Table of Contents
Importance of Addressing Mixed Urogenital Flora
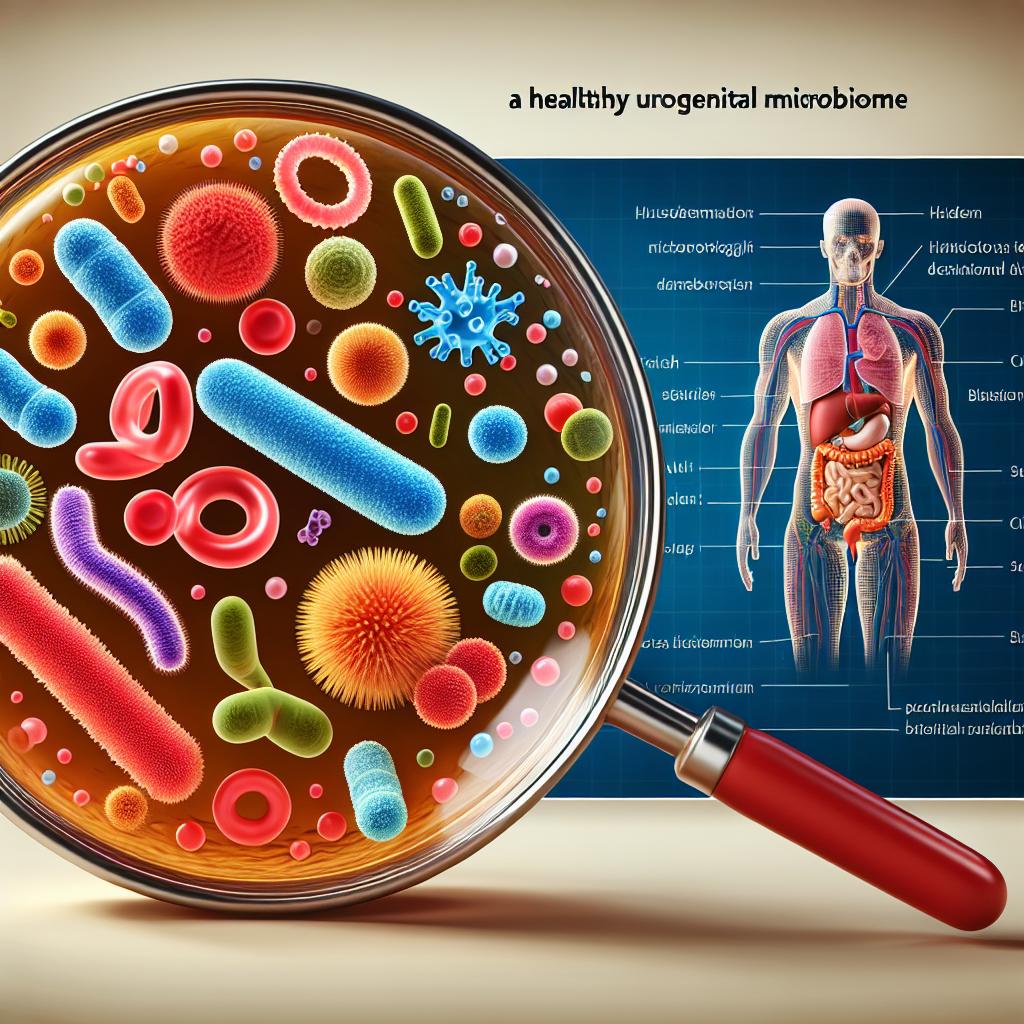
Mixed urogenital flora refers to the presence of various bacteria and microorganisms in the urogenital tract, which can disrupt the natural balance necessary for healthy function. This imbalance can result in conditions such as bacterial vaginosis, recurrent UTIs, and even pelvic inflammatory disease. A study indicated that more than 404.6 million people globally suffer from urinary tract infections, with women being disproportionately affected due to anatomical reasons (Zeng et al., 2022).
