Table of Contents
Understanding Urinary Tract Infections
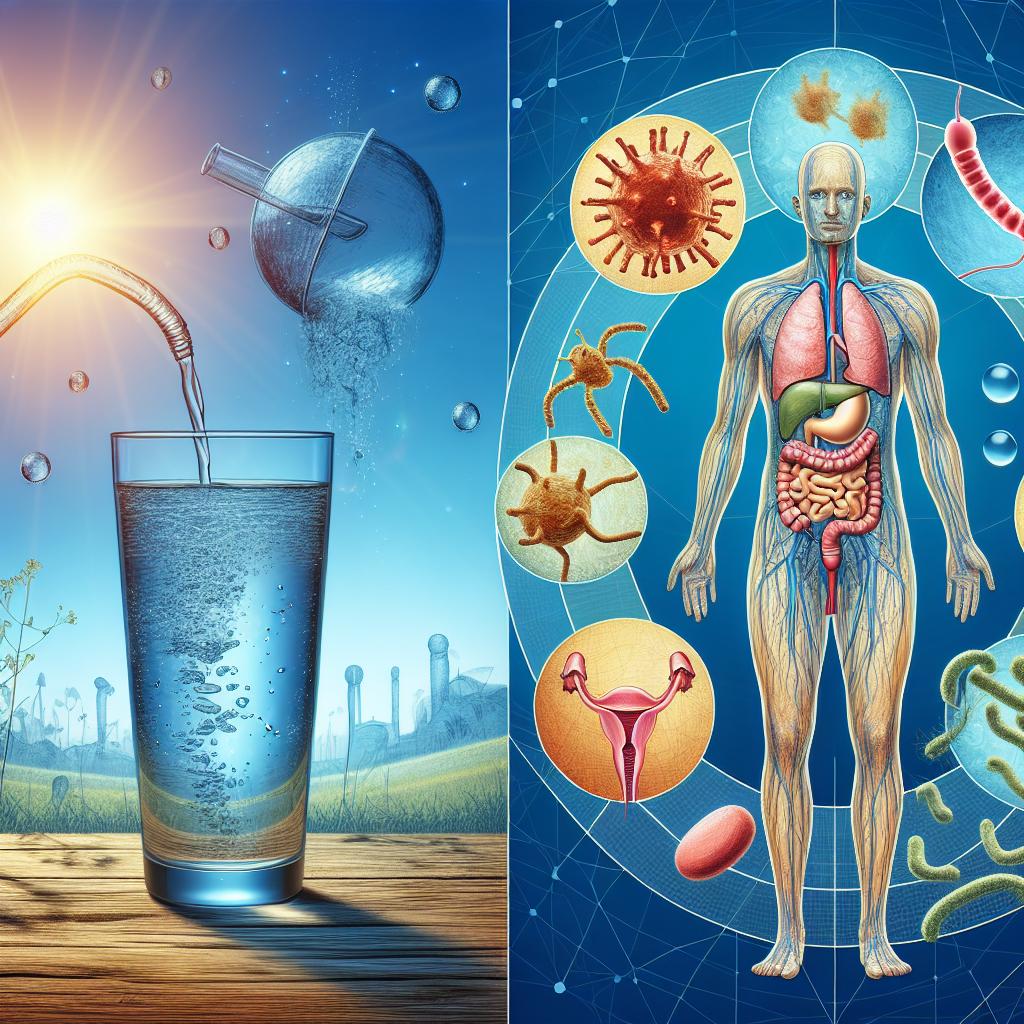
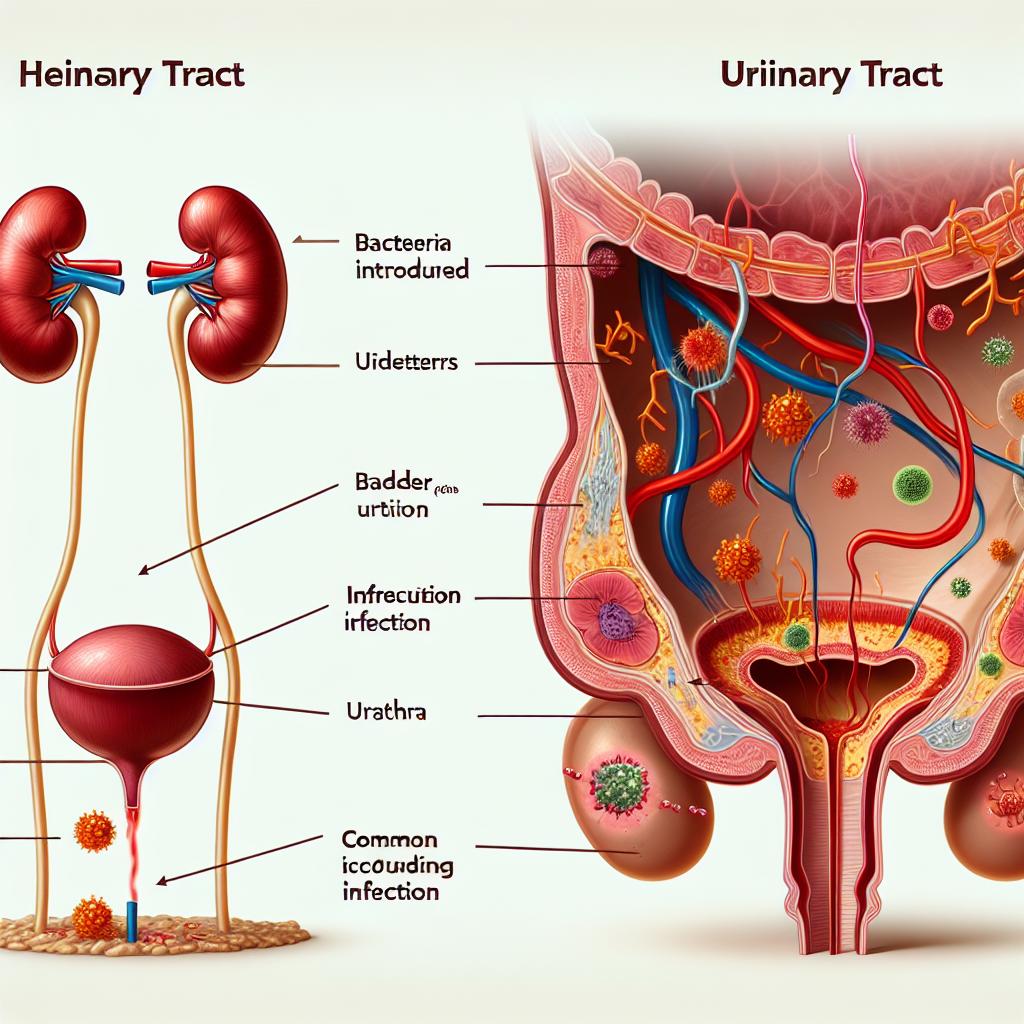
A urinary tract infection is an infection that can involve any part of the urinary tract – from the kidneys to the bladder and urethra. Bacteria, most notably Escherichia coli, are identified as the main culprits in the majority of cases. The pathogenesis of a UTI is generally explained by the ascent of bacteria from the perineal region into the urethra, where they establish colonization and multiply. In many cases, host factors such as anatomic abnormalities, changes in urine flow, and compromised immune defenses facilitate this process. Although the majority of UTIs are not life threatening, they carry substantial morbidity and can significantly impact one’s quality of life.
In women particularly, the proximity of the anus and urethral opening increases the risk of bacterial contamination. Nevertheless, another important aspect that has been discussed recently is the potential role of contaminated fingers in transferring pathogens to the urinary tract. Activities that involve inadequate hand hygiene, touching contaminated surfaces, or improper wiping after toileting can facilitate the spread of organisms into the urogenital area. An increasing body of work suggests that even a small inoculum transferred from the fingers can sometimes overcome the body’s natural barriers and lead to an infection.
The Role of Our Fingers in UTI Transmission
Our hands serve as one of the primary interfaces between our body and the external environment. They interact with a wide range of surfaces, objects, and bodily fluids, and if not cleaned properly, they can harbor pathogenic bacteria. Contaminated fingers can inadvertently transfer bacteria to the urogenital area during either personal hygiene routines or routine daily activities. For example, if infected or contaminated fingertips are used to clean the periurethral area after urination or during menstruation, the bacteria on these fingers can be introduced directly into the urethral opening.
