Table of Contents
Understanding UTI Pain: Triggers and Symptom Overview
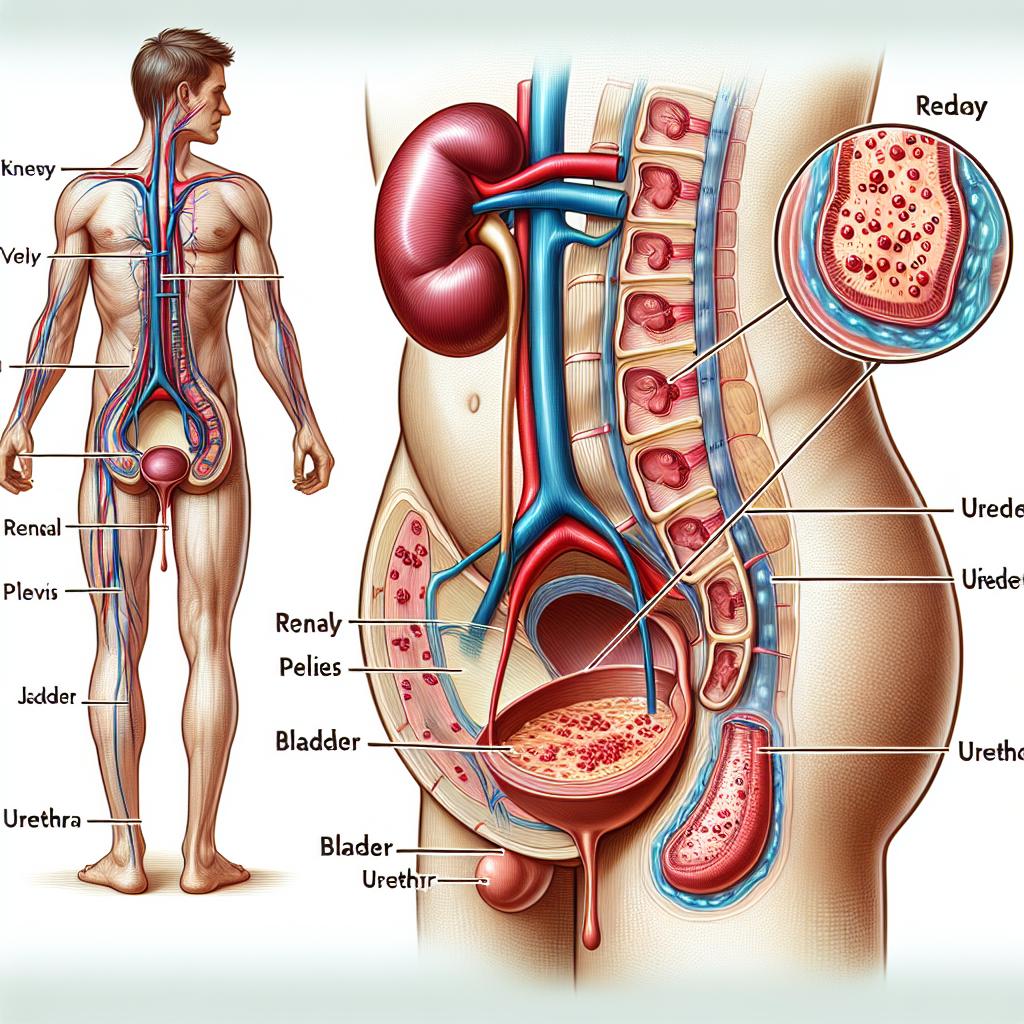
UTI pain can arise from a variety of biological and physiological factors. Infections of the urinary system, particularly those affecting the bladder (cystitis) or kidneys (pyelonephritis), can release bacterial toxins and inflammatory mediators that irritate the lining of the urinary tract. This inflammation leads to nerve activation and the sensitization of pain pathways, which may result in burning sensations during urination and persistent pelvic discomfort.
Many patients report that their pain is exacerbated by frequent urination and the passage of urine through an inflamed urethra. This pain is not simply a function of the presence of bacteria, but also of the body’s local inflammatory response. In some research on chronic bacterial prostatitis—an infection that can share overlapping symptoms and pathophysiology with UTIs—treatment strategies are enhanced using adjuvant therapies that aim to reduce tissue inflammation and accelerate healing [1]. Although prostatitis is a condition specific to males, the concept of combining anti-inflammatory agents with antibiotics can also provide inspiration for UTI pain relief in both genders.
