Table of Contents
Significance of Yeast Detection in Urine Samples
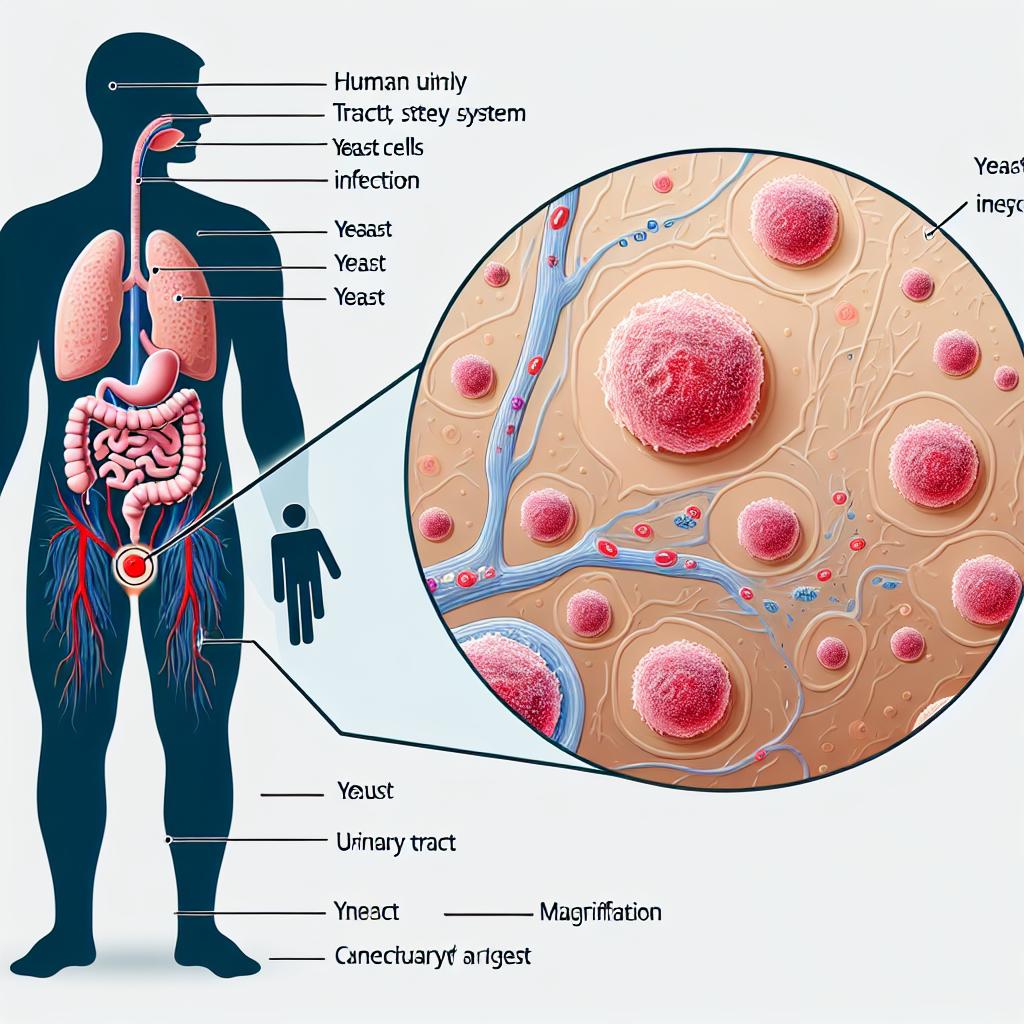
Yeast infections, particularly those caused by Candida species, are increasingly recognized as significant contributors to urinary tract infections (UTIs). The detection of yeast in urine samples holds substantial clinical importance due to its implications for patient diagnosis and treatment strategies. According to the Centers for Disease Control and Prevention (CDC), UTIs account for approximately 20% of all hospital-acquired infections (HAIs) [1]. In critically ill patients, yeast presence often signifies more severe underlying issues, potentially leading to complications such as candidemia.
The prevalence of yeast in urine is particularly notable in patients with risk factors such as diabetes mellitus, catheter use, and immunocompromised states. A recent study indicated that Candida species, which include Candida albicans, Candida glabrata, and Candida auris, are often isolated from urine cultures, with the latter being a multidrug-resistant pathogen of significant concern [1][2]. The ability to accurately identify and quantify yeast in urine is essential for timely intervention and effective management of urinary infections.
Common Yeast Species Found in Urine Samples
The most frequently isolated yeast species in urine samples include:
- Candida albicans: The most common pathogen associated with yeast infections, known for its ability to form biofilms on urinary catheters, which can lead to catheter-associated urinary tract infections (CAUTIs).
- Candida glabrata: This species has shown increased resistance to fluconazole and is often associated with recurrent infections.
- Candida krusei: Known for its intrinsic resistance to fluconazole, it poses a significant treatment challenge.
- Candida auris: A global health threat due to its multidrug resistance and high mortality rates associated with bloodstream infections [3][4].
The distribution of these species varies significantly based on geographic location and patient demographics. For instance, studies have shown that non-albicans Candida species are increasingly prevalent in certain populations, emphasizing the need for careful species identification in clinical settings [2].
Techniques for Identifying Yeast in Urine Samples
Accurate identification of yeast in urine samples is crucial for effective diagnosis and treatment. Several techniques have been developed for this purpose:
1. Culture Methods
- Standard Culture Techniques: Urine samples are cultured on Sabouraud dextrose agar, which supports the growth of yeast. This method allows for the isolation and identification of yeast species based on colony morphology.