Addressing mixed urogenital flora is essential for several reasons:
- Preventing Infections: A balanced microbiome can help prevent pathogenic bacteria from colonizing the urogenital tract, thereby reducing the risk of infections.
- Promoting Reproductive Health: Maintaining a healthy urogenital flora is crucial for fertility and pregnancy outcomes, as infections can lead to complications during these stages.
- Enhancing Quality of Life: Persistent infections and discomfort associated with mixed flora can significantly impact a person’s quality of life, including physical, emotional, and social aspects.
Symptoms Indicating Mixed Urogenital Flora Issues
Recognizing the symptoms of mixed urogenital flora issues is the first step towards effective treatment. Common symptoms include:
- Unusual Discharge: Changes in the color, odor, or consistency of vaginal discharge can indicate an imbalance in the urogenital flora. An increase in foul-smelling discharge may suggest bacterial vaginosis (Chieng et al., 2024).
- Painful Urination: Dysuria or pain during urination is a classic symptom of UTIs and can also be associated with mixed flora conditions.
- Pelvic Pain: Chronic pelvic pain, especially when accompanied by other symptoms, may signal underlying infections or inflammation due to mixed flora.
- Frequent Urination: Increased urgency and frequency of urination can indicate a UTI, which is often linked to the presence of pathogenic bacteria (Foxman et al., 2003).
- Fever and Systemic Symptoms: In some cases, systemic symptoms like fever may accompany local symptoms, indicating a more severe infection or inflammatory response.
Treatment Options for Mixed Urogenital Flora
Effective management of mixed urogenital flora typically involves a multifaceted treatment approach. The following options are commonly recommended:
-
Antibiotic Therapy: While antibiotics are the first line of defense against bacterial infections, their overuse can lead to antibiotic resistance and disrupt the natural flora. Therefore, careful selection and use of antibiotics are critical (Sihra et al., 2018).
-
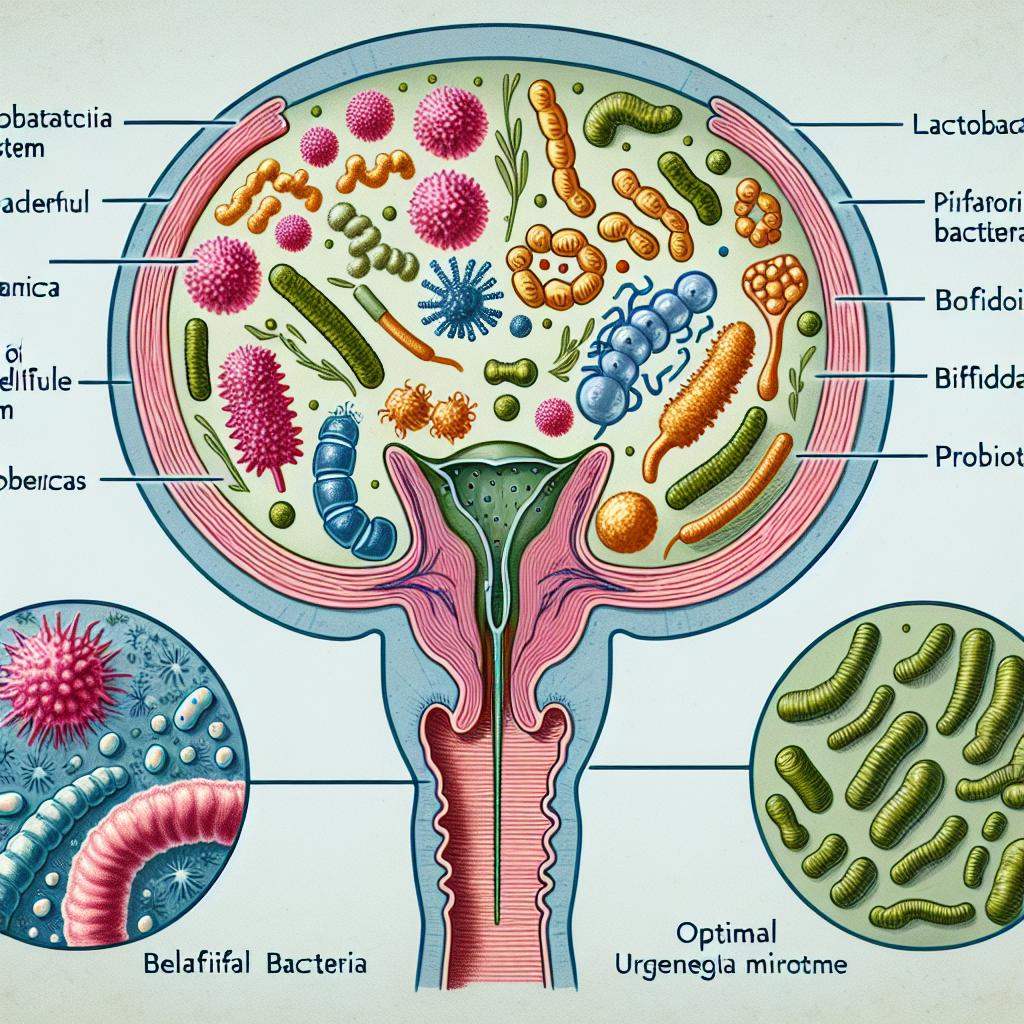
Probiotics: The use of probiotics has gained attention as a beneficial strategy in managing mixed urogenital flora. Probiotics can help restore the natural balance of bacteria in the urogenital tract. Research indicates that specific strains of Lactobacillus can reduce the incidence of UTIs by enhancing the diversity of the vaginal microbiota and inhibiting pathogen adherence (Saraiva et al., 2025).
-