This risk is especially important in settings where hygiene is compromised, such as in regions with limited availability of clean water or among individuals who have difficulties performing adequate self-care. In fact, studies have suggested that women with neuromuscular diseases may already have additional difficulties when they attempt to urinate away from home, increasing their vulnerability to complications such as urinary tract infections [1]. These individuals often rely on assistance or improvise solutions that may not always be sterile, causing a higher chance for bacterial entry. Moreover, when the natural mechanism for bladder emptying is impaired, any contamination introduced by the fingers carries a greater risk of producing an infection because of prolonged urine retention and an overdistended bladder that impairs local immune defense.
In a similar manner, even in otherwise healthy individuals, neglect of proper hand hygiene can result in the accumulation of bacteria that once introduced into the urinary tract, may set the stage for a UTI. Factors such as using fingers for manual cleaning during toileting, applying cosmetic products without first washing hands, or even caring for children and coming in contact with their potentially contaminated hands can contribute to overall risk. The infectious potential of such transmission is contingent on the virulence of the organisms, the load of bacteria transferred, and the individual’s immune response.
Factors Increasing UTI Risk from Finger Contamination
Personal Hygiene and Daily Routines
One of the most straightforward factors linked with increased odds of UTI transmission is poor hand hygiene. In situations where individuals neglect proper hand washing after using the restroom, the microbial load on the fingers can be excessively high, resulting in a subsequent transfer of these microbes during touch contact with the perineal area. In environments with poor sanitation or inadequate hygiene infrastructure, the inherent risk escalates. Additionally, personal care practices, such as using communal towels or shared bathroom items, can facilitate cross-contamination and increase the opportunity for bacterial transmission.
Challenges in Special Populations
Certain populations are inherently at greater risk for UTIs. For instance, women with neuromuscular diseases face unique challenges when attempting to urinate in public or unsupervised settings [1]. These conditions can hinder mobility and reduce the ability to maintain proper hygiene practices, thus increasing the probability that their hands may be contaminated or used in ways that inadvertently introduce bacteria into the urinary tract. These individuals might struggle with self-care due to physical limitations and may depend on caregivers for assistance. In these circumstances, the standard practices for preventing UTIs may be harder to implement, leading to a higher prevalence of infections. Data from functional and radiological studies in diverse clinical scenarios continue to highlight the need for targeted interventions in such vulnerable groups.
Environmental and Socio-Cultural Factors
Beyond personal hygiene, environmental factors such as overcrowded living conditions, limited access to clean water, or inadequate public restroom facilities play a significant role in UTI risk. When these factors converge with individual behavioral practices such as inadequate hand washing, the likelihood of bacterial contamination increases substantially. For example, surveys conducted in areas with constrained sanitation have indicated a high prevalence of enteric infections among individuals with inadequate hand hygiene. Although these environments are often associated with gastrointestinal infections, the same principles of transmission apply to uropathogenic bacteria. Furthermore, cultures that prioritize communal practices over frequent personal cleaning might inadvertently propagate higher rates of contamination, thereby facilitating the spread of bacteria from fingers to the urinary tract.
The Impact of Chronic Conditions
Patients with chronic conditions such as diabetes mellitus, immunosuppression, or advanced age have modified immune responses that make them more susceptible to infections. When such patients are exposed to bacteria—whether through the hands or other routes—the impaired immune surveillance can allow even a low inoculum to develop into an active infection. For instance, diabetic patients typically have impaired neutrophil function and poor microvascular circulation, making it more difficult for the body to clear bacterial infections. Consequently, these patients are not only more prone to UTIs but may also experience complications such as pyelonephritis if the infection ascends to the upper urinary tract.
Prevention Strategies: How to Reduce UTI Risk from Finger Contamination
Given the potential role of fingertips in transferring bacteria, adhering to strict hygiene practices is paramount. The following strategies are most effective in reducing the risk of UTIs associated with finger contact:
Rigorous Hand Washing
Frequent and proper hand washing with soap and water stands as the first barrier against the spread of bacteria. It is important to wash hands both before and after any contact with the perineal area or after using the restroom. Detailed instructions for proper hand washing — using soap to clean between fingers, under the nails, and for at least 20 seconds — should be followed. The Centers for Disease Control and Prevention (CDC) emphasize this repetitive action because it physically removes pathogens rather than killing them, thereby substantially reducing the risk of contamination.
