Table of Contents
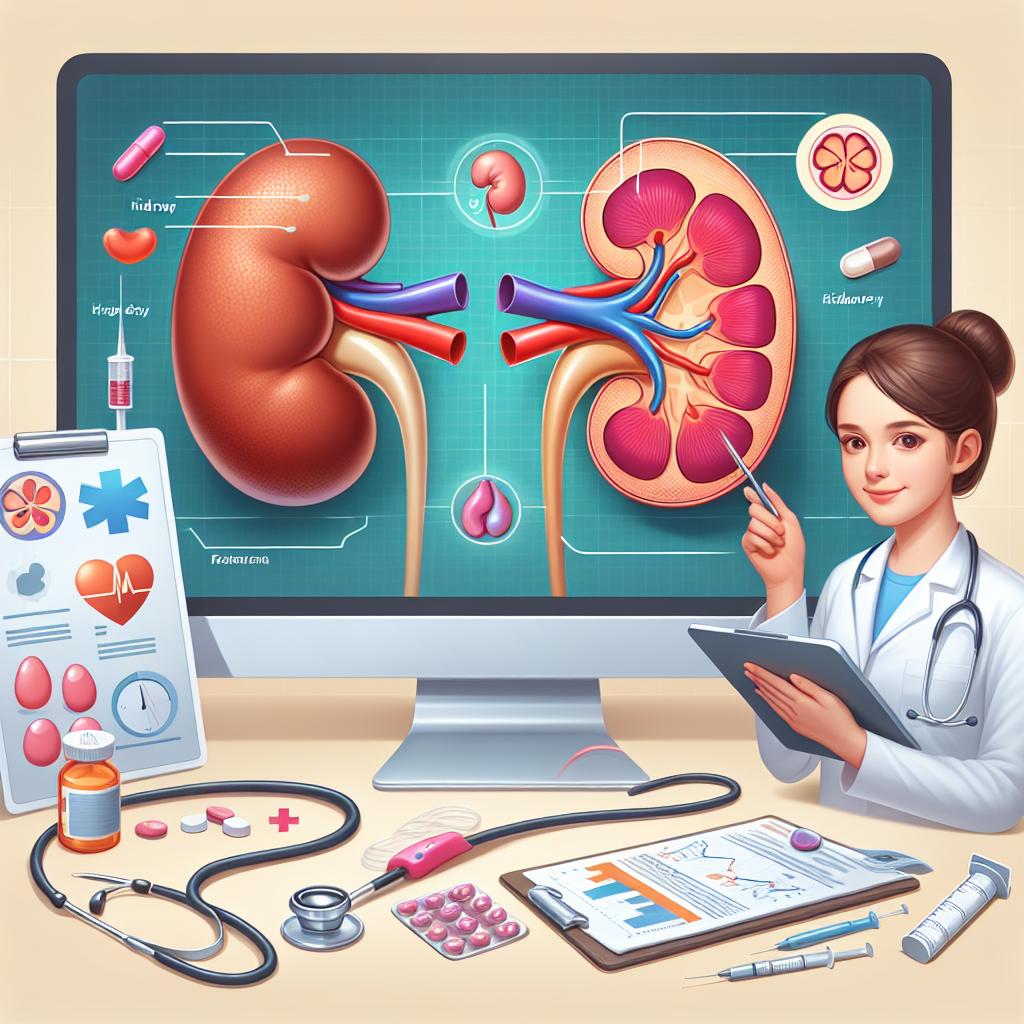
Overview of Stage 3a Kidney Disease: Symptoms and Diagnosis
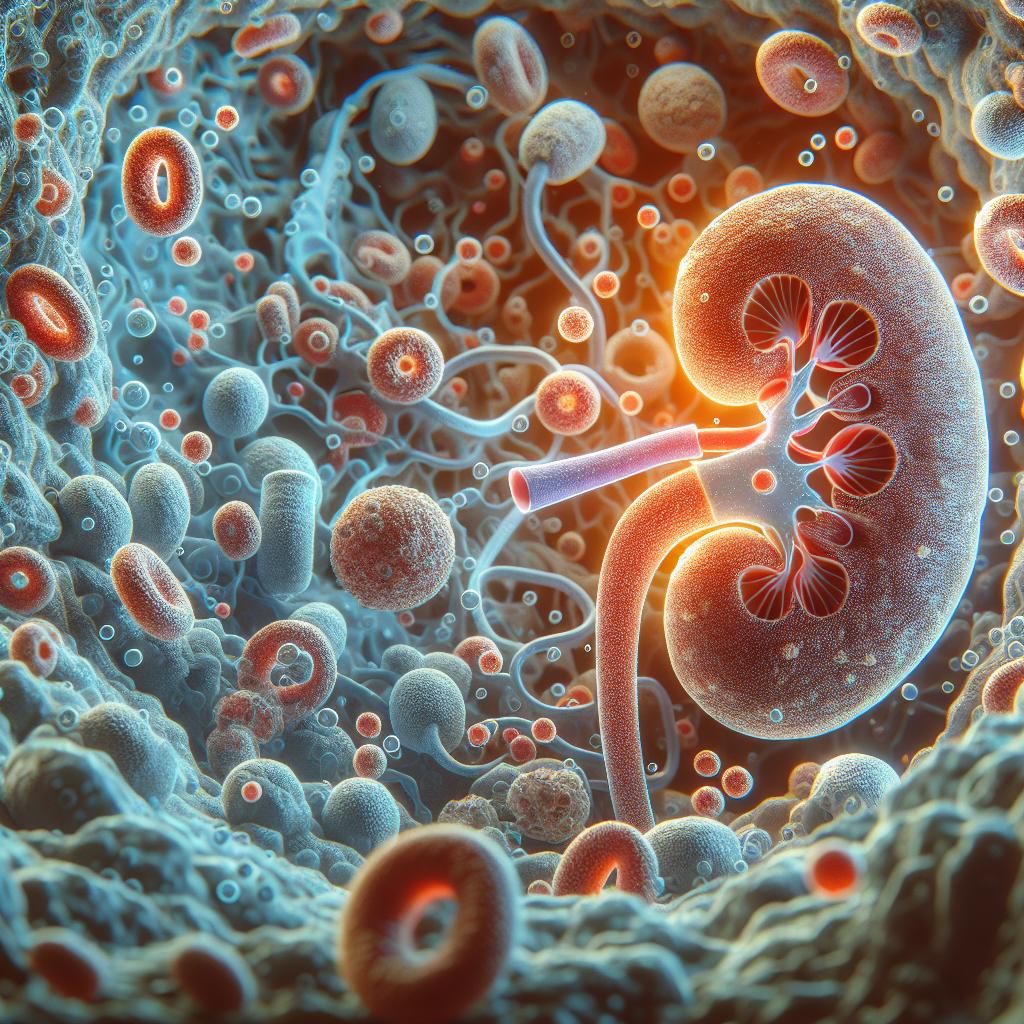
Stage 3a kidney disease is characterized by a moderate decline in kidney function, typically classified by an estimated Glomerular Filtration Rate (eGFR) between 45 and 59 mL/min. This stage often results in a range of symptoms, which can vary significantly among individuals. Common symptoms include fatigue, fluid retention leading to swelling (edema), changes in urination patterns, and anemia. Patients might also experience a buildup of waste products in the body, causing nausea and a general feeling of being unwell (Morrison et al., 2023).
Diagnosis of stage 3a kidney disease usually involves laboratory tests, including serum creatinine levels and urine tests to assess proteinuria. The presence of other conditions such as diabetes or hypertension is also considered, as these can exacerbate kidney damage. Imaging studies, such as ultrasounds, may be utilized to visualize kidney structure and rule out obstructions (Morrison et al., 2023). Early diagnosis is crucial as it allows for the implementation of management strategies aimed at slowing disease progression.
Treatment Options for Stage 3a Kidney Disease: What You Need to Know
Effective management of stage 3a kidney disease focuses on preserving kidney function and preventing complications. The treatment options available can be categorized into pharmacological and non-pharmacological strategies.
Pharmacological Strategies