Dietary Changes: Incorporating foods rich in prebiotics and probiotics can support urogenital health. Foods such as yogurt, kefir, and fermented vegetables can promote the growth of beneficial bacteria. A balanced diet rich in fruits, vegetables, and whole grains can also enhance overall immune function (Kranz et al., 2022).
-
Hormonal Treatments: For postmenopausal women, hormone replacement therapy may help restore vaginal flora by alleviating dryness and promoting a healthy environment (Zhu et al., 2022).
-
Personal Hygiene Practices: Maintaining good hygiene practices, such as proper wiping techniques and the use of unscented products, can help prevent the introduction of pathogens into the urogenital tract.
Table 1: Common Treatment Options for Mixed Urogenital Flora
| Treatment Option | Description |
|---|---|
| Antibiotic Therapy | Targeting specific pathogens with prescribed antibiotics. |
| Probiotics | Administration of beneficial bacteria to restore balance. |
| Dietary Changes | Incorporating prebiotics and probiotics through food sources. |
| Hormonal Treatments | Use of hormone replacement therapy to restore vaginal health. |
| Personal Hygiene | Maintaining cleanliness to avoid infections. |
Role of Probiotics in Mixed Urogenital Flora Management
Probiotics play a significant role in the management of mixed urogenital flora. They help restore the natural balance of the microbiome and enhance the body’s immune response. Here’s how probiotics work:
- Competition with Pathogens: Probiotics can inhibit the growth of pathogenic bacteria by competing for nutrients and binding sites in the urogenital tract (Saraiva et al., 2025).
- Production of Antimicrobial Substances: Certain probiotic strains produce substances, such as hydrogen peroxide and bacteriocins, which can directly inhibit the growth of harmful bacteria (Gupta et al., 2017).
- Immune Modulation: Probiotics can enhance mucosal immunity by promoting the secretion of immunoglobulin A (IgA) and modulating the activity of immune cells (New et al., 2022).
Table 2: Benefits of Probiotics in Urogenital Health
| Benefit | Mechanism of Action |
|---|---|
| Inhibition of Pathogens | Compete for resources and attachment sites. |
| Antimicrobial Activity | Produce substances that inhibit pathogenic growth. |
| Immune Enhancement | Stimulate immune response and promote antibody production. |
Dietary Interventions to Support Urogenital Health
Dietary interventions can significantly influence urogenital flora and overall health. Here are some key dietary strategies:
-
Increase Fiber Intake: Consuming a high-fiber diet can promote the growth of beneficial gut bacteria and enhance the production of short-chain fatty acids (SCFAs), which have anti-inflammatory properties (Džidić-Krivić et al., 2025).