Furthermore, some patients experience referred pain that extends to lower back areas, suggesting that urinary tract inflammation sometimes involves pelvic nerve stimulation. Notably, the severity of UTI pain depends on individual differences in immune responses, pain thresholds, and any underlying conditions such as urinary tract dilation or chronic urinary incontinence. In any case, proper recognition of the pain triggers is the first step toward effective management.
Evidence-Based Medical Treatments for UTI Pain Relief
When it comes to medical intervention, prompt diagnosis and treatment are critical. In many cases, the use of antibiotics to quickly combat the underlying bacterial infection is the cornerstone of UTI management. However, antibiotic treatment alone often does not immediately relieve pain. It is here that adjunct therapies come to the forefront.
For instance, in the management of chronic bacterial prostatitis—a condition similar in many respects to frequent Utis—recent research has shown that adding adjuvants like the nutraceutical formulation Butirprost® to fluoroquinolone therapy can enhance pain relief, reduce lower urinary tract symptoms, and improve quality of life [1]. The active ingredients of such adjuvants help reduce inflammation and promote tissue repair, potentially providing faster alleviation of pain than antibiotic therapy alone.
In addition to these combined treatments, non-steroidal anti-inflammatory drugs (NSAIDs) are often employed to target inflammation and offer symptomatic relief. Patients may be advised to follow a short course of NSAIDs to relieve acute UTI pain while awaiting improvement from antibiotic action. Medical professionals sometimes recommend local heat therapy, which increases blood circulation to the pelvic area, promoting natural healing processes and reducing spasm-related pain.
Novel diagnostic procedures also play an important role in ensuring accurate treatment. Emerging technologies, such as metagenomic next-generation sequencing (mNGS), have demonstrated increased sensitivity in detecting various pathogens from urine specimens—even in cases of low bacterial load [6]. These advances allow clinicians to tailor antibiotic treatment more precisely. Although mNGS is primarily used for diagnostic accuracy rather than pain management per se, knowing the exact pathogen helps guide efficient treatment and avoid delays that can prolong pain and discomfort.
A multidisciplinary approach is essential: while antibiotics and NSAIDs serve as the primary medical treatments, a patient’s response is monitored closely, and treatments are adjusted based on clinical progress. In cases where excessive pain or urinary obstruction is present, urologists may recommend procedures to relieve blockages, such as the placement of ureteral stents or, in complicated cases, urinary diversion [9]. Effective coordination among healthcare professionals minimizes delays in pain relief and ensures that every aspect of infection management is addressed.
Natural Remedies and Home Care for UTI Pain Relief
