Table of Contents
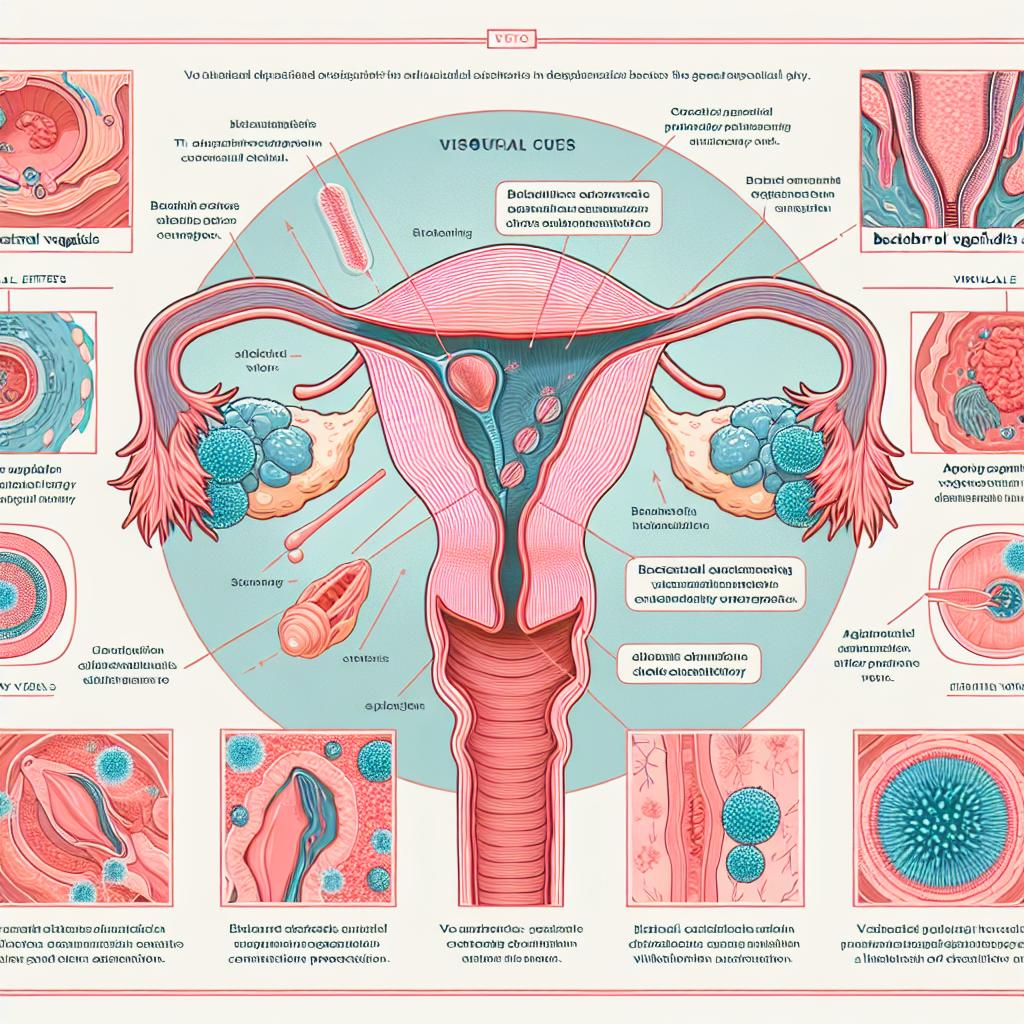
Symptoms to Identify UTI and Yeast Infection
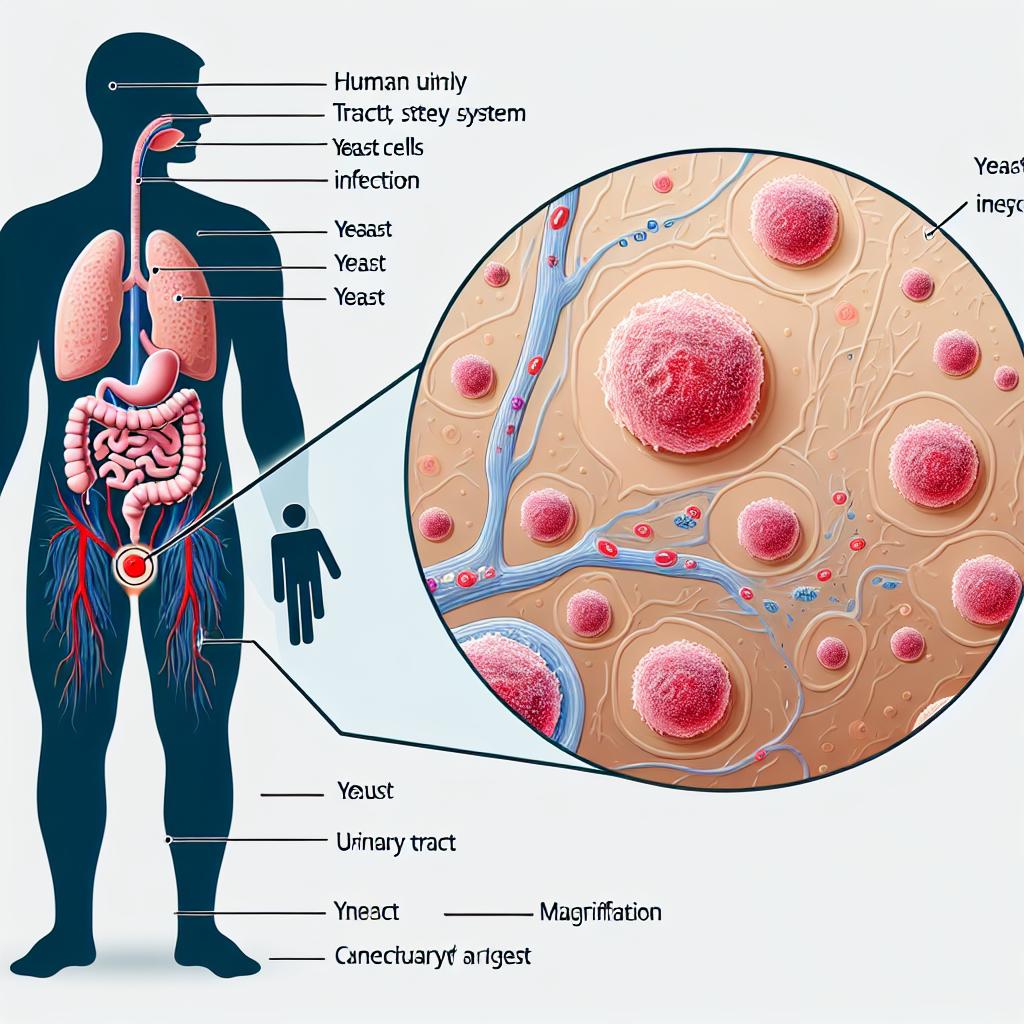
Urinary Tract Infections (UTIs):
UTIs can affect any part of the urinary system, including the bladder, urethra, ureters, and kidneys. Common symptoms include:
- Frequent Urination: A strong urge to urinate often, even if little urine is produced.
- Burning Sensation: Pain or a burning feeling during urination.
- Cloudy or Strong-Smelling Urine: Changes in the appearance and odor of urine can indicate infection.
- Pelvic Pain: Discomfort in the lower abdomen or pelvic region.
- Blood in Urine: Hematuria, or blood in urine, can be a serious symptom of a UTI.