Use of Hand Sanitizers
In circumstances where soap and water are not readily available, alcohol-based hand sanitizers offer an alternative, although they may not be as effective if hands are visibly soiled. Sanitizers containing at least 60% alcohol have been found to reduce bacterial counts significantly. However, their use should complement and not replace conventional hand washing practices. As the potential for contamination is greatest after hand-to-surface interactions, frequent use, particularly before any personal hygiene routines related to the genital area, is strongly advised.
Safe Wiping and Grooming Practices
The manner in which one cleans the perineal region is critical. It is generally recommended to wipe from front to back in order to prevent the inadvertent transfer of bacteria from the anal region towards the urethra. In addition, the use of disposable wipes, especially when on the go, can minimize bacterial spread. For individuals with limited dexterity, the assistance of caregivers who are well-trained in maintaining hygiene protocols is essential. Educational programs for patients — particularly those with neuromuscular diseases or physical limitations — should emphasize the importance of safe wiping techniques in preventing UTIs.
Environmental and Lifestyle Considerations
Access to clean water and sanitary facilities is a cornerstone of infection prevention. Public awareness programs and community interventions that improve access to hygiene resources can have a broad impact on reducing UTI incidence, especially in underserved areas. Additionally, individuals should be encouraged to avoid practices that may compromise hygiene, such as sharing towels or improperly storing personal hygiene products in communal spaces.
Special Considerations for Vulnerable Populations
For special populations, such as individuals with neuromuscular disorders or those with incontinence issues, targeted strategies are crucial. For instance, in a study investigating challenges faced by women with neuromuscular diseases when having to urinate away from home, it was noted that these individuals often miss opportunities to empty their bladder completely, leading to urine stasis and subsequent infections [1]. Interventions may include adaptive devices designed to facilitate self-care, regular scheduled toileting, and involvement of caregivers in maintaining hygiene protocols. Enhanced education tailored to these groups can help mitigate the risks associated with reduced bladder emptying and poor hygiene.
Cultural and Behavioral Interventions
Recognizing the role of cultural practices in everyday hygiene is essential. Health education initiatives that respect cultural norms while promoting best practices for hygiene can empower communities to adopt preventive strategies. For example, public campaigns that encourage hand washing and safe restroom practices in schools and workplaces have shown promise in reducing the overall burden of bacterial infections, including UTIs. In these programs, visual aids like posters and instructional videos can be particularly effective in demonstrating proper hand washing techniques and safe wiping practices.
Research Insights and Clinical Evidence
While numerous studies have focused on the epidemiology and treatment of UTIs, only a few have addressed the specific connection between hand contamination and the onset of UTIs. An investigation into the challenges faced by women with neuromuscular diseases highlighted the precarious balance these patients maintain between self-care and dependence on caregivers to manage urinary hygiene [1]. The study revealed that impaired mobility, compounded with environmental barriers, results in situations where hands become an inadvertent conduit of bacteria from contaminated sources to the urinary tract. Although the study did not directly measure rates of UTIs in this population, it underscored the frequency of secondary complications, including UTIs, in individuals lacking effective urinary hygiene.
Another source, abstracts from the 2023 Annual Meeting of the Society of General Internal Medicine [3], have repeatedly emphasized the role of comprehensive infection prevention strategies in vulnerable populations. Although these abstracts primarily focus on broad infection control methods in hospital settings, the principles extrapolated from their data also support the notion that manual hygiene significantly affects infection rates in the general community. The takeaway is that adherence to sanitation protocols not only prevents enteric or respiratory infections but might also extend to reducing the risk of urinary infections.
Furthermore, a closer look at the interplay between urogenital health and hygiene reveals that even subtle lapses in hand care can facilitate colonization of the urethra by uropathogenic E. coli and other bacteria. Laboratory studies evaluating bacterial adherence to urothelial cells have demonstrated that even a small inoculum can trigger an inflammatory cascade if the host defences are compromised. These findings are in line with clinical observations, where patients with poor hand hygiene often present with recurrent Utis that are difficult to treat due to the resilient nature of bacteria forming biofilms on uroepithelial surfaces.
