Table of Contents
How Protein in Urine Affects Your Health
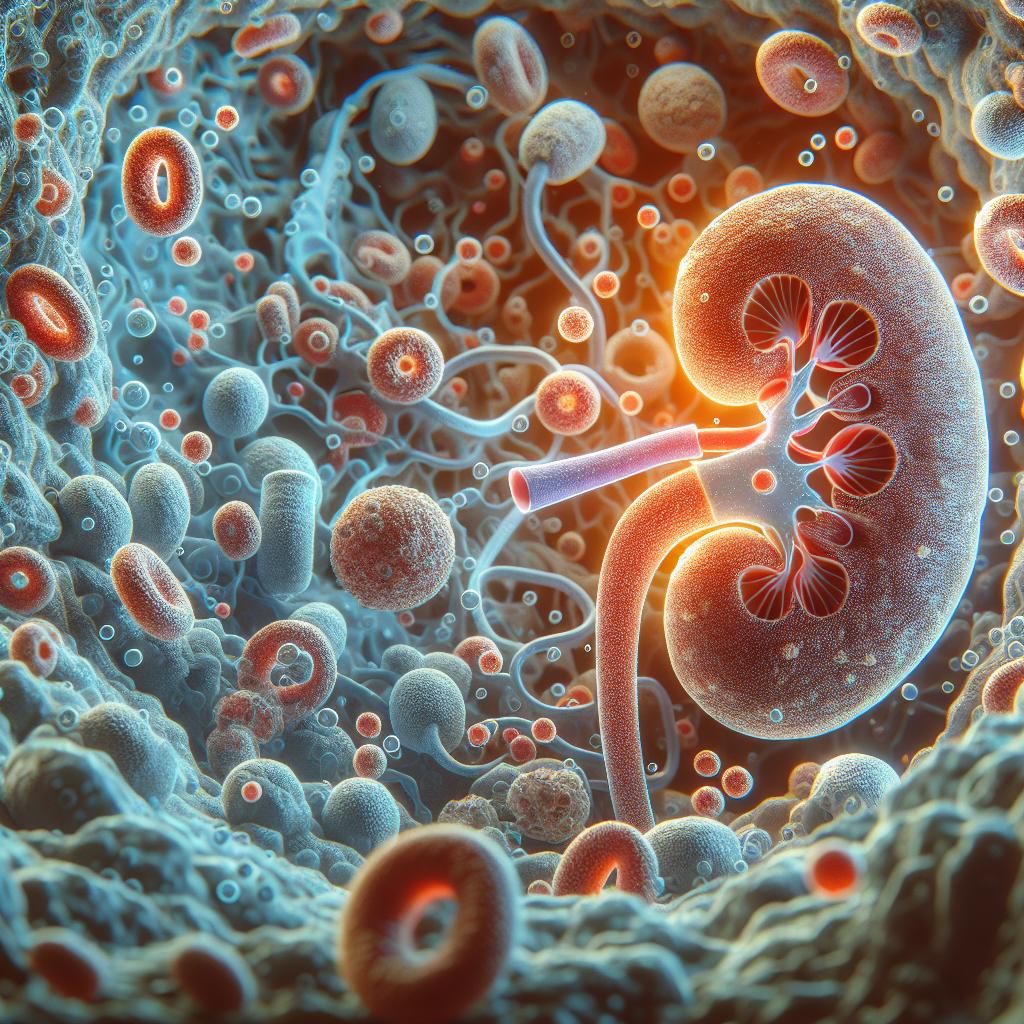
The presence of protein in urine, known as proteinuria, can be an early indicator of kidney dysfunction and other underlying health issues. Proteinuria may signal that the kidneys are not filtering blood properly, allowing proteins such as albumin to leak into the urine. This condition can have significant health implications, including an increased risk of cardiovascular disease and kidney failure. Studies show that persistent proteinuria correlates with a higher risk of chronic kidney disease (CKD) progression (Kettunen et al., 2021). Moreover, protein in urine can reflect systemic conditions, such as diabetes and hypertension, which contribute to kidney damage over time.
Elevated protein levels can lead to complications like edema, high blood pressure, and decreased kidney function. The kidneys typically filter out waste products while retaining essential proteins; thus, their impairment may indicate more serious health concerns. In this context, monitoring protein levels in urine is crucial for early diagnosis and intervention.
Common Causes of High Protein Levels in Urine
Several factors can contribute to increased protein levels in urine. These include:
- Kidney Disease: Conditions such as glomerulonephritis, diabetic nephropathy, and hypertension can damage the kidneys’ filtering units, leading to protein leakage.
- Dehydration: A concentrated urine sample can result in higher protein readings.
- Infections: Urinary tract infections (UTIs) can temporarily elevate protein levels due to inflammation.
- Exercise: Strenuous physical activity can lead to transient proteinuria.
- Medications: Certain drugs, particularly nonsteroidal anti-inflammatory drugs (NSAIDs) and some antibiotics, can affect kidney function and protein levels.
Understanding the underlying causes of proteinuria is essential for developing effective management strategies. For instance, addressing hypertension or diabetes can significantly reduce proteinuria and improve kidney health (Mountjoy et al., 2018).
Lifestyle Changes to Lower Protein in Urine
Implementing lifestyle changes can play a significant role in managing protein levels in urine. Key strategies include:
- Hydration: Maintaining adequate fluid intake helps dilute urine, potentially lowering protein concentration.