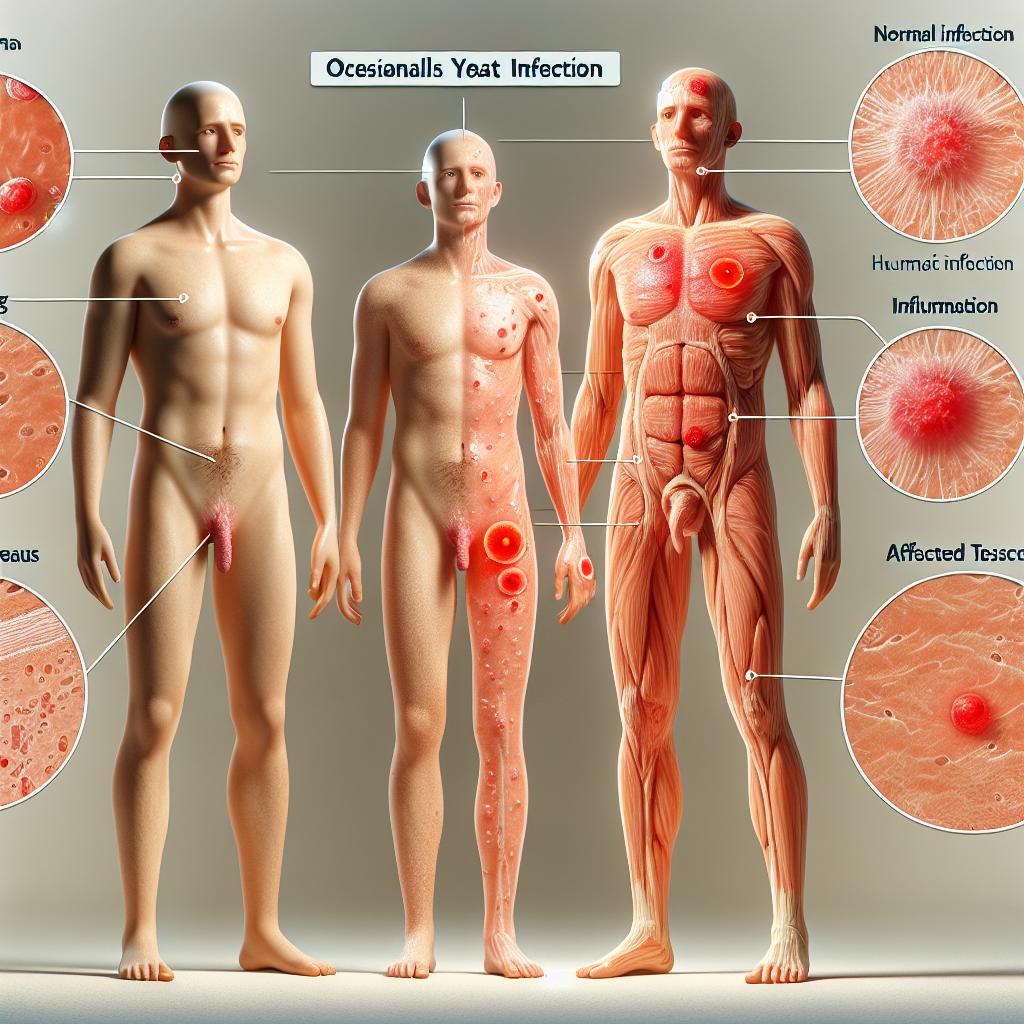
Yeast Infections:
Yeast infections primarily affect women, although men can also be affected. Typical symptoms include:
- Itching and Irritation: Persistent itching in the vaginal area.
- Thick, White Discharge: Often resembling cottage cheese, this discharge is typically odorless.
- Redness and Swelling: Inflammation of the vulva and vaginal walls.
- Pain During Intercourse: Discomfort or pain during sexual activity.
- Burning Sensation: Similar to UTIs, a burning sensation may occur during urination.
Understanding these symptoms can help in early identification and treatment, reducing the risk of complications.
Common Causes of UTI and Yeast Infection
Causes of UTIs:
- Bacterial Infection: The most common cause of UTIs is the bacterium Escherichia coli (E. coli), which normally resides in the intestines.
- Sexual Activity: Increased sexual activity can introduce bacteria into the urinary tract.
- Urinary Tract Obstruction: Conditions like kidney stones can block urine flow, leading to infections.
- Poor Hygiene: Inadequate personal hygiene can contribute to bacterial growth.
- Catheter Use: Catheters can introduce bacteria into the urinary tract.
Causes of Yeast Infections:
- Fungal Growth: The fungus Candida, particularly Candida albicans, is the primary cause of yeast infections.
- Antibiotic Use: Antibiotics can disrupt the natural balance of bacteria and yeast in the body, allowing yeast to overgrow.
- Hormonal Changes: Fluctuations in hormones, such as during menstruation or pregnancy, can predispose women to infections.
- High Sugar Levels: Elevated blood sugar levels can promote yeast growth, making diabetes a risk factor.
- Moist Environments: Warm, moist environments can facilitate fungal growth.
By recognizing these causes, individuals can take proactive steps to minimize their risk.
Preventative Measures for UTI and Yeast Infection
Preventing UTIs:
- Stay Hydrated: Drinking plenty of water helps flush bacteria from the urinary tract.