Patients may be prescribed medications to control underlying conditions such as hypertension and diabetes. Angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) are often recommended to help protect kidney function by lowering blood pressure and reducing proteinuria. Statins may be prescribed to manage dyslipidemia, further minimizing cardiovascular risks associated with chronic kidney disease (CKD) (Morrison et al., 2023).
Non-Pharmacological Strategies
Lifestyle modifications are equally vital in managing stage 3a kidney disease. Dietary changes are critical, often involving a reduction in protein intake to decrease the kidneys’ workload. Patients are encouraged to follow a renal diet, which typically emphasizes fruits, vegetables, and whole grains while limiting sodium, potassium, and phosphorus (Morrison et al., 2023).
Regular Monitoring
Regular follow-up appointments are essential for monitoring kidney function and adjusting treatment plans accordingly. Blood tests to assess eGFR and urine tests to measure protein levels help guide management strategies. Patients should also be educated about recognizing early signs of complications, such as worsening edema or changes in urine output, prompting timely medical intervention (Morrison et al., 2023).
Dietary Guidelines for Patients with Stage 3a Kidney Disease
Dietary management is a cornerstone of treatment for stage 3a kidney disease. Adhering to specific dietary guidelines can significantly impact the progression of kidney disease and overall health.
Protein Intake
Restricting protein intake is often recommended to minimize the kidneys’ workload. The general guideline suggests moderating protein consumption to about 0.6 to 0.8 grams per kilogram of body weight per day, depending on the individual’s nutritional status and kidney function (Morrison et al., 2023). High-quality proteins, such as those from lean meats, fish, eggs, and dairy, should be prioritized.
