Table of Contents
Causes of UTI After Period: Understanding the Triggers
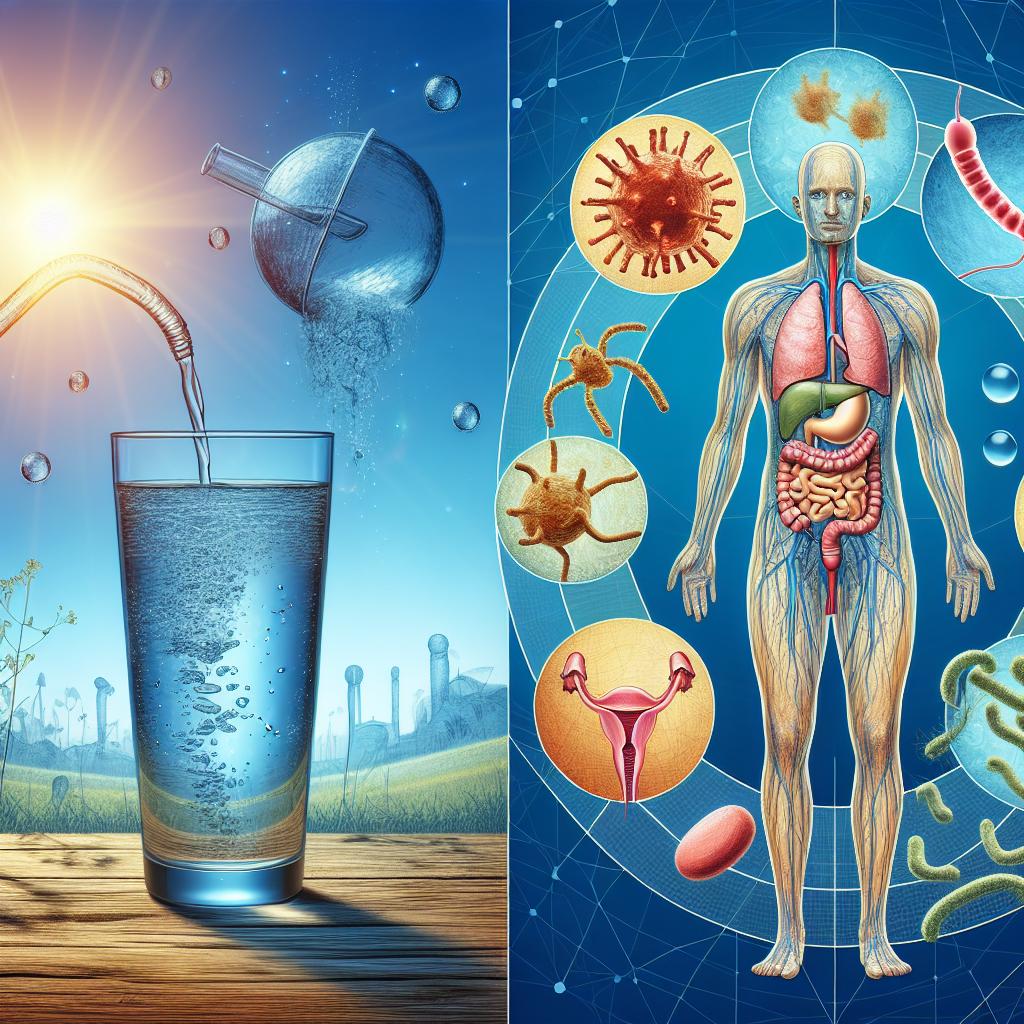
The onset of a urinary tract infection following menstruation can be attributed to several interrelated factors. Firstly, hormonal fluctuations during the menstrual cycle can affect the bladder and urethra, potentially increasing susceptibility to infections (Nair et al., 2023). After menstruation, the vaginal flora may also undergo changes that can lead to overgrowth of pathogenic bacteria, contributing to a higher risk of UTIs.
Additionally, it is essential to consider hygiene practices during menstruation. The use of sanitary products, if not changed regularly, can create a moist environment conducive to bacterial growth. Furthermore, the introduction of bacteria into the urethra during the use of tampons or menstrual cups can also be a contributing factor (Carpenter et al., 2023).
Table 1: Common Triggers for UTI After Menstruation
| Trigger | Description |
|---|---|
| Hormonal Changes | Fluctuations in estrogen and progesterone levels |
| Vaginal Flora Alterations | Changes in microbial balance post-menstruation |
| Sanitary Product Hygiene | Infrequent changing of tampons or pads |
| Urethral Introduction of Bacteria | Use of menstrual products leading to bacterial entry |
Symptoms of UTI After Menstruation: What to Watch For
Recognizing the symptoms of a UTI is vital for early intervention. Common symptoms may include:
- Frequent Urination: An increased urge to urinate, often with little output.