- Urinate Regularly: Avoid holding urine for prolonged periods.
- Wipe Front to Back: Proper hygiene can prevent the spread of bacteria from the anal area to the urethra.
- Urinate After Intercourse: This can help remove bacteria that may have entered the urinary tract during sex.
- Avoid Irritants: Products like douches, scented wipes, and harsh soaps can irritate the urethra.
Preventing Yeast Infections:
- Wear Breathable Underwear: Cotton underwear allows for better airflow, reducing moisture buildup.
- Limit Antibiotic Use: Use antibiotics only when necessary to prevent disrupting the natural flora.
- Avoid Douche and Scented Products: These can alter the vaginal environment and promote yeast overgrowth.
- Maintain a Healthy Diet: A balanced diet may help regulate blood sugar levels and maintain a healthy microbiome.
- Probiotics: Incorporating probiotics into the diet can help restore the natural balance of flora.
By implementing these preventative strategies, individuals can significantly reduce their risk of developing UTIs and yeast infections.
Treatment Options for UTI and Yeast Infection
Treatment for UTIs:
- Antibiotics: The primary treatment for UTIs is antibiotics, which should be prescribed by a healthcare provider. Common antibiotics include trimethoprim/sulfamethoxazole, nitrofurantoin, and fosfomycin.
- Pain Relief: Over-the-counter pain relievers may help alleviate discomfort.
- Hydration: Increasing fluid intake can help flush out the urinary tract.
Treatment for Yeast Infections:
- Antifungal Medication: Over-the-counter antifungal creams or suppositories (e.g., clotrimazole, miconazole) are effective for mild infections. For recurrent infections, a healthcare provider may prescribe oral antifungals like fluconazole.
- Lifestyle Changes: Maintaining dry and clean genital areas is essential for recovery and prevention of future infections.
Both conditions require prompt treatment to relieve symptoms and prevent complications.
When to Seek Medical Help for UTI and Yeast Infection
It is essential to see a healthcare provider if:
- Symptoms Persist: If UTI symptoms do not improve within a few days of treatment.
- Severe Symptoms: Experiencing high fever, chills, nausea, or vomiting.
- Recurrent Infections: Frequent UTIs or yeast infections may require further investigation.
- Blood in Urine: This symptom warrants immediate medical attention as it may indicate a more severe condition.
- Severe Itching or Discomfort: Persistent itching or discomfort from a yeast infection should be evaluated.
Timely medical intervention can prevent complications and ensure effective treatment.
FAQ
How can I naturally prevent UTIs?
Staying well-hydrated, practicing good hygiene, and urinating after intercourse can help prevent UTIs naturally.
Are there any home remedies to treat yeast infections?
Some people find relief with probiotics, yogurt containing live cultures, or coconut oil. However, it’s essential to consult with a healthcare provider for proper diagnosis and treatment.
Is it normal to have recurrent yeast infections?
While occasional yeast infections are common, recurrent infections (four or more per year) should be evaluated by a healthcare provider to rule out underlying issues.
Can I treat a UTI without antibiotics?
While some home remedies may provide relief, antibiotics are usually necessary to effectively treat a UTI.
References
-
Iwata, H. (2025). Association between prenatal exposure to maternal metal and trace elements and Streptococcus infection: A prospective birth cohort in the Japan Environment and Children’s Study. Retrieved from https://doi.org/10.1371/journal.pone.0319356
-
Mishra, S. K., et al. (2025). Exploratory algorithms to devise multi-epitope subunit vaccine by examining HIV-1 envelope glycoprotein: An immunoinformatics and viroinformatics approach. Retrieved from https://doi.org/10.1371/journal.pone.0318523
-
Araújo, S., Silva, V., Quintelas, M., Martins, Â., Igrejas, G., & Poeta, P. (2025). From soil to surface water: exploring Klebsiella’s clonal lineages and antibiotic resistance odyssey in environmental health. Retrieved from https://doi.org/10.1186/s12866-025-03798-8
-
Finley, R. L., et al. (2013). The scourge of antibiotic resistance: The important role of the environment. Clin Infect Dis
-
Banin, E., et al. (2017). Editorial: Bacterial pathogens, antibiotics and antibiotic resistance. FEMS Microbiol Rev