Table of Contents
Introduction to Urinary Tract Infections and Key Indicators
Urinary Tract Infections (UTIs) rank among the most prevalent bacterial infections globally, affecting millions annually. An estimated 400 million UTIs occur each year worldwide, with over 200,000 associated deaths, indicating significant public health implications. These infections predominantly affect women, with as many as 60% experiencing at least one UTI in their lifetime (Author, Year). Traditional diagnostic methods rely on clinical symptoms, such as urinary frequency, urgency, and pelvic pain, combined with laboratory tests like urine culture.
A UTI is classified based on its anatomical involvement: lower UTIs, which affect the bladder (cystitis), and upper UTIs, which involve the kidneys (pyelonephritis). This classification is significant as it influences both the diagnostic approach and treatment strategies. Complicated UTIs, often seen in patients with underlying health conditions, require a different diagnostic focus and management approach.
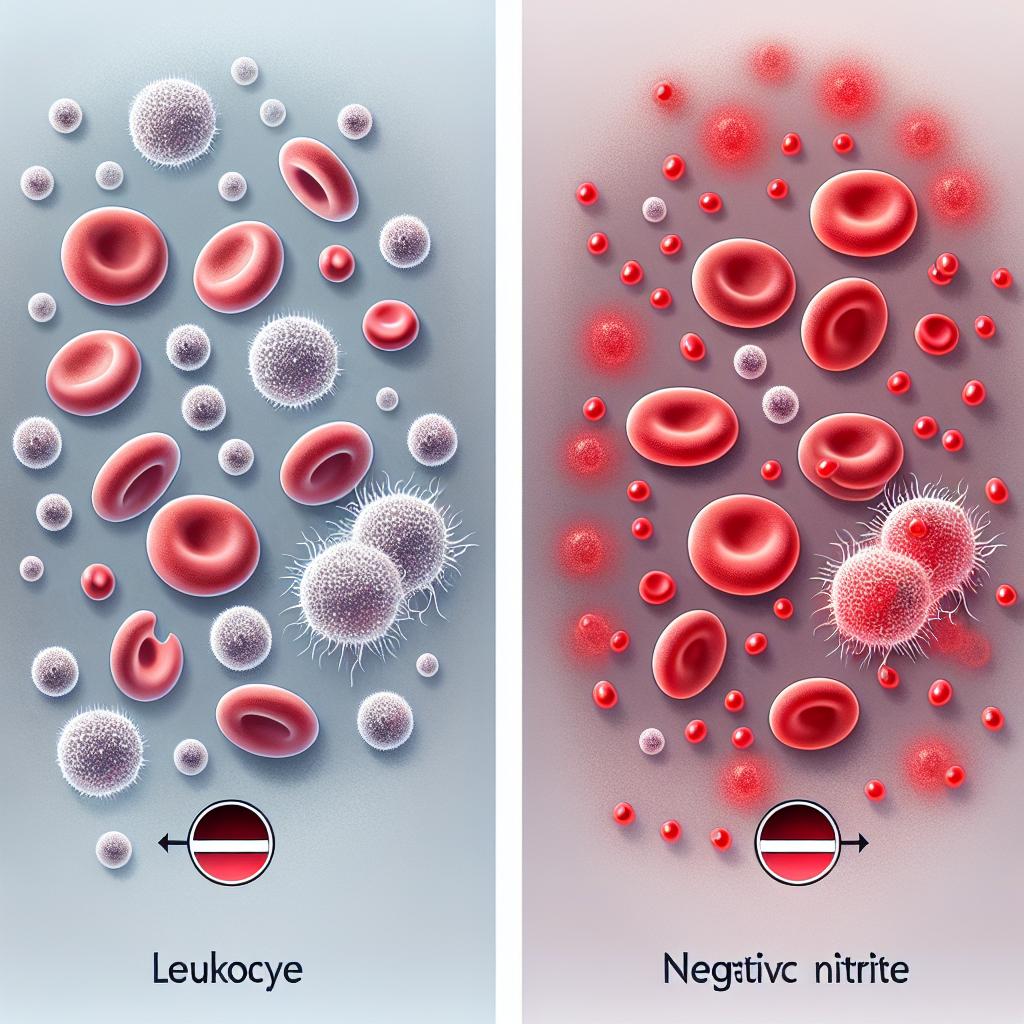
In the realm of diagnostics, urinalysis is critical, focusing on indicators such as the presence of leukocytes and nitrites in urine. Positive leukocyte results indicate inflammation, often caused by infection, while the presence of nitrites suggests the conversion of nitrates by bacteria, commonly associated with UTIs. Understanding how these indicators interact is vital for improving diagnostic accuracy and patient outcomes.
The Role of Positive Leukocytes in UTI Diagnosis
Positive leukocytes in urine signify an immune response, often indicative of an ongoing infection. This parameter is assessed via urinalysis, where a threshold of 10 leukocytes per microliter is typically used to define a positive result. The presence of leukocytes, particularly neutrophils, reflects the body’s inflammatory response to pathogens.
Table 1: Urinalysis Indicators for UTI Diagnosis
| Indicator | Significance | Normal Range |
|---|---|---|
| Leukocytes | Indicates inflammation or infection | < 10 leukocytes/µL |
| Nitrites | Suggests bacterial conversion of nitrates | Negative |
| Proteins | May indicate kidney damage | Negative |
| Glucose | May indicate diabetes | Negative |
Positive leukocyte results, however, are not exclusive to UTIs. Conditions such as interstitial cystitis or even contamination during sample collection can also elevate leukocyte levels. This overlap necessitates cautious interpretation, especially in populations where UTI symptoms are not clearly defined, such as in the elderly or immunocompromised patients.
