Table of Contents
How Protein in Urine Affects Your Health
The presence of protein in urine can indicate underlying health issues, particularly kidney dysfunction. The kidneys’ primary role is to filter waste products from the bloodstream while retaining essential proteins. When the kidneys are damaged or diseased, they may allow proteins, primarily albumin, to leak into the urine. Prolonged proteinuria can lead to serious health issues, including:
- Kidney Damage: Persistent protein leakage can exacerbate kidney damage, leading to chronic kidney disease (CKD).
- Cardiovascular Risks: Individuals with proteinuria are at a heightened risk for cardiovascular diseases, including hypertension and heart failure.
- Nutritional Deficiencies: Loss of protein can result in nutritional deficiencies which can weaken the immune system and lead to muscle wasting.
- Edema: Protein loss can lead to fluid retention and swelling due to a decrease in oncotic pressure in the blood.
Recognizing and addressing proteinuria is vital for preventing these severe health issues.
Common Causes of Proteinuria
Understanding the causes of proteinuria is essential for addressing the issue effectively. Common causes include:
- Diabetes Mellitus: High glucose levels can damage the kidney’s filtering units, leading to protein leakage (Cohen & Weinstein, 2018).
- Hypertension: High blood pressure can cause damage to the kidneys, resulting in proteinuria.
- Infections: Urinary tract infections (UTIs) can temporarily increase protein levels in urine.
- Kidney Diseases: Conditions such as glomerulonephritis and nephrotic syndrome specifically target kidney function and can cause significant protein loss.
- Medications: Certain medications, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), can induce kidney damage, leading to proteinuria.
- Exercise: Strenuous physical activity can lead to transient proteinuria, known as exercise-induced proteinuria.
Identifying the underlying cause is crucial for tailoring appropriate treatment strategies.
Lifestyle Changes to Reduce Protein in Urine
Making specific lifestyle changes can significantly help manage protein levels in urine. Here are some effective strategies:
-
Maintain Healthy Blood Sugar Levels: For individuals with diabetes, keeping blood sugar levels within target ranges is essential to prevent kidney damage. Regular monitoring and adherence to prescribed medications can help achieve this goal.
-
Control Blood Pressure: Managing hypertension through dietary changes, exercise, and medications can reduce kidney strain and minimize proteinuria.
-
Stay Hydrated: Adequate water intake helps maintain kidney function and dilute urine, which may help reduce protein concentration.
-
Limit Alcohol and Tobacco Use: Both substances can exacerbate kidney problems, leading to increased proteinuria.
-
Regular Exercise: Engaging in moderate physical activity can improve overall health, help control blood pressure, and manage weight, thus benefiting kidney function.
Dietary Adjustments for Managing Proteinuria
Diet plays a significant role in managing proteinuria. The following dietary adjustments can be beneficial:
-
Low-Protein Diet: Reducing protein intake may lessen the workload on the kidneys. For those with advanced kidney disease, a healthcare provider may recommend a protein-restricted diet.
-
Increase Fruits and Vegetables: A diet rich in fruits and vegetables can help reduce inflammation and support kidney health due to their antioxidant properties.
-
Limit Sodium Intake: Reducing salt intake can help control blood pressure and prevent fluid retention, which is particularly important for individuals with kidney issues.
-
Healthy Fats: Incorporating sources of healthy fats, such as olive oil and fish, can help improve overall health without putting excess stress on the kidneys.
-
Hydration: Drinking adequate fluids, particularly water, can help kidneys filter waste more effectively.
-
Monitor Potassium and Phosphorus: High levels of potassium and phosphorus can be harmful in kidney disease; thus, monitoring and adjusting their intake may be necessary.
