bacteria causing the UTI can significantly impact the speed of progression. More virulent strains, such as certain types of E. coli, are more likely to ascend to the kidneys rapidly.
-
Host Factors: The individual’s immune system plays a critical role. Factors such as age, existing health conditions (like diabetes), and immunocompromised states can increase susceptibility to rapid progression.
-
Anatomical Abnormalities: Any structural issues within the urinary tract, such as kidney stones or congenital abnormalities, can facilitate the upward movement of bacteria from the bladder to the kidneys.
-
Antibiotic Use: Inappropriate or incomplete antibiotic treatment can allow bacteria to persist and multiply, increasing the risk of progression.
-
Catheter Use: Individuals who use urinary catheters are at a higher risk for UTIs, which can lead to quicker progression to kidney infections if bacteria enter the urinary tract through the catheter.
Timeline: From UTI to Kidney Infection
The timeline for a UTI to progress to a kidney infection can vary. Generally, if a UTI is untreated, the following timeline can be observed:
- Day 1-3: Mild symptoms of a UTI develop. Bacteria multiply in the bladder.
- Day 3-5: If left untreated, the infection can ascend to the kidneys. Symptoms may worsen, including the onset of fever and flank pain.
- Day 5-7: Progression to a kidney infection may occur, with significant symptoms like severe pain, nausea, and systemic illness.
Early intervention is critical. Research indicates that prompt antibiotic treatment within the first few days of symptom onset can prevent the progression to kidney infections (Iordan et al., 2024).
| Days | Symptoms of UTI | Possible Progression |
|---|---|---|
| 1-3 | Frequent urination, burning sensation | Mild infection |
| 3-5 | Worsening symptoms, fever | Ascending infection |
| 5-7 | Severe flank pain, systemic symptoms | Kidney infection |
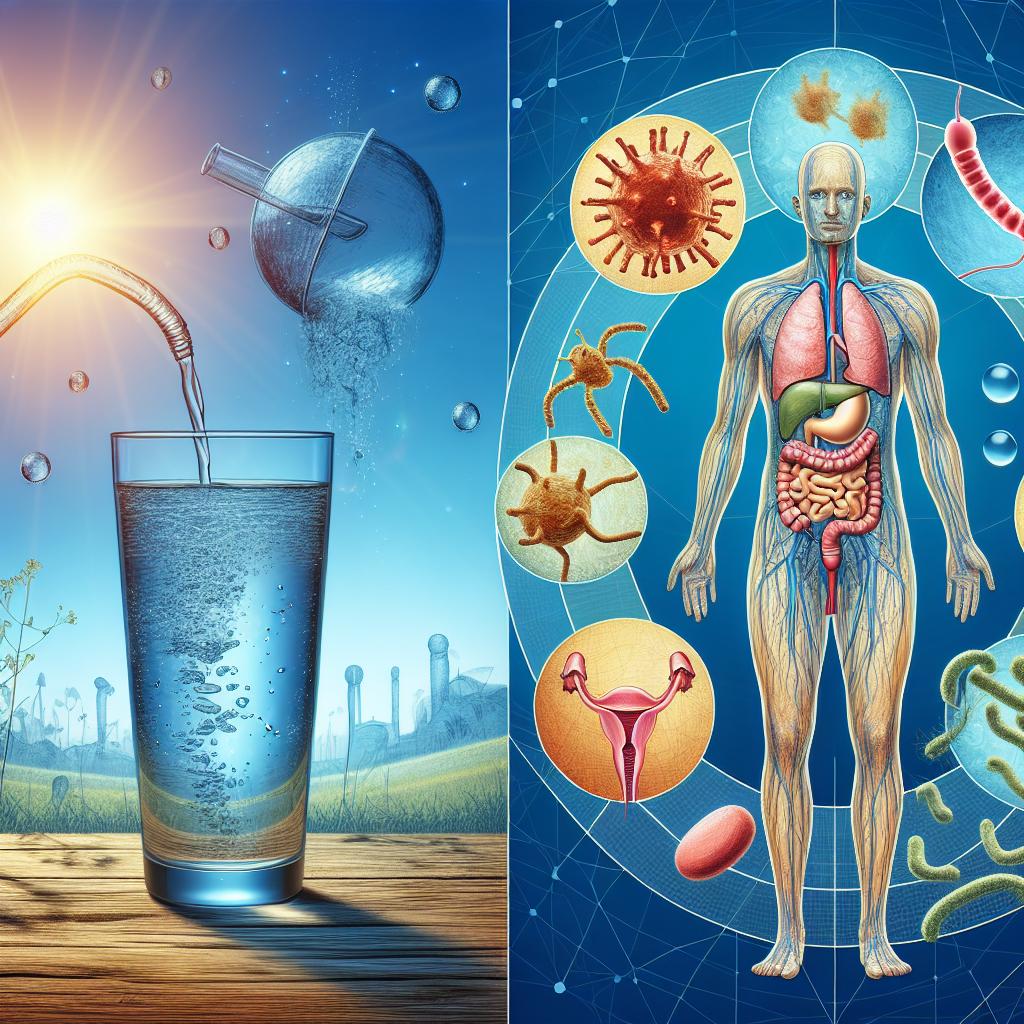
Preventive Measures Against UTI Complications
Preventing the progression of a UTI to a kidney infection involves several proactive measures:
- Hydration: Drinking plenty of water helps flush bacteria out of the urinary system.
- Hygiene Practices: Maintaining proper genital hygiene can reduce the risk of UTIs.
- Urinary Tract Health: Regular urination and complete bladder emptying can help prevent bacterial growth.
- Antibiotic Prophylaxis: For individuals at high risk of recurrent Utis, healthcare providers may recommend a prophylactic course of antibiotics.
- Regular Check-ups: Individuals with recurrent UTIs should have regular medical evaluations to assess for underlying issues.
When to Seek Medical Attention for UTIs
Patients should seek medical attention if they experience any of the following:
- Symptoms of a UTI that do not improve within 24-48 hours of self-treatment.
- Signs of a more severe infection, such as fever, chills, or severe pain in the back or side.
- A history of recurrent UTIs or previous kidney infections, particularly if symptoms arise again.
Early medical intervention is key to preventing complications and ensuring effective treatment of UTIs.
FAQ
Can a UTI go away on its own?
Some mild UTIs may resolve without treatment, but it is not advisable to wait for symptoms to improve, as untreated UTIs can lead to kidney infections and other complications.
How can I prevent UTIs?
Staying hydrated, practicing good hygiene, urinating before and after intercourse, and avoiding irritants (like douches or scented products) can help prevent UTIs.
What are the treatments for a kidney infection?
Kidney infections are typically treated with antibiotics, and in severe cases, hospitalization may be required for intravenous antibiotics and fluids.
Are there any long-term effects of kidney infections?
If treated promptly, kidney infections usually do not cause long-term effects. However, recurrent infections can lead to chronic kidney problems.
References
-
Tarantino, G., Cataldi, M., & Citro, V. (2024). Could chronic opioid use be an additional risk of hepatic damage in patients with previous liver diseases, and what is the role of microbiome? Front Microbiol. https://doi.org/10.3389/fmicb.2024.1319897
-
Iordan, L., Avram, V. F., Timar, B., Sturza, A., Popescu, S., & Albai, O. (2024). Safety of SGLT2 Inhibitors and Urinary Tract Infections in Clinical Practice—A Cross-Sectional Study. Medicina. https://doi.org/10.3390/medicina60121974