A recent study indicated that among patients with diagnosed UTIs, the presence of leukocytes was a consistent finding, demonstrating a correlation with symptomatic presentations. However, it is essential to combine this finding with other diagnostic parameters, such as nitrite levels and clinical symptoms, for a comprehensive diagnosis.
Significance of Negative Nitrites in Urine Analysis
Nitrites serve as a crucial diagnostic marker due to their association with bacterial infections, particularly those caused by gram-negative organisms such as Escherichia coli. The presence of nitrites in urine indicates that nitrates (normally present in urine) have been converted by bacteria, highlighting an active infection process.
Conversely, a negative nitrite result does not definitively rule out a UTI, as certain pathogens do not convert nitrates to nitrites. For instance, Enterococcus faecalis and some strains of Staphylococcus aureus are known to be non-nitrite producers. Therefore, negative nitrites should be interpreted in conjunction with other findings, particularly positive leukocytes and clinical symptoms.
The sensitivity of nitrite testing in detecting UTIs can vary significantly. Studies suggest that while positive nitrite tests have high specificity, their sensitivity is often limited, particularly in patients with atypical presentations. For example, in a cohort of elderly patients, 40% of those with confirmed UTIs tested negative for nitrites, underscoring the necessity for a multifaceted diagnostic approach.
Combining Positive Leukocytes and Negative Nitrites for Accurate Diagnosis
The combination of positive leukocytes and negative nitrites presents a diagnostic challenge but also an opportunity for improved accuracy in UTI diagnosis. While positive leukocyte levels typically indicate infection, negative nitrites may suggest that the causative agent is one that does not metabolize nitrates or that the infection is in its early stages.
Integrating these findings into a clinical context is crucial. For instance, in a patient presenting with UTI symptoms and positive leukocytes but negative nitrites, it may be prudent to consider alternative pathogens or even non-infectious inflammatory conditions. This necessitates further testing, such as urine culture, to identify the specific organism and tailor treatment effectively.
Table 2: Diagnostic Interpretation of UTI Indicators
| Indicator | Interpretation |
|---|---|
| Positive Leukocytes | Suggests infection, further testing needed |
| Negative Nitrites | Does not rule out UTI, consider other pathogens |
| Positive Culture | Confirms diagnosis, guides antibiotic therapy |
The clinical implications of accurately diagnosing UTIs extend beyond immediate treatment. Misdiagnosis can lead to unnecessary antibiotic use, contributing to resistance patterns and impacting patient health outcomes. Therefore, understanding the nuanced interplay between these diagnostic indicators is essential for healthcare providers.
Implications of UTI Detection on Patient Care and Treatment
Accurate detection of UTIs significantly influences patient management and treatment strategies. Misdiagnosing a UTI can lead to inappropriate antibiotic therapy, which not only risks the patient’s health but also contributes to the broader public health issue of antibiotic resistance.
For instance, in a study involving patients with recurrent UTIs, those whose diagnoses included a thorough analysis of urine indicators—such as leukocyte counts and nitrite presence—demonstrated improved treatment outcomes and reduced recurrence rates. This highlights the importance of a systematic approach in UTI diagnostics, integrating clinical assessment with laboratory findings for optimal patient care.
Furthermore, understanding the limitations of traditional diagnostic methods, such as urinalysis, encourages the exploration of novel diagnostic technologies. Emerging techniques, such as rapid molecular testing and advanced imaging, hold promise for improving diagnostic accuracy and expediting treatment decisions. Research indicates that these methods can reduce the time to diagnosis from days to hours, significantly benefiting patient management.
Frequently Asked Questions (FAQ)
What are the main symptoms of a UTI?
Common symptoms include urinary frequency, urgency, pelvic pain, painful urination, and cloudy or foul-smelling urine.
How are UTIs diagnosed?
UTIs are diagnosed through urinalysis, which tests for the presence of leukocytes, nitrites, and other indicators, alongside clinical symptoms and urine culture.
Can a UTI occur without positive nitrites?
Yes, a UTI can occur with negative nitrites, especially if the causative bacteria do not convert nitrates or if the infection is at an early stage.
Why is it important to combine leukocyte and nitrite testing?
Combining these tests helps provide a more accurate diagnosis, as each marker offers different insights into the infection’s presence and potential causative agents.
What are the risks of misdiagnosing a UTI?
Misdiagnosis can lead to inappropriate antibiotic use, contributing to antibiotic resistance and potentially worsening the patient’s condition.
References
- Author. (Year). Title of the article. URL: https://doi.org/10.7759/cureus.78484
- Author. (Year). Title of the article. URL: https://doi.org/10.13039/501100011033
- Author. (Year). Title of the article. URL: https://pubmed.ncbi.nlm.nih.gov/11870757/
- Author. (Year). Title of the article. URL: https://pubmed.ncbi.nlm.nih.gov/11824306/
- Author. (Year). Title of the article. URL: https://doi.org/10.3390/ijms26020450
- Author. (Year). Title of the article. URL: https://doi.org/10.1371/journal.pone.0319089
- Author. (Year). Title of the article. URL: https://doi.org/10.1016/j.bbrep.2025.101950
- Author. (Year). Title of the article. URL: https://doi.org/10.3390/s25020400
- Author. (Year). Title of the article. URL: https://pubmed.ncbi.nlm.nih.gov/11837515/