Sodium Restriction
Limiting sodium intake is crucial to manage hypertension and fluid retention. A sodium intake of less than 2,300 mg per day is generally advised, although some patients may benefit from even lower levels (Morrison et al., 2023). Reading food labels and avoiding processed foods can help maintain this restriction.
Potassium and Phosphorus Management
Patients may also need to monitor their potassium and phosphorus intake. Foods rich in potassium, such as bananas, oranges, and potatoes, may need to be limited, especially in cases of hyperkalemia. Similarly, phosphorus-rich foods, including dairy products, nuts, and certain meats, should be consumed in moderation to avoid complications like bone disease (Morrison et al., 2023).
Fluid Intake
Fluid intake may need adjustment based on the patient’s individual circumstances, particularly if they experience significant swelling or fluid retention. Monitoring daily fluid intake can help maintain balance and prevent complications associated with excessive fluid accumulation (Morrison et al., 2023).
Lifestyle Changes to Improve Outcomes in Stage 3a Kidney Disease
In addition to dietary modifications, several lifestyle changes can promote better health outcomes for individuals with stage 3a kidney disease.
Physical Activity
Engaging in regular physical activity is beneficial, as it helps control weight, lowers blood pressure, and improves overall cardiovascular health. Patients should aim for at least 150 minutes of moderate-intensity exercise per week, as tolerated (Morrison et al., 2023). Activities may include walking, swimming, cycling, or any enjoyable form of exercise.
Smoking Cessation
Smoking has detrimental effects on kidney health and overall cardiovascular functioning. Quitting smoking can significantly improve health outcomes for patients with CKD. Support programs and pharmacotherapy may be helpful for those struggling to quit (Morrison et al., 2023).
Stress Management
Managing stress through techniques such as mindfulness, meditation, or yoga can positively influence overall well-being and support kidney health. Chronic stress can exacerbate hypertension and other health issues, making stress reduction practices essential for patients with kidney disease (Morrison et al., 2023).
Regular Health Screenings
Routine health check-ups are essential to monitor kidney function and manage other health conditions. Regular screenings for blood pressure, blood sugar levels, and cholesterol are vital for preventing complications associated with kidney disease (Morrison et al., 2023).
Importance of Regular Monitoring and Follow-Up in Stage 3a Kidney Disease
Regular monitoring and follow-up are critical components in the management of stage 3a kidney disease. These practices enable healthcare providers to track disease progression, adjust treatment plans, and address complications promptly.
Blood Tests
Patients should undergo routine blood tests to measure serum creatinine and estimate eGFR. These tests help assess kidney function and determine if any adjustments in medication or dietary changes are necessary (Morrison et al., 2023).
Urine Tests
Urine tests are essential for monitoring proteinuria, which is a key indicator of kidney damage. The presence of protein in urine can signal the progression of kidney disease and the need for more aggressive management strategies (Morrison et al., 2023).
Patient Education
Educating patients about the importance of regular monitoring, recognizing signs of complications, and adhering to prescribed treatment plans is vital. Patients should be encouraged to communicate any changes in their health status to their healthcare providers (Morrison et al., 2023).
Coordination of Care
Multidisciplinary care involving nephrologists, dietitians, and primary care providers is crucial for comprehensive management. Coordinated care ensures that all aspects of the patient’s health are addressed, optimizing outcomes and reducing the risk of complications (Morrison et al., 2023).
FAQ
What is stage 3a kidney disease?
Stage 3a kidney disease indicates a moderate decline in kidney function, typically with an eGFR of 45-59 mL/min. It often involves symptoms like fatigue, swelling, and changes in urination.
How can I manage stage 3a kidney disease effectively?
Effective management includes medications to control underlying conditions, dietary modifications, lifestyle changes, and regular monitoring of kidney function.
What dietary changes should I make?
Patients should consider reducing protein, sodium, potassium, and phosphorus intake, alongside monitoring fluid consumption based on individual needs.
Why is regular follow-up important for kidney disease?
Regular follow-up allows for close monitoring of kidney function, timely adjustments to treatment, and early detection of potential complications.
Can exercise help with stage 3a kidney disease?
Yes, regular physical activity can help manage weight, lower blood pressure, and improve overall cardiovascular health, which is beneficial for kidney disease management.
References
-
Morrison, M. A., Artru, F., Trovato, F. M., Triantafyllou, E., & McPhail, M. J. (2023). Potential therapies for acute‐on‐chronic liver failure. Liver International, 45, e15545
-
Parvin, R., Ullah, M. H., Pervin, H., & Siddiki, A. M. A. M. Z. (2025). Designing of a multiepitope-based vaccine against echinococcosis utilizing the potent Ag5 antigen: Immunoinformatics and simulation approaches. PLoS One, 15(2), e0310510. https://doi.org/10.1371/journal.pone.0310510
-
Haque, A., & Echinococcosis. (2025). Designing of a multiepitope-based vaccine against echinococcosis utilizing the potent Ag5 antigen: Immunoinformatics and simulation approaches. PLoS ONE