Table 1: Dietary Recommendations for Reducing Protein in Urine
| Food Group | Recommendations |
|---|---|
| Proteins | Limit intake; prioritize plant-based proteins |
| Fruits & Vegetables | Aim for 5-7 servings a day |
| Sodium | Limit to < 2,300 mg/day |
| Healthy Fats | Include olive oil, nuts, and fish |
| Fluids | Stay hydrated with water, limit sugary drinks |
| Potassium & Phosphorus | Monitor and adjust intake based on kidney function |
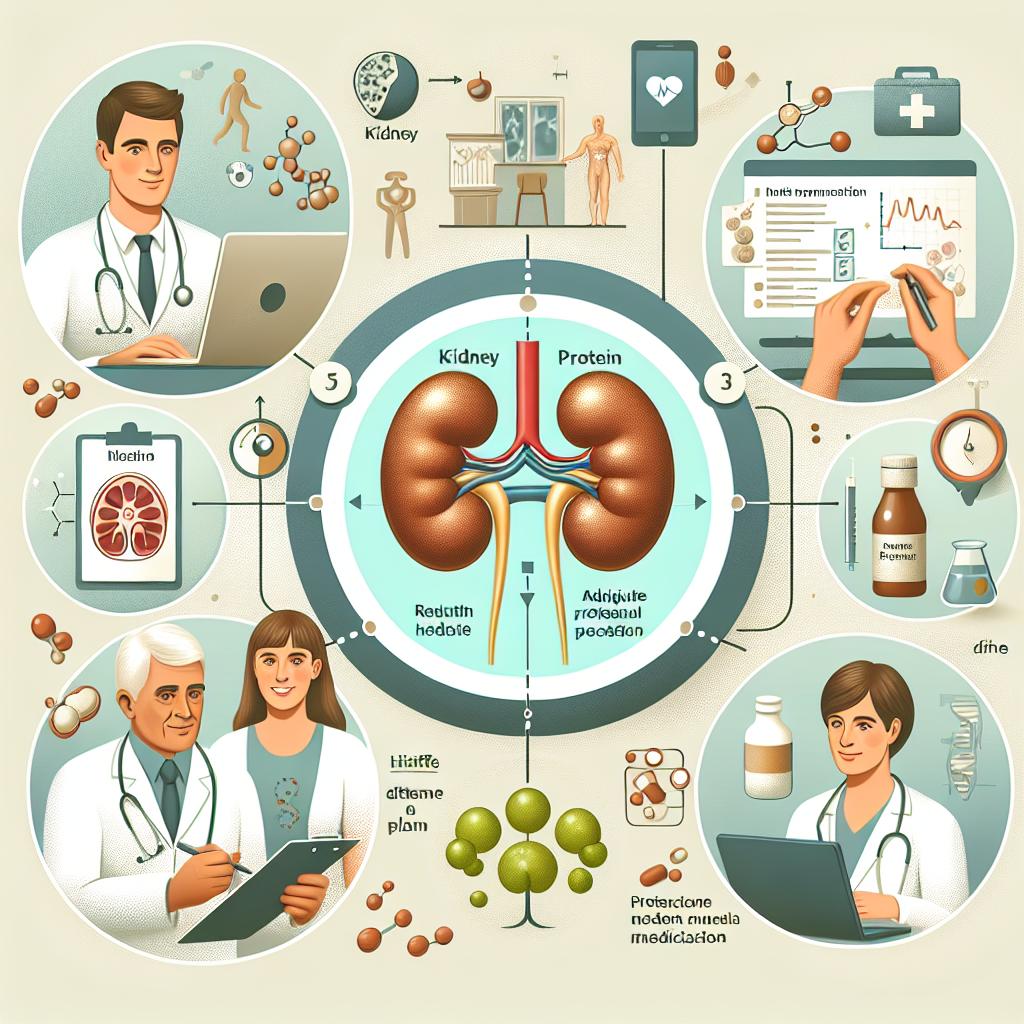
Medical Treatments and Interventions for Protein in Urine
In some cases, lifestyle and dietary changes may not be sufficient to manage proteinuria, and medical interventions might be necessary. Here are some treatments to consider:
-
Medications: Angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs) can help control proteinuria and protect kidney function in patients with diabetes and hypertension.
-
Immunosuppressive Agents: In cases of autoimmune disorders affecting the kidneys, immunosuppressive medications may be required.
-
Dialysis: For patients with severe kidney failure, dialysis may become necessary to filter waste products from the blood.
-
Kidney Transplant: In cases of end-stage renal disease, a kidney transplant may be the only viable option to restore kidney function.
-
Regular Monitoring: Regular check-ups and urine tests are essential for monitoring protein levels and kidney function over time.
Frequently Asked Questions (FAQ)
What is proteinuria?
Proteinuria is the presence of an abnormal amount of protein in the urine, which can be a sign of kidney damage or disease.
What causes protein to leak into urine?
Several factors can cause proteinuria, including diabetes, hypertension, kidney diseases, infections, and certain medications.
How can I reduce protein in urine naturally?
Lifestyle changes such as maintaining a healthy diet, managing blood sugar and blood pressure, staying hydrated, and engaging in regular exercise can help reduce protein levels in urine.
When should I see a doctor about proteinuria?
If you experience symptoms such as swelling, fatigue, or changes in urination patterns, or if you have risk factors for kidney disease, you should consult your healthcare provider.
Can diet affect proteinuria?
Yes, dietary changes such as reducing protein intake, increasing fruits and vegetables, and limiting sodium can significantly impact protein levels in urine.
References
-
Cohen, E., & Weinstein, A. (2018). The role of cannabinoids in the treatment of chronic pain. Phytocannabinoids and synthetic cannabinoids: from recreational consumption to potential therapeutic use – a review. Retrieved from https://doi.org/10.3389/ftox.2024.1495547
-
Zolfi, E., Khaleghi Mehr, F., Emtiazi, N., & Moradi, Y. (2025). A review of the carcinogenic potential of human papillomavirus (HPV) in urological cancers. Biomed Central. Retrieved from https://doi.org/10.1186/s12985-025-02682-1
-
Naga, N. G., El-Badan, D. E., Rateb, H. S., Ghanem, K. M., & Shaaban, M. I. (2025). Innovative application of ceftriaxone as a quorum sensing inhibitor in Pseudomonas aeruginosa. Scientific Reports. Retrieved from https://doi.org/10.1038/s41598-025-87609-0
-
Aboulwafa, M. M., Mostafa, N. M., Youssef, F. S., Eldahshan, O. A., & Singab, A. N. (2025). Lavandula dentata leaves as potential natural antibiofilm agents against Pseudomonas aeruginosa. Scientific Reports. Retrieved from https://doi.org/10.1038/s41598-025-88824-5
-
ZBiotics ameliorates T2DM-induced histopathological damage in liver, kidney and adipose tissues by modulating the NOD-like receptor signaling in Wistar rats. (2025). BMC Endocrine Disorders. Retrieved from https://doi.org/10.1186/s13098-025-01600-3
-
The exploration of therapeutic potential of bioflavonoids in metabolic acidosis and inflammation-associated with acute kidney injury: Therapeutic potential of bioflavonoids in acute kidney injury. (2023). Retrieved from https://pubmed.ncbi.nlm.nih.gov/11877053/
-
Emerging Elastic Micro-Nano Materials for Diagnosis and Treatment of Thrombosis. (2023). Retrieved from https://pubmed.ncbi.nlm.nih.gov/11868703/