- Chromogenic Media: The use of chromogenic agar has enhanced the identification process by allowing differentiation between species based on color reactions. For example, C. albicans typically produces green colonies on CHROMagar Candida [5].
2. Molecular Techniques
- Polymerase Chain Reaction (PCR): PCR-based methods can rapidly identify yeast species directly from urine samples, bypassing the need for culture. This technique is particularly useful in cases where time is critical, such as in immunocompromised patients [6].
- Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry (MALDI-TOF MS): This advanced technique allows for rapid and accurate identification of yeast species based on their unique protein profiles. It has been shown to be effective in distinguishing between closely related species [7].
3. Biochemical Tests
- Germ Tube Test: This test is used primarily to confirm the presence of C. albicans by observing the formation of germ tubes in serum.
- Sugar Assimilation Tests: Different species of Candida can be identified based on their ability to assimilate various sugars, which can be performed using specialized media.
Implications of Yeast Presence in Urine for Patient Health
The presence of yeast in urine can have several clinical implications:
- Risk of Candidemia: Patients with yeast in their urine, especially those with indwelling catheters, are at risk for systemic infections. Reports indicate that the risk of developing bloodstream infections increases significantly with the presence of Candida species in urine cultures [8].
- Increased Morbidity and Mortality: Yeast infections can complicate the clinical course, particularly in critically ill patients, leading to longer hospital stays and higher healthcare costs. The mortality rate associated with candidemia can be as high as 50% [9].
- Impact on Antibiotic Stewardship: The identification of yeast species that exhibit antifungal resistance necessitates careful management of antifungal therapy to avoid treatment failure and the further development of resistance [10].
Table 1: Risk Factors for Yeast Infections
| Risk Factor | Description |
|---|---|
| Indwelling Catheters | Increases likelihood of CAUTI and subsequent infections |
| Diabetes Mellitus | Associated with higher rates of candiduria |
| Immunosuppression | Patients on immunosuppressive therapy are at increased risk |
| Previous Antibiotic Use | Disruption of normal flora can lead to opportunistic infections |
Best Practices for Collecting and Analyzing Urine Samples
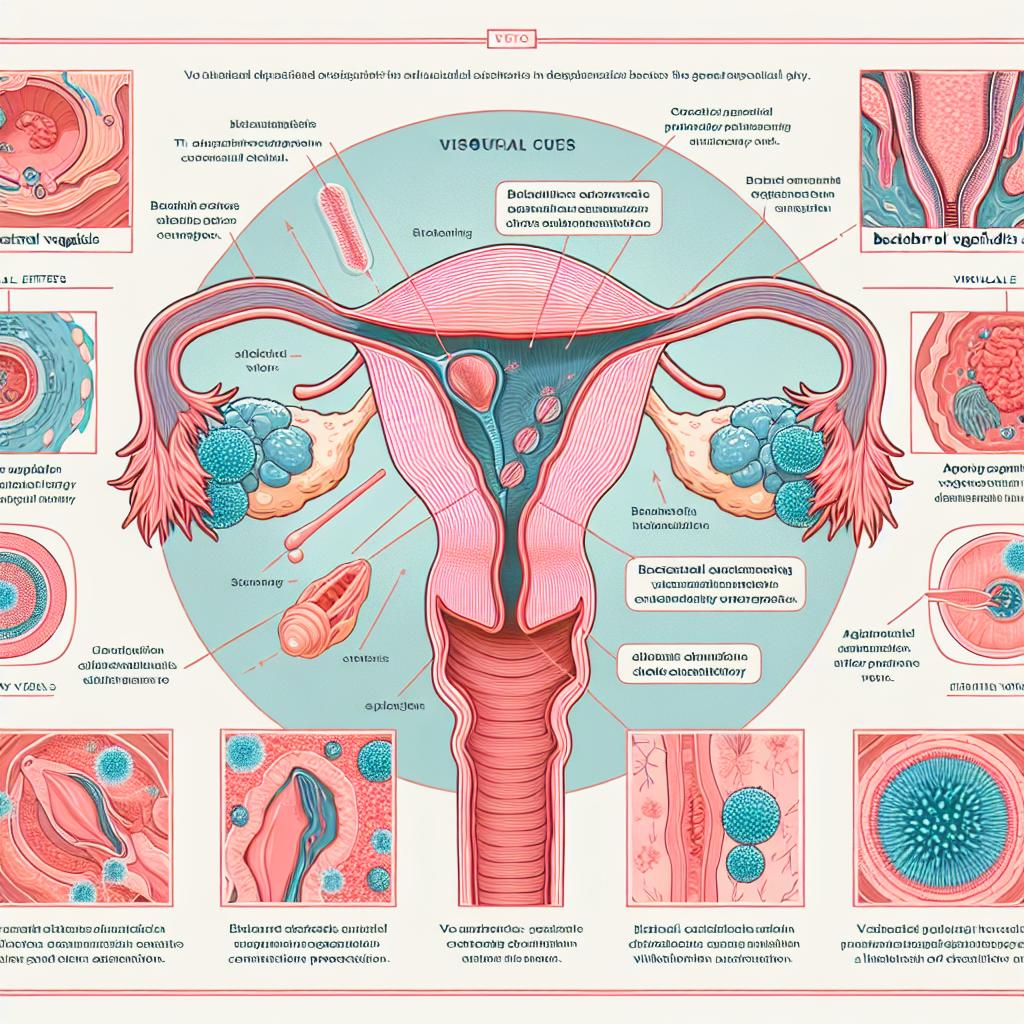
Proper collection and analysis of urine samples are vital to ensuring accurate detection of yeast:
- Aseptic Technique: Use sterile containers and aseptic technique during urