Table of Contents
Overview of UTI with Blood: Causes and Symptoms
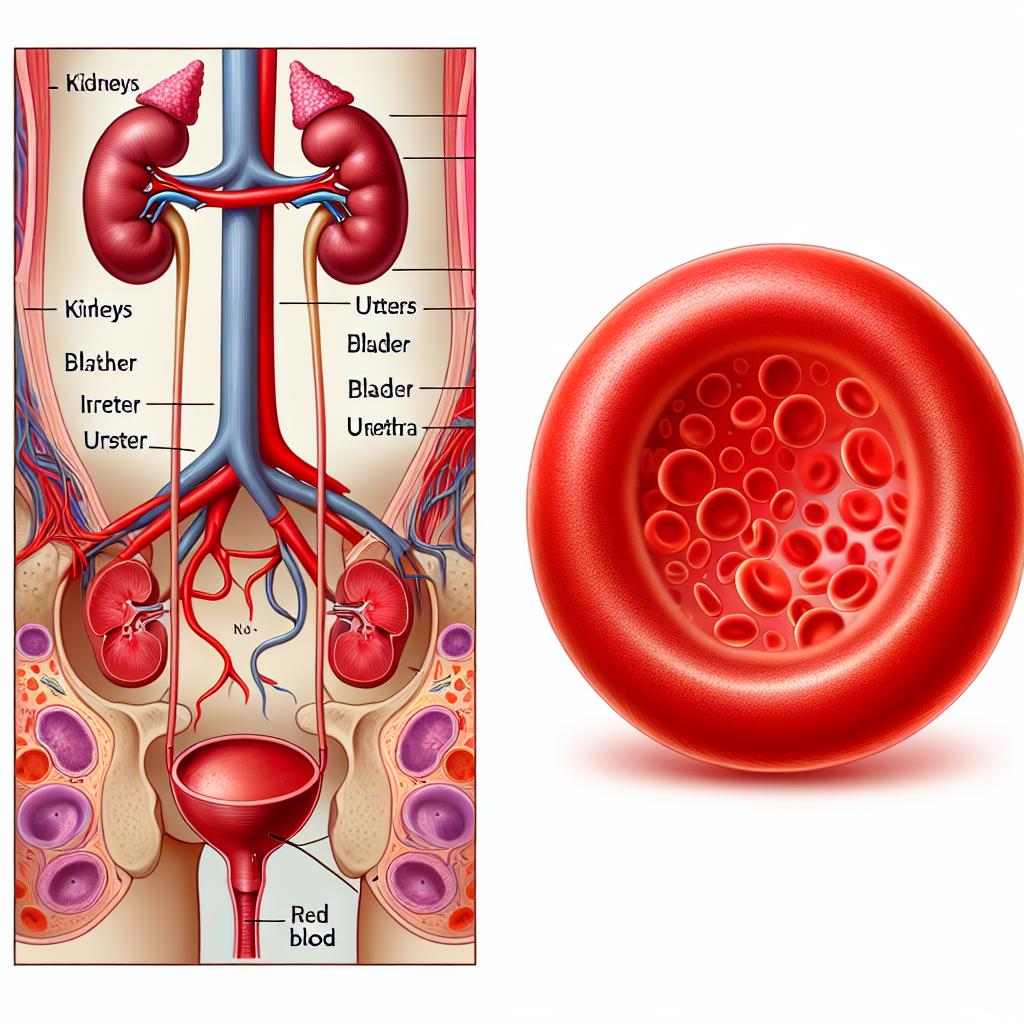
Urinary tract infections (UTIs) are one of the most common bacterial infections, particularly affecting women. The presence of blood in the urine, known as hematuria, can signify a more severe underlying condition. The primary causes of UTIs with blood presence include infections caused by bacteria such as Escherichia coli, trauma to the urinary tract, kidney stones, and malignancies in the urinary system (Gupta et al., 2025).
Common symptoms of UTIs include:
- Dysuria: Painful urination is a hallmark symptom.
- Increased frequency: Patients may feel the need to urinate more often, even with little output.
- Urgency: A strong, persistent urge to urinate often accompanies dysuria.
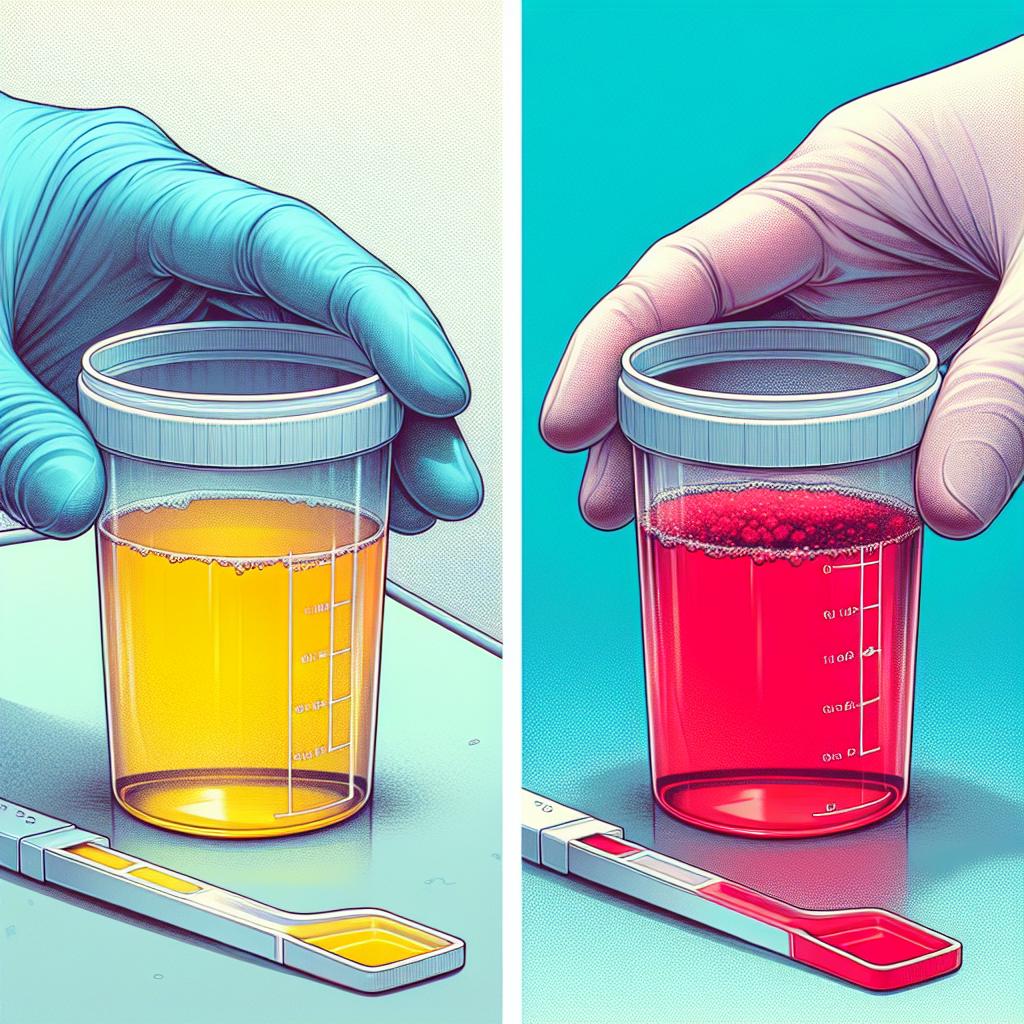
- Hematuria: The presence of blood can manifest as pink, red, or cola-colored urine.
- Flank pain: Pain in the side or back may indicate kidney involvement.
The positive predictive value of pyuria (presence of pus in urine) for diagnosing lower UTIs is approximately 90% when accompanied by the aforementioned symptoms (Gupta et al., 2025). However, differentiating between asymptomatic bacteriuria (ASB) and UTI can be challenging, particularly in vulnerable populations such as the elderly or those with cognitive impairments (Gupta et al., 2025).
Diagnostic Approaches for Identifying UTI with Blood
Diagnosing a UTI with blood involves a combination of clinical assessment and laboratory tests. The following diagnostic approaches are commonly used:
-
Urinalysis: A dipstick test can reveal the presence of leukocytes, nitrites, and red blood cells. Microscopic examination can confirm hematuria and pyuria.
-
Urine Culture: This test identifies the specific bacteria causing the infection and determines antibiotic susceptibility, which is crucial for effective treatment (Gupta et al., 2025).
-
Imaging Studies: If kidney stones or structural abnormalities are suspected, ultrasound or CT scans may be utilized. These imaging modalities help visualize the urinary tract’s anatomy and identify any obstructions or lesions.
-
Cystoscopy: In cases of recurrent Utis or persistent hematuria, cystoscopy may be performed to visualize the bladder and urethra directly, allowing for the identification of tumors or other abnormalities.
-
Blood Tests: A complete blood count (CBC) can help assess the degree of infection and kidney function tests can determine if there is any renal impairment due to the infection.
Treatment Options for UTI with Blood: Antibiotics and Beyond
Treatment of UTIs with blood presence primarily involves antibiotic therapy, tailored to the specific pathogen identified through urine cultures. The following treatment options are typically considered:
Antibiotic Therapy
-
First-Line Agents: Commonly prescribed antibiotics include nitrofurantoin, trimethoprim-sulfamethoxazole, and fosfomycin for uncomplicated UTIs. These agents are effective against the most common causative agents.
-
Fluoroquinolones: Ciprofloxacin and levofloxacin are often reserved for complicated or resistant cases due to their broad spectrum of activity but should be used cautiously due to potential side effects (Gupta et al., 2025).
-
Beta-lactams: Amoxicillin-clavulanate and cephalosporins are alternatives for patients with contraindications to first-line agents.
-
Empirical Therapy: In cases of severe symptoms or when initial cultures are pending, broad-spectrum intravenous antibiotics may be initiated.
Adjunctive Therapies
- Pain Management: Phenazopyridine can be used to relieve dysuria and bladder discomfort but should not replace antibiotic therapy.
- Hydration: Increased fluid intake is encouraged to dilute urine and promote flushing of the urinary tract.
- Urinary Antiseptics: Agents such as methenamine can be considered in recurrent cases to reduce bacterial load.
Preventive Measures for UTI with Blood in At-Risk Populations
Preventive strategies are crucial in at-risk populations to minimize the recurrence of UTIs with blood presence. These include:
-
Behavioral Modifications: Encouraging regular voiding and complete bladder emptying can significantly reduce UTI incidence.
-
Hygiene Practices: Teaching proper hygiene techniques, particularly post-coital voiding in women, can help prevent infections.
-
Prophylactic Antibiotics: For patients with recurrent UTIs, low-dose prophylactic antibiotics may be prescribed for a limited period.
-
Management of Contributing Conditions: Effective treatment of conditions such as diabetes mellitus, urinary retention, or anatomical abnormalities can reduce UTI frequency.
-
Education: Providing education on the signs and symptoms of UTIs can ensure prompt treatment, thus reducing complications associated with delayed care.
Long-Term Complications and Follow-Up Care for UTI with Blood
Long-term complications of untreated or recurrent UTIs can lead to significant morbidity. These may include:
-
Chronic Kidney Disease: Persistent infections can cause scarring and damage to the kidneys, leading to chronic renal impairment (Gupta et al., 2025).
-
Recurrent Infections: Patients may experience frequent Utis, necessitating ongoing management strategies.
-
Sepsis: Severe UTIs can progress to systemic infections, requiring hospitalization and aggressive treatment.
Follow-Up Care
Patients diagnosed with UTIs and blood presence should have regular follow-up appointments to monitor kidney function and ensure effective management of any underlying conditions. Repeat urinalysis and cultures may be warranted if symptoms recur. Education on lifestyle modifications and adherence to treatment regimens is essential for prevention.
| Complication | Description |
|---|---|
| Chronic Kidney Disease | Long-term damage leading to renal impairment. |
| Recurrent Infections | Increased frequency of UTIs requiring ongoing management. |
| Sepsis | Systemic infection requiring hospitalization and aggressive treatment. |
FAQ
What causes blood in urine with a UTI? Blood in urine during a UTI can be caused by inflammation of the bladder lining, kidney stones, or damage to the urinary tract from the infection itself.
How is a UTI with blood diagnosed? A UTI with blood is diagnosed through urinalysis, urine culture, imaging studies, and sometimes cystoscopy.
What are the treatment options for a UTI with blood? Treatment typically involves antibiotics tailored to the specific bacteria, pain management, and increased fluid intake.
Can UTIs with blood lead to serious complications? Yes, untreated UTIs with blood can lead to chronic kidney disease, recurrent infections, and sepsis.
How can I prevent recurrent UTIs? Preventive measures include maintaining proper hygiene, regular voiding, staying hydrated, and, in some cases, using prophylactic antibiotics.
References
- Gupta, K., Hooton, T. M., & Naber, K. (2025). Urinary tract infections: Diagnosis and management. Updates on HIV Pre-exposure Prophylaxis in Latin America: Available Drugs and Implementation Status. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11892447/
- Gupta, K., et al. (2025). Urine Leukocyte Counts for Differentiating Asymptomatic Bacteriuria From Urinary Tract Infection and Predicting Secondary Bacteremia. Journal of Korean Medical Science. Retrieved from https://doi.org/10.3346/jkms.2025.40.e30