A summary of key factors and their association with UTI risk is provided in Table 1 below.
| Risk Factor | Mechanism of Increased Risk | Population Impact |
|---|---|---|
| Poor hand hygiene | Bacterial contamination from the environment transferred via fingers | General community; high in developing areas |
| Impaired mobility | Reduced ability to maintain personal hygiene; dependency on caregivers | Neuromuscular disease patients, elderly |
| Delayed bladder emptying | Prolonged urine retention increases bacterial growth and biofilm formation | Individuals with physical limitations |
| Environmental/sanitation issues | Inadequate access to clean facilities increases exposure to pathogens | Populations in resource-limited settings |
| Chronic illnesses | Altered immune response; impaired clearance of pathogens | Diabetic patients; immunocompromised |
Table 1. Key Risk Factors for UTIs Associated with Poor Hand Hygiene and Related Mechanisms.
The table above summarizes key hazards that can predispose individuals to UTIs. Clinical correlation with patient outcomes suggests that a holistic approach to hygiene, combined with interventions tailored to the underlying risk factors, is necessary for effective prevention.
In addition to behavioral and environmental interventions, emerging research is also focusing on molecular markers of inflammation in the urinary tract. Although such markers have primarily been studied in the context of chronic kidney disease and intervertebral disc degeneration [4], the insights gained from these studies highlight that inflammatory mediators are a common denominator across various tissues. For example, cytokines released by urothelial cells in response to bacterial invasion may serve as early indicators of infection before clinical symptoms become pronounced. This underscores the importance of timely and diligent hygiene practices that can suppress the inflammatory cascade before it leads to symptomatic UTIs.
Implications for Daily Life and Preventive Health
The possibility of finger-mediated transmission of uropathogens necessitates a shift in our daily habits. Given that hands are involved in nearly every aspect of our routine—from cooking and eating to managing personal hygiene—it becomes crucial to integrate effective hand-washing routines into everyday life. For many, especially those with active lifestyles or long working hours, strategic breaks for hand cleaning may prevent the spread of microbes to sensitive areas, including the urogenital region.
For caregivers and individuals with limited mobility, educational efforts should emphasize the importance of using assistive devices that promote thorough cleaning. Institutions like rehabilitation centers should provide specialized support to ensure that patients with neuromuscular disorders can maintain hygiene that minimizes the risk of UTIs and other infections.
Moreover, integrating hand hygiene protocols into public health policies can reduce the incidence of UTIs across larger populations. Simple, yet consistent messages about the importance of washing hands before and after bathroom use or contact with potentially contaminated surfaces can make a measurable difference. As more evidence emerges linking hand hygiene with decreased UTI rates, it becomes imperative that both healthcare providers and policy makers leverage this knowledge in developing public health campaigns.
Preventive health is not solely the responsibility of the individual, but also of the healthcare system and society at large. Public health initiatives should target vulnerable communities with the dual goals of increasing awareness and improving access to sanitation infrastructures, such as clean public restrooms and readily available hand-washing stations. In settings with constrained resources, even affordable soap-based interventions can have a profound impact on lowering UTI risk.
Clinical Management and Future Perspectives
When UTIs do occur, early clinical recognition and management are vital. The standard treatment protocol for uncomplicated UTIs typically involves a course of antibiotics. However, the increasing prevalence of antibiotic-resistant bacteria necessitates strategies that focus on prevention. Effective patient education about hand hygiene and proper cleaning techniques is not only cost-effective but also minimizes the need for repeated antibiotic courses.
Moreover, research suggests that monitoring inflammatory markers in high-risk patients could serve as an early warning system, prompting timely interventions before the infection progresses to a more complicated stage. For instance, a patient with diabetes who habitually exhibits poor hand hygiene might benefit from periodic screening tests that evaluate cytokine levels in the urine. Early detection of a low-grade inflammatory response could allow for preemptive measures, ranging from behavioral modification to prophylactic antimicrobial therapy.
