Table of Contents
Symptoms and Causes of Yeast and Trichomoniasis Discharge
Yeast Infections
Yeast infections, primarily caused by Candida albicans, manifest in various symptoms. Common symptoms include:
- Itching and irritation: Often persistent and can lead to discomfort.
- Vaginal discharge: Typically thick, white, and clumpy resembling cottage cheese.
- Redness and swelling: The vulva may appear inflamed.
- Pain during intercourse: Discomfort may arise due to inflammation.
The prevalence of yeast infections is notably high, with studies indicating that up to 75% of women will experience a yeast infection at least once in their lifetime (Fernandes et al., 2023). Contributing factors include:
- Antibiotic use: Disruption of normal vaginal flora can lead to overgrowth of yeast.
- Hormonal changes: Fluctuations during pregnancy, menstruation, or due to contraceptive use can increase susceptibility.
- Immunocompromised states: Conditions like diabetes or HIV can predispose individuals to infections.
Trichomoniasis
Trichomoniasis is a sexually transmitted infection caused by the protozoan Trichomonas vaginalis. Symptoms may include:
- Abnormal discharge: Often yellowish or greenish, with a foul odor.
- Itching and irritation: Similar to yeast infections but may be more pronounced.
- Painful urination and intercourse: This can lead to further discomfort.
Trichomoniasis affects millions of women globally, and recent research indicates that co-infection with other STIs is common, complicating treatment (Van Der Pol et al., 2024).
The causes of trichomoniasis are mainly linked to:
- Sexual contact: Transmission occurs via sexual activity, highlighting the need for safe sex practices.
- Multiple sexual partners: Increased risk correlates with a higher number of partners.
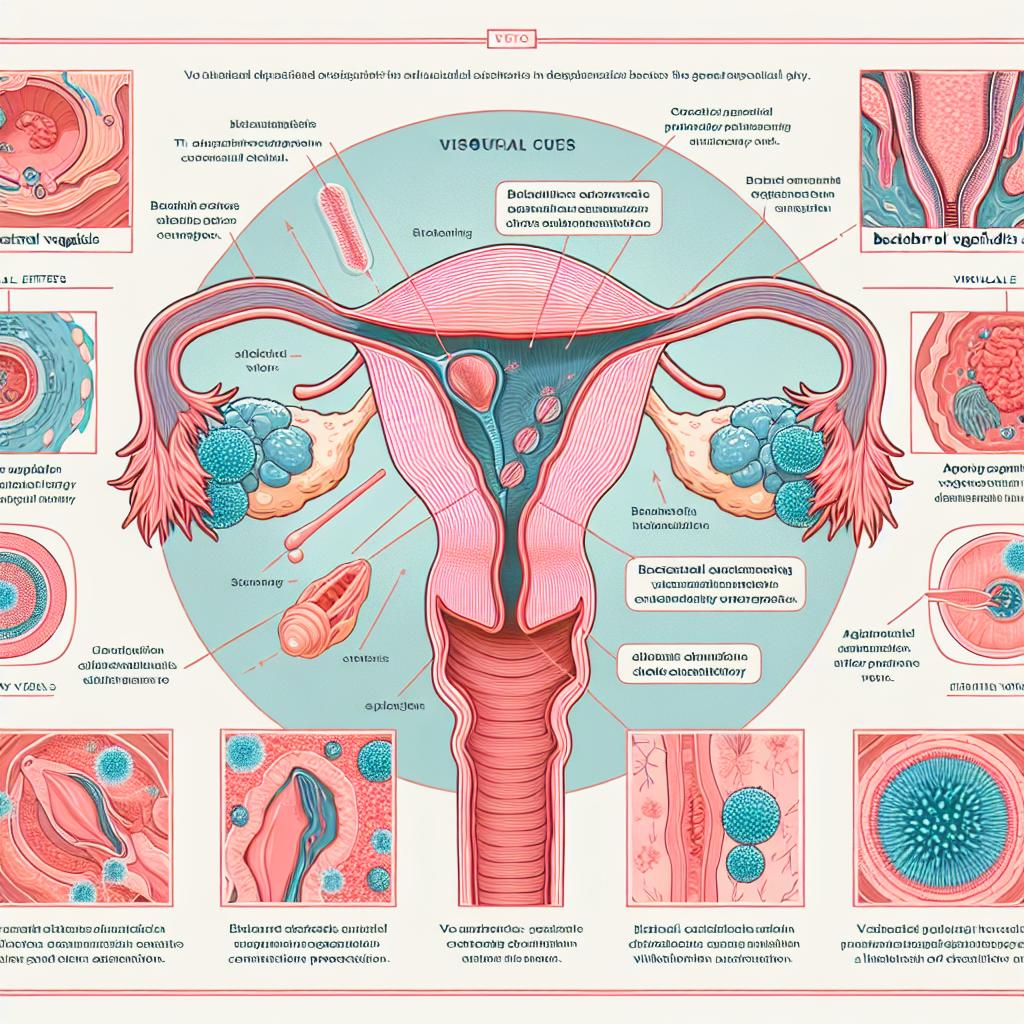
Diagnostic Methods for Identifying Yeast and Trichomoniasis
Accurate diagnosis is essential for effective treatment of yeast infections and trichomoniasis. Common diagnostic methods include:
Clinical Examination
- Visual assessment: A healthcare provider may perform a physical examination to assess symptoms.