- Burning Sensation: A painful or burning sensation during urination.
- Cloudy or Strong-Smelling Urine: Changes in the urine’s appearance or odor.
- Pelvic Discomfort: Pain or pressure in the lower abdomen.
- Fever and Chills: In more severe cases, systemic symptoms like fever may occur.
It’s important to note that some women may experience UTI symptoms even if they do not have a confirmed infection, a condition known as interstitial cystitis (IC) (Heimann et al., 2024). Differentiating between a UTI and IC is crucial for appropriate treatment.
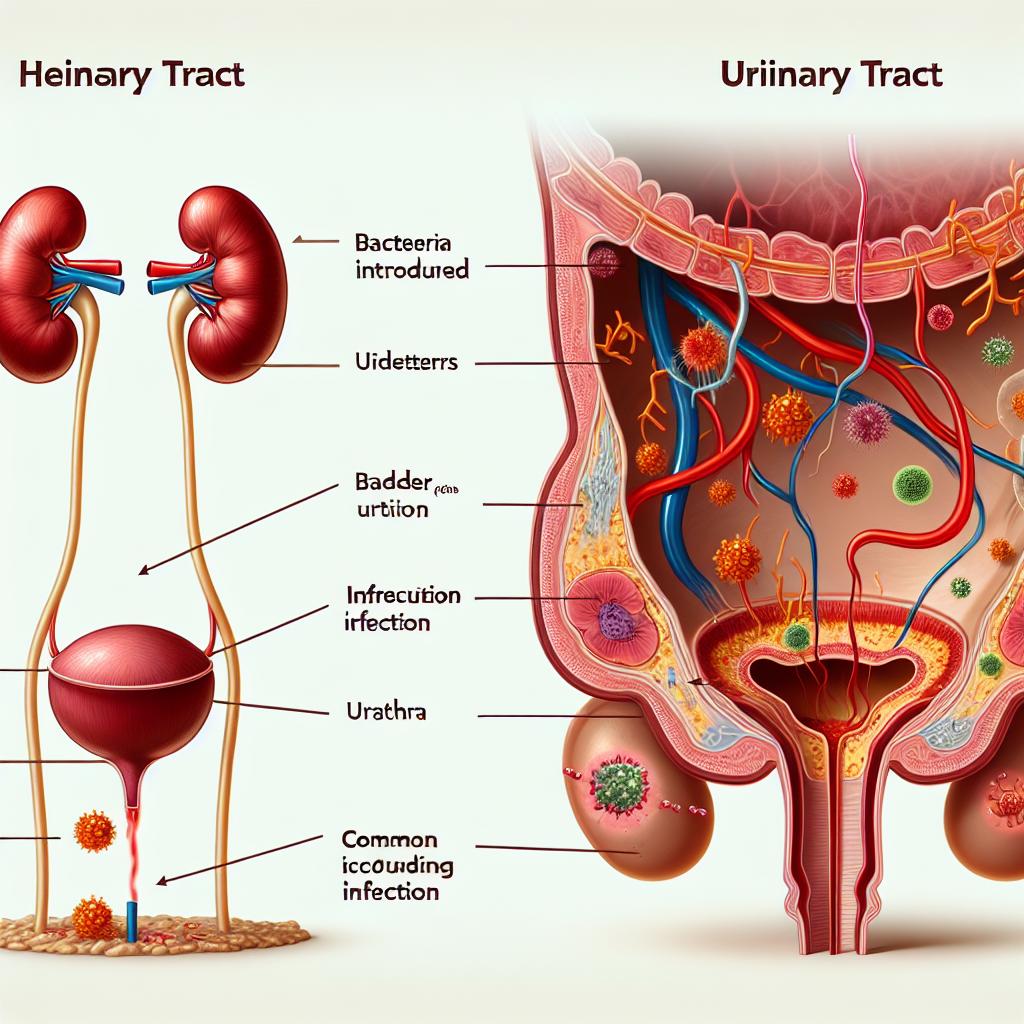
Diagnosing UTI After Period: Tests and Procedures Explained
Diagnosis of a UTI typically involves a combination of patient history, symptom assessment, and laboratory tests. The following steps are usually taken:
- Urinalysis: A sample of urine is tested for the presence of white blood cells, red blood cells, and bacteria.