Additionally, future studies may focus on the molecular pathways activated by bacterial adhesion to urothelial cells. A greater understanding of these pathways could lead to novel therapeutic targets. Inhibitors that block specific cytokine receptors or the biofilm formation process might one day complement existing preventive measures, reducing reliance on antibiotics and lowering the risk of resistance.
Finally, as telemedicine and remote healthcare continue to evolve, digital health technologies can play an essential role in monitoring patient hygiene practices. Smart devices integrated into home bathrooms, for example, could remind individuals to wash their hands or even monitor the quality of water used for hand washing. Such technology, though in its infancy, could become a cornerstone in preventive medicine, particularly in vulnerable populations.
Conclusion
In summary, urinary tract infections are a pervasive health problem that can be influenced by a surprisingly simple factor: the cleanliness of our fingers. Our hands come into contact with a multitude of bacteria daily, and when proper hygiene is not observed, these pathogens can be transferred to the urogenital area, ultimately instigating infection. The risk is further amplified in populations that struggle with mobility or have specific neuromuscular challenges, where difficulties with accessing proper facilities may lead to compromised hygiene practices [1].
Preventative strategies, including rigorous hand washing, the use of effective hand sanitizers, and safe wiping techniques, are essential in mitigating the risk. Environmental improvements and culturally sensitive public health campaigns can additionally reinforce these behaviors and reduce UTI incidence at a community level. For clinicians, educating patients about these risks and incorporating regular hygiene assessments into clinical visits can enhance outcomes.
Although studies directly linking finger contamination to UTIs may still be limited, the broader evidence indicates that proper manual hygiene is critical not only for safeguarding against respiratory and gastrointestinal infections but also for ensuring urinary tract health [3]. Continued research into the molecular underpinnings of inflammation in the urogenital tract will help refine these preventive measures and may eventually provide new therapeutic targets.
As we advance into a future where healthcare is increasingly personalized, understanding the factors contributing to UTIs will allow both patients and practitioners to implement practical steps that reduce risk while promoting overall wellness. In essence, something as seemingly mundane as hand hygiene may be the key to preventing a common and debilitating condition.
Frequently Asked Questions
Can contaminated fingers directly cause a UTI?
Yes, fingers that are contaminated with uropathogenic bacteria can transfer these microbes to the genital areIf proper hygiene is not observed—such as washing hands before contact with the perineal region—the bacteria may enter the urethra and initiate an infection [1].
Who is most at risk of acquiring a UTI via finger contamination?
Women, particularly those with impaired mobility or certain neuromuscular conditions, are at higher risk due to the closer proximity of the urethral opening to contaminated areas. Environmental factors and social settings lacking access to proper sanitation further exacerbate the risk [1][3].
What hygiene practices are recommended to prevent UTIs?
Rigorous hand washing using soap and water for at least 20 seconds, using alcohol-based hand sanitizers when soap is unavailable, and cleaning the perineal area from front to back are all recommended practices. In addition, using disposable wipes and avoiding the sharing of personal hygiene items can help reduce the bacterial load [1].
How can caregivers help individuals with limited mobility prevent UTIs?
Caregivers should be trained in proper hygiene techniques and use assistive devices to help patients maintain cleanliness, especially when self-care is challenging. Regularly scheduled toileting and the use of adaptive equipment can help ensure effective cleaning and reduce bacterial contamination [1].
Are there any technological solutions that may help prevent UTIs?
Emerging digital health technologies, such as smart reminders, sensors in bathroom fixtures, and telemedicine monitoring, are being explored to enhance personal hygiene. These innovations can prompt regular hand washing and monitor sanitation practices, particularly in vulnerable populations [3].
References
- Challenges Faced by Women With Neuromuscular Diseases When Having to Urinate Away From Home. (n.d.). Retrieved from https://pubmed.ncbi.nlm.nih.gov/11265239/
- ESPGHAN 56th Annual Meeting Abstracts. (2024)
- Abstracts from the 2023 Annual Meeting of the Society of General Internal Medicine. (2023). Retrieved from https://doi.org/10.1007/s11606-023-08226-z
- Oral Health Assessment in Chronic Kidney Disease Patients on Maintenance Haemodialysis. (2023). Retrieved from https://pubmed.ncbi.nlm.nih.gov/10775241/