In addition to evidence-based pharmaceutical interventions, many individuals explore alternative natural remedies that can speed up recovery and offer additional pain relief. Home care strategies not only mitigate discomfort but also help prevent the recurrence of UTIs.
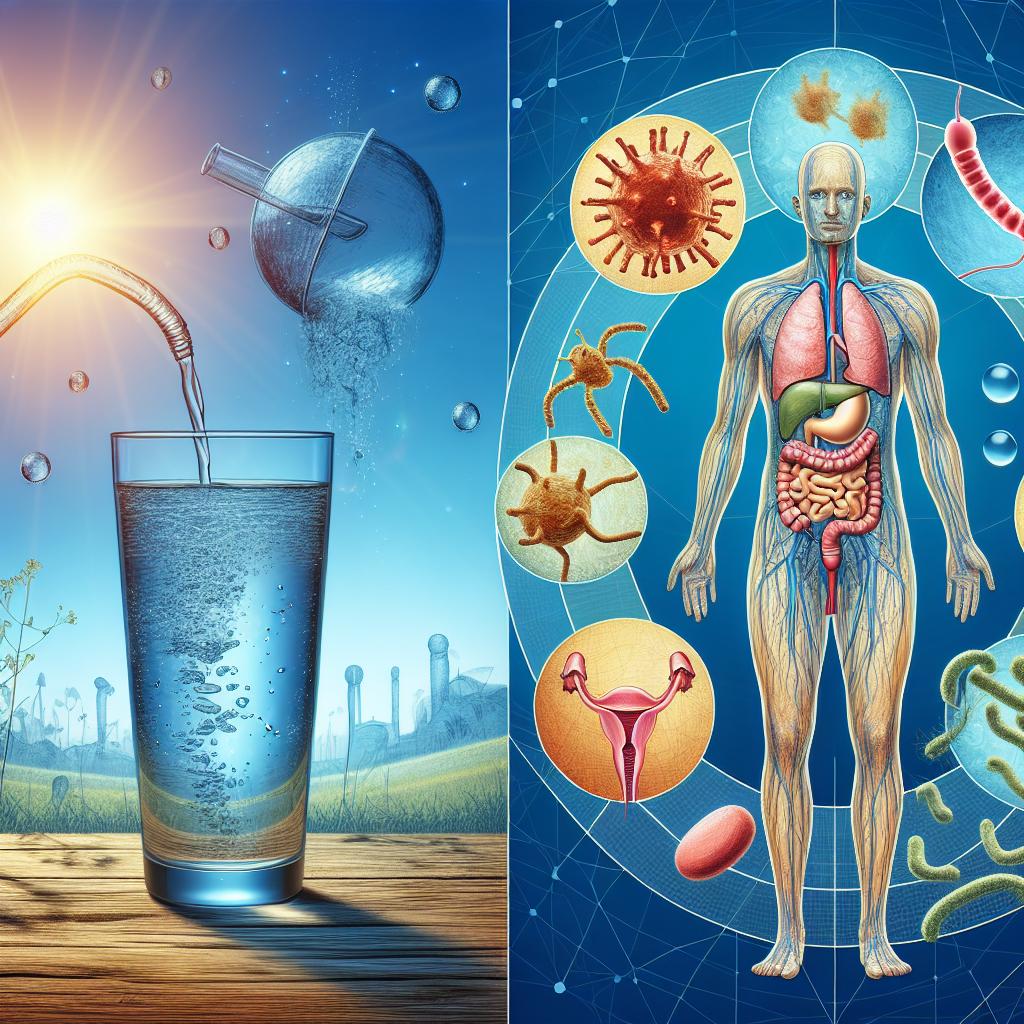
One of the most established natural remedies is the use of increased fluid intake. Hydration serves two important roles: it encourages frequent urination, which flushes out bacteria, and it maintains optimal urine concentration to reduce irritation in the urinary tract. Herbal teas—such as those containing cranberry extract, uva ursi, or garlic—are popular choices. Cranberry, in particular, has been widely recognized for its ability to prevent bacterial adhesion to the bladder wall, thereby lowering the risk of recurrent Utis and alleviating inflammation over time.
Complementary therapies such as probiotics and dietary modifications can further support urinary tract health. Probiotics help balance the natural flora within the urinary and gastrointestinal tracts, reducing pathogenic bacterial colonization. Home remedies may also include natural anti-inflammatories such as turmeric—containing curcumin—which has been shown to have potent antioxidant and anti-inflammatory properties. These natural compounds can help dampen the inflammatory response in the urinary tract, thereby reducing pain.
In some research on self‐care strategies, patients have reported improved management of urinary symptoms when they adopt a holistic lifestyle encompassing mind-body practices, adequate rest, and stress reduction techniques [8]. Self-care is a crucial component of recovery from chronic conditions, including UTIs and related urinary incontinence. Engaging in activities such as pelvic floor exercises, yoga, and mindfulness meditation not only reduces the stress that can exacerbate pain but may also help improve bladder control and reduce episodes of urinary urgency.
Patients should be encouraged to monitor their symptoms at home and maintain a diary of pain levels, dietary changes, and any natural supplements used. Although using home remedies does not replace medical treatment, these strategies are proven to offer significant adjunctive benefits and empower patients to actively participate in their own healing process.
Prevention Techniques to Minimize UTI Discomfort
Prevention is always better than cure when it comes to urinary tract infections. A proactive approach that focuses on reducing exposure to potential pathogens and strengthening urinary tract defenses can significantly lower the risk of UTIs and related pain.
Good personal hygiene, particularly after sexual activity, is essential to prevent the spread of bacteria to the urinary tract. Wiping from front to back is a simple but effective measure that minimizes the risk of fecal contamination in women. For both men and women, avoiding the use of irritating feminine hygiene products and bubble baths can reduce irritation of the urethral lining.