- Weight Management: Achieving and maintaining a healthy weight can reduce the risk of diabetes and hypertension, which are linked to proteinuria.
- Exercise: Regular physical activity improves cardiovascular health and can help manage blood pressure and diabetes, thus protecting kidney function.
- Stress Management: Chronic stress can negatively affect blood pressure and kidney health. Techniques such as yoga, meditation, and mindfulness can be beneficial.
Incorporating these lifestyle changes can create a holistic approach to reducing protein levels in urine and improving overall health outcomes.
Dietary Adjustments for Reducing Protein in Urine
Dietary modifications are crucial in managing proteinuria. Some effective dietary strategies include:
- Reducing Sodium Intake: High sodium levels can lead to hypertension, worsening kidney function. It’s advisable to limit processed foods and added salt.
- Increasing Fruits and Vegetables: A diet rich in fruits and vegetables can provide antioxidants and fiber, promoting kidney health and reducing inflammation (Heileson et al., 2021).
- Limiting Protein Intake: In some cases, reducing dietary protein can alleviate the kidneys’ workload. However, this should be done under medical supervision.
- Healthy Fats: Incorporating sources of omega-3 fatty acids, such as fatty fish and flaxseeds, may benefit kidney function and reduce inflammation.
These dietary adjustments can help manage protein levels in urine while promoting overall kidney health.
Medical Treatments and Interventions for Proteinuria
When lifestyle and dietary changes are insufficient, medical interventions may be necessary. Treatments may include:
- Medications: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) are often prescribed to lower blood pressure and reduce proteinuria.
- Diuretics: These can help manage fluid retention associated with kidney dysfunction.
- Control of Underlying Conditions: Effective management of diabetes and hypertension is critical in reducing proteinuria. Regular monitoring and adherence to treatment plans can lead to significant improvements.
- Dialysis or Transplantation: In cases of severe kidney failure, dialysis or kidney transplantation may be required.
Collaboration with healthcare professionals is essential in determining the most effective treatment plan for individuals with proteinuria.
Monitoring and Managing Protein Levels in Urine
Regular monitoring of protein levels in urine is vital for individuals at risk of kidney disease. This can involve:
- Routine Urinalysis: Periodic testing can help detect changes in protein levels and kidney function.
- Blood Pressure Monitoring: Keeping track of blood pressure is crucial, as hypertension can worsen proteinuria.
- Blood Sugar Control: For individuals with diabetes, maintaining optimal blood sugar levels is essential for kidney health.
Outcomes can be significantly improved through vigilant monitoring and proactive management strategies, allowing for timely interventions to prevent further kidney damage.
Table 1: Monitoring Parameters for Proteinuria Management
| Parameter | Recommended Frequency |
|---|---|
| Urinalysis | Annually or biannually |
| Blood pressure | At each medical visit |
| HbA1c for diabetics | Every 3-6 months |
| Kidney function tests | As advised by physician |
FAQ
What are the symptoms of proteinuria?
Proteinuria often has no symptoms. However, symptoms may include swelling in the legs, ankles, or around the eyes, foamy urine, and fatigue.
How is proteinuria diagnosed?
Proteinuria is diagnosed through a urinalysis, which measures the amount of protein in urine. Additional tests may be needed to assess kidney function.
Can proteinuria be reversed?
In many cases, proteinuria can be managed or reversed by treating the underlying cause, such as diabetes or hypertension, and making lifestyle changes.
Is proteinuria serious?
Persistent proteinuria can be a sign of kidney disease and may lead to complications. Early detection and management are crucial to prevent further damage.
How often should I monitor protein levels in urine?
Individuals at risk of kidney disease should have their protein levels monitored regularly, typically as part of routine health check-ups or as advised by a healthcare provider.
References
-
Kettunen, O., Ihalainen, J. K., Ohtonen, O., Valtonen, M., Mursu, J., & Linnamo, V. (2021). Energy availability during training camp is associated with signs of overreaching and changes in performance in young female cross-country skiers. Biomedical Human Kinetics, 13(1), 246-254. https://doi.org/10.2478/bhk-2021-0030
-
Mountjoy, M., Sundgot-Borgen, J., Burke, L., Carter, S., Constantini, N., Lebrun, C., Meyer, N., Sherman, R., Steffen, K., & Budgett, R. (2018). IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. British Journal of Sports Medicine, 52(11), 678-679
-
Heileson, J. L., Anzalone, A. J., Carbuhn, A. F., Askow, A. T., Stone, J. D., Turner, S. M., Hillyer, L. M., Ma, D. W. L., Luedke, J. A., & Jagim, A. R. (2021). The effect of omega-3 fatty acids on a biomarker of head trauma in NCAA football athletes: a multi-site, non-randomized study. Journal of the International Society of Sports Nutrition, 18(1), 65
-
Kettunen, O., Ihalainen, J. K., Ohtonen, O., Valtonen, M., Mursu, J., & Linnamo, V. (2021). Energy availability during training camp is associated with signs of overreaching and changes in performance in young female cross-country skiers. Biomedical Human Kinetics, 13(1), 246-254. https://doi.org/10.2478/bhk-2021-0030
-
Mountjoy, M., Sundgot-Borgen, J., Burke, L., Carter, S., Constantini, N., Lebrun, C., Meyer, N., Sherman, R., Steffen, K., & Budgett, R. (2018). IOC consensus statement on relative energy deficiency in sport (RED-S): 2018 update. British Journal of Sports Medicine, 52(11), 678-679