- Urine Culture: This test identifies the specific bacteria causing the infection and determines antibiotic susceptibility.
- Imaging Studies: In recurrent cases, imaging such as an ultrasound or CT scan may be used to identify any structural abnormalities in the urinary tract.
Table 2: Diagnostic Tests for UTI
| Test | Purpose |
|---|---|
| Urinalysis | To detect the presence of bacteria and inflammatory cells |
| Urine Culture | To identify the specific pathogen and its antibiotic resistance |
| Imaging Studies | To evaluate for anatomical abnormalities contributing to recurrent Utis |
Treatment Options for UTI After Period: Antibiotics and Beyond
Treatment for UTIs typically involves the use of antibiotics, which are selected based on the sensitivity profile of the identified pathogen. Commonly prescribed antibiotics include:
- Nitrofurantoin: Often used for uncomplicated UTIs.
- Trimethoprim/Sulfamethoxazole: Commonly prescribed but resistance is increasing.
- Fosfomycin: An alternative for those with allergies to other antibiotics.
In addition to antibiotics, symptomatic relief can be achieved through analgesics and increased fluid intake to help flush out the bacteria (Heimann et al., 2024). It’s essential to complete the entire course of antibiotics as prescribed to prevent recurrence and resistance.
Table 3: Common Antibiotics Used in UTI Treatment
| Antibiotic | Indication | Resistance Concerns |
|---|---|---|
| Nitrofurantoin | Uncomplicated UTIs | Some resistance noted |
| Trimethoprim/Sulfamethoxazole | First-line for uncomplicated UTIs | Increasing resistance |
| Fosfomycin | Alternative treatment | Generally low resistance |
Preventive Strategies for UTI After Period: Tips for Women
Preventing UTIs after menstruation involves both behavioral and lifestyle modifications. Here are some effective strategies:
- Hygiene Practices: Maintain good personal hygiene by wiping from front to back and changing sanitary products frequently.
- Hydration: Drink plenty of water to help dilute urine and promote frequent urination.
- Cranberry Products: Some studies suggest that cranberry juice or supplements may help prevent UTIs, although results are mixed (Carpenter et al., 2023).
- Urination Post-Intercourse: Urinating after sexual activity can help flush out bacteria introduced into the urethra.
- Avoid Irritants: Stay away from irritating feminine products that can alter the vaginal flora.
Table 4: Preventive Strategies for UTI
| Strategy | Description |
|---|---|
| Hygiene Practices | Regular bathing and proper wiping techniques |
| Hydration | Increased fluid intake to promote urination |
| Cranberry Products | May help prevent bacterial adherence |
| Post-Intercourse Urination | Flushing out introduced bacteria |
| Avoiding Irritants | Steering clear of products that may irritate the urinary tract |
FAQ Section
How can I tell if I have a UTI after my period?
Common symptoms of a UTI include frequent urination, burning during urination, cloudy urine, and pelvic discomfort. If you experience these symptoms, consult with a healthcare provider for diagnosis and treatment.
Can I take over-the-counter medications for UTI relief?
Yes, there are over-the-counter medications available that can help relieve the pain associated with UTIs, such as phenazopyridine. However, they do not treat the infection itself.
Are there any long-term effects of untreated UTIs?
Untreated Utis can lead to more severe complications, including kidney infections (pyelonephritis) and recurrent UTIs. It is essential to seek treatment if symptoms arise.
What should I do if I keep getting UTIs after my period?
If you experience recurrent UTIs, it’s important to consult with a healthcare provider. They may recommend lifestyle changes, prophylactic antibiotics, or further testing to identify underlying issues.
Can diet affect my risk of getting a UTI?
Yes, certain dietary choices can influence UTI risk. Foods high in sugar may promote bacterial growth, while hydration and foods like cranberries may help prevent UTIs.
References
-
Carpenter, A., Hinkle, J., Snow, N., Kalluri, N., Perkins, D., & Nakamura, J. (2023). Emergency Department Antibiotic Prescribing for Pediatric Urinary Tract Infections, 2011–2020. PubMed. https://pubmed.ncbi.nlm.nih.gov/11892075/
-
Heimann, D., Kohnhäuser, D., Kohnhäuser, A. J., & Brönstrup, M. (2024). Antibacterials with Novel Chemical Scaffolds in Clinical Development. Drugs. https://doi.org/10.1007/s40265-024-02137-x
-
Nair, S., & Thakur, S. (2023). Updates on HIV Pre-exposure Prophylaxis in Latin America: Available Drugs and Implementation Status. PubMed. https://pubmed.ncbi.nlm.nih.gov/11892447/