Also, strategies that minimize catheter-associated UTIs (CAUTIs) are critical for individuals who require long-term catheterization. Research into spectroscopic methodologies for the early detection of UTIs has indicated that innovative diagnostic devices—in combination with improved catheter designs—could play an important role in early identification and intervention for CAUTIs [7]. A recent survey among healthcare professionals has confirmed that early diagnosis is considered a high priority for reducing UTI incidence in catheterized patients. Such devices often combine fluorescence ratiometric measurements and UV–Vis absorption to monitor urine sample quality quickly, enabling timely treatment and reducing the duration of pain.
Preventive measures, including the use of antibiotic prophylaxis in well-selected high-risk individuals, have also been a subject of debate. Some studies advocate the use of low-dose antibiotics for patients with recurrent infections or significant anatomical abnormalities, while others emphasize the risk of developing antibiotic resistance. Currently, a recommended approach is to reserve prophylaxis for patients with high-grade vesicoureteral reflux or significant urinary tract dilation, as determined by ultrasound criteria [4]. Establishing guidelines in accordance with national consensus recommendations ensures that antibiotic prophylaxis is used judiciously, reducing further complications and improving overall patient outcomes.
Maintaining a healthy diet rich in antioxidants and anti-inflammatory nutrients further supports the body’s defense mechanisms. Adequate vitamin C intake, for example, not only boosts immunity but also acidifies the urine, creating an environment that is less favorable for bacterial growth. Lifestyle adjustments—such as avoiding caffeine and alcohol, which may irritate the bladder—are additional pragmatic strategies to prevent discomfort.
Finally, patients are encouraged to schedule regular follow-ups with their healthcare providers. Timely ultrasounds and renal function tests can help detect anatomical anomalies that might predispose an individual to recurrent UTIs, thereby allowing for early intervention before significant pain develops.
When and How to Seek Professional UTI Care
Despite the efficacy of home remedies and preventive measures, there are instances when professional medical care becomes indispensable. Early professional intervention is especially important if pain persists beyond a couple of days of self-care, if the patient experiences high fever, severe back or flank pain, or symptoms of systemic infection such as chills and vomiting.
A prompt evaluation by a healthcare provider can ensure that the correct antibiotics are prescribed. As discussed earlier, modern diagnostic technologies such as mNGS have greatly enhanced the accuracy of pathogen identification [6]. If you have recurrent UTIs—especially in the presence of anatomical abnormalities like urinary tract dilation or vesicoureteral reflux—it is crucial to undergo a thorough diagnostic workup. Urological evaluation may include imaging studies such as ultrasound or intravenous urography to assess the urinary tract anatomy. In complicated cases, interventional procedures like ureteral stent placement or even urinary diversion may be necessary to alleviate obstruction-induced pain and preserve renal function [9].
It is also important to note that certain populations—such as postmenopausal women, individuals with diabetes, and those with a history of kidney stones—are at higher risk for complications. These patients should seek early consultation if UTI symptoms emerge.
Furthermore, for patients who require long-term catheterization, regular monitoring in a hospital or clinic setting is vital. Innovative diagnostic devices designed for early UTI detection may be integrated into clinical protocols to ensure timely and effective intervention. These devices, currently undergoing further research and development [7], promise to reduce the period of undiagnosed infection and the associated pain.
Overall, professional care is necessary not only to treat the acute infection but also to address any underlying factors that may predispose an individual to recurrent UTIs. A multidisciplinary approach that involves primary care physicians, urologists, and, when applicable, infectious disease specialists ensures that patients receive comprehensive care for both immediate pain relief and long-term urinary tract health.
Data Table: Overview of UTI Pain Management Strategies
| Strategy Category | Approach | Time to Relief | Additional Benefits |
|---|---|---|---|
| Medical Treatments | Antibiotic therapy, NSAIDs, adjuvant formulations (e.g., Butirprost®) | Rapid (within 48–72 hours) | Resolves infection, reduces inflammation, and improves tissue repair |
| Natural Remedies | Increased fluid intake, herbal supplements (cranberry, uva ursi), probiotics, dietary modifications | Gradual (several days to weeks) | Prevents recurrences, supports immune system, enhances self-care ability |
| Preventive Measures | Improved personal hygiene, catheter care protocols, lifestyle adjustments | Ongoing | Minimizes recurrence, maintains urinary tract health |
| Professional Intervention | Urological evaluation, advanced imaging, urinary diversion | Immediate to within days | Identifies underlying issues, prevents complications, tailored treatment |
Table 1. Summary of UTI Pain Management Strategies and Associated Benefits.