- Vaginal pH testing: Normal vaginal pH is between 3.8 and 4.5; elevated pH levels may indicate infection.
Laboratory Tests
- Wet mount microscopy: This allows for the identification of yeast or trichomonads in discharge samples (Obiero et al., 2018).
- Culture tests: Cultures can help identify the specific causative agent, especially in recurrent infections.
- PCR testing: Molecular methods provide rapid and accurate identification of pathogens, including Candida and Trichomonas vaginalis (Fernandes et al., 2023).
New Diagnostic Technologies
Recent advances in molecular diagnostic tools, such as multiplex PCR assays, can detect multiple pathogens from a single sample, improving diagnostic accuracy and patient outcomes (Van Der Pol et al., 2024).
Treatment Options for Yeast Infections and Trichomoniasis
Once diagnosed, treatment options can vary based on the type and severity of the infection.
Treatment for Yeast Infections
-
Antifungal medications: First-line treatments typically include azole antifungals such as fluconazole or topical agents like clotrimazole (Yefet et al., 2024).
-
Probiotics: Some studies suggest that probiotics may help restore normal flora post-antibiotic use, although results vary (Nachum et al., 2025).
Treatment for Trichomoniasis
-
Antimicrobial therapy: Metronidazole or tinidazole is the standard treatment for trichomoniasis, typically administered in a single high dose or over a period of days (Schumann et al., 2024).
-
Partner treatment: To prevent re-infection, partners should also receive treatment simultaneously (Obiero et al., 2018).
Combination Therapy
Due to the frequent occurrence of co-infections, combination therapies may be necessary, particularly for patients diagnosed with both bacterial vaginosis and yeast infections (Fernandes et al., 2023).
Preventative Measures for Managing Vaginal Discharge Issues
Preventing infections involves both lifestyle changes and proper hygiene practices. Important preventative measures include:
- Maintaining good personal hygiene: Regular washing with mild, unscented soaps helps maintain vaginal health.
- Wearing breathable underwear: Cotton fabric allows for better ventilation compared to synthetic materials, reducing moisture buildup.
- Safe sex practices: Using condoms can lower the risk of STIs, including trichomoniasis (Yefet et al., 2024).
- Limiting antibiotic use: Avoid unnecessary antibiotics, which can disrupt the natural vaginal flora.
Regular Check-ups
Routine gynecological exams can help detect infections early and manage any symptoms before they escalate.
When to Seek Medical Attention for Yeast and Trichomoniasis Discharge
It is essential to seek medical advice when experiencing:
- Persistent symptoms: If itching, burning, or abnormal discharge continues despite treatment.
- Severe pain: Experiencing sharp or severe pain during urination or intercourse.
- Recurrent infections: More than four episodes of yeast infections in a year warrant further investigation.
Conclusion
Effective management of vaginal discharge caused by yeast infections and trichomoniasis hinges on understanding the symptoms, accurate diagnosis, and appropriate treatment options. Preventative measures and awareness of when to seek medical attention can significantly improve women’s reproductive health.
References
- van der Pol, B., Aycock, C., Dixon, P., Kodsi, S., Paradis, S., Torres-Chavolla, E., & Parvu, V. (2024). Comprehensive assessment of vaginal infections using a single swab. Sexually Transmitted Infections. https://doi.org/10.1136/sextrans-2024-056263
- nachum, Z., Suleiman, A., Colodner, R., Battino, S., Wattad, M., Kuzmin, O., & Yefet, E. (2025). Oral probiotics to prevent recurrent vulvovaginal infections during pregnancy—multicenter double-blind, randomized, placebo-controlled trial. Nutrients, 17(3), 460. https://doi.org/10.3390/nu17030460
- Fernandes, V. L., Martinho, S. M., & Pires, A. R. (2023). Utility of Cand PCR in the Diagnosis of Vulvovaginal Candidiasis in Pregnant Women. Journal of Fungi, 11(1), 5. https://doi.org/10.3390/jof11010005
- Yefet, E., & Nachum, Z. (2024). Knowledge of Vulvovaginal Candidiasis Characteristics, Signs, Symptoms, and Appropriate Treatment Among Portuguese Pharmacy Professionals. Healthcare, 13(4). https://doi.org/10.3390/healthcare13040402
- Schumann, J. A., Plasner, S., & Gorman, S. (2024). Vaginal candidiasis. StatPearls.
- Obiero, J., Rulisa, S., Ogongo, P., & Wiysonge, C. S. (2018). Nifuratel-Nystatin combination for the treatment of mixed infections of bacterial vaginosis, vulvovaginal candidiasis, and trichomonal vaginitis. Cochrane Database of Systematic Reviews
FAQ
What are the main symptoms of a yeast infection?
Symptoms include intense itching, thick white discharge resembling cottage cheese, redness, and swelling.
How is trichomoniasis diagnosed?
It is diagnosed through physical examination, wet mount microscopy, and culture tests.
What treatments are available for yeast infections?
Treatment typically involves antifungal medications such as fluconazole or topical clotrimazole.
Can probiotics help with recurrent yeast infections?
Some studies suggest that probiotics may aid in restoring normal vaginal flora, but results can vary.
When should I see a doctor for vaginal discharge?
If you experience persistent symptoms, severe pain, or recurrent infections, consult a healthcare professional.