-
Incorporate Fermented Foods: Foods such as yogurt, kimchi, and sauerkraut are rich in probiotics and can help maintain a healthy balance of bacteria in the urogenital tract (Kranz et al., 2022).
-
Limit Sugars and Processed Foods: High sugar and processed food intake can promote the growth of pathogenic bacteria, thus disrupting the balance of the microbiota (Zhu et al., 2022).
-
Hydration: Adequate fluid intake is crucial for urinary health, as it helps flush out bacteria and maintain mucosal integrity (Guay, 2009).
Table 3: Dietary Recommendations for Urogenital Health
| Dietary Component | Recommended Action |
|---|---|
| Fiber | Increase intake through fruits, vegetables, and whole grains. |
| Fermented Foods | Include yogurt, kefir, and kimchi regularly. |
| Reduce Sugar | Limit processed foods and added sugars. |
| Hydration | Drink sufficient fluids daily to promote urinary health. |
FAQ
What are mixed urogenital flora issues? Mixed urogenital flora issues refer to an imbalance of bacteria and microorganisms in the urogenital tract, which can lead to infections such as UTIs and bacterial vaginosis.
How can I tell if I have a UTI? Symptoms of a UTI may include painful urination, frequent urge to urinate, cloudy or foul-smelling urine, and pelvic pain.
Can probiotics help with recurrent UTIs? Yes, specific probiotic strains, particularly Lactobacillus, have been shown to help prevent recurrent UTIs by restoring healthy vaginal flora and inhibiting pathogen growth.
What dietary changes can support urogenital health? A diet rich in fiber, fermented foods, and adequate hydration can help maintain a healthy balance of urogenital flora and support overall health.
What should I do if I suspect a UTI? If you suspect a UTI, consult a healthcare provider for diagnosis and appropriate treatment, including possibly antibiotics or probiotics.
References
-
Džidić-Krivić, A., Begagić, E., Hadžić, S., Bećirović, A., Bećirović, E., Hibić, H., … & Kadić Vukas, S. (2025). Unveiling the Important Role of Gut Microbiota and Diet in Multiple Sclerosis. Brain Sciences. https://doi.org/10.3390/brainsci15030253
-
Gupta, V., Nag, D., Garg, P. (2017). Recurrent Urinary Tract Infections in Women: How Promising Is the Use of Probiotics? Indian Journal of Medical Microbiology, 35(4), 347-354.
-
Kranz, J., Lackner, J., Künzel, U., Wagenlehner, F., Schmidt, S. (2022). Plant-Based Foods and their Role in the Management of Urinary Tract Infections. Nutrients, 14(10), 2204
-
New, F. J., Theivendrampillai, S., Julliebø-Jones, P., Somani, B. (2022). The Role of Probiotics for Recurrent UTIs in the Twenty-First Century: A Systematic Review of Literature. Current Urology Reports, 23(12), 98.
-
Saraiva, A., Raheem, D., Poly Rani, R., Mowyna, M. N., Romão, B., … & Raposo, A. (2025). Probiotics and Plant-Based Foods as Preventive Agents of Urinary Tract Infection: A Narrative Review of Possible Mechanisms Related to Health. Nutrients, 17(6), 986. https://doi.org/10.3390/nu17060986
-
Sihra, N., Goodman, A., Zakri, R., Sahai, A., Malde, S. (2018). Nonantibiotic Prevention and Management of Recurrent Urinary Tract Infection. Nature Reviews Urology, 15(11), 677-686.
-
Zeng, Z., Zhan, J., Zhang, K., Chen, H., Cheng, S. (2022). Global, Regional, and National Burden of Urinary Tract Infections from 1990 to 2019: An Analysis of the Global Burden of Disease Study 2019. World Journal of Urology, 40(5), 757-763.