Frequently Asked Questions (FAQ)
What are the common triggers for UTI pain?
UTI pain is typically triggered by bacterial infections that lead to inflammation of the urinary tract. Factors such as bladder irritation due to bacterial toxins, frequent urination, and referred pain from pelvic nerve involvement can all contribute to significant discomfort.
How effective are adjuvant treatments in relieving UTI pain?
Adjuvant treatments, such as the use of nutraceutical formulations together with standard antibiotics, have been shown to improve pain relief by reducing inflammation and promoting tissue repair. This integrated approach can result in faster recovery and better overall symptom management [1].
Can natural remedies completely replace medical treatment in managing UTIs?
Although natural remedies like increased hydration, herbal supplements, and probiotics can help manage symptoms and prevent recurrences, they should not replace medical treatment entirely. They are best used as complementary measures alongside prescribed antibiotics and anti-inflammatory medications.
When should I see a doctor for UTI pain?
It is important to seek professional care if UTI pain persists for more than a couple of days, if you experience systemic symptoms such as fever or chills, or if you have severe pain that interferes with daily activities. High-risk patients, including those with recurrent UTIs or underlying urinary tract abnormalities, should consult a healthcare provider as soon as symptoms arise.
What role do diagnostic tests play in UTI pain management?
Accurate diagnostic tests are essential for ensuring that the specific pathogen causing the infection is identified. Technologies such as metagenomic next-generation sequencing (mNGS) have enhanced diagnostic accuracy, enabling clinicians to tailor antibiotic therapy more precisely and reduce delays in treatment [6].
References
-
Crocetto, F., Barone, B., De Luca, L., Creta, M., Granulomatous Prostatitis: A Challenging Differential Diagnosis to Take into Consideration. (2025). Medicina, 61(1), 148. https://doi.org/10.3390/medicina61010148
-
Lu, Y., Zhu, Y., Ma, C., Wang, L., Zhou, M., Chen, T., … Fan, Z. (2024). Senegalin-2: A Novel Hexadecapeptide from Kassina senegalensis with Antibacterial and Muscle Relaxant Activities, and Its Derivative Senegalin-2BK as a Bradykinin Antagonist. Biomolecules, 15(1), 30. https://doi.org/10.3390/biom15010030
-
[Nutcracker Syndrome Discussion]. (2024). In Journal of Vascular Surgery: Venous and Lymphatic Disorders (Advance online publication). https://doi.org/10.1016/j.jvsv.2024.101983
-
Bahadori, A., Wilhelm-Bals, A., Caccia, J., Chehade, H., Goischke, A., Habre, C., … Parvex, P. (2024). Swiss Consensus on Prenatal and Early Postnatal Urinary Tract Dilation: Practical Approach and When to Refer. Children, 11(12), 1561. https://doi.org/10.3390/children11121561
-
Kanungo, G., Nagrath, P., Samal, P., Mishra, S., & Others. (2022). Automated Red Cell Exchange in Sickle Cell Disease Patients: Retrospective Analysis of Series of Cases in a Tertiary Care Hospital in Eastern India. Asian Journal of Transfusion Science, 12(3), 18235-35425-11202. https://pubmed.ncbi.nlm.nih.gov/11734800/
-
[Application of Metagenomic Next-Generation Sequencing]. (2024). Frontiers in Cellular and Infection Microbiology, 14, 1386377. https://doi.org/10.3389/fcimb.2024.1386377
-
[A Spectroscopic Methodology to Early Detection of Urinary Tract Infections]. (2025). Sensors, 25(2), 400. https://doi.org/10.3390/s25020400
-
Bahadori, A. (2024). Self-Care Conditioning Factors in Women and Men with Urinary Incontinence and Human T-Lymphotropic Virus Type 1. Revista Eletrônica de Enfermagem USP, 27
-
[Hydronephrosis and Survival in Cervical Cancer Patients: The Role of Urinary Diversion]. (2024). Gynecologic Oncology Reports. https://doi.org/10.1016/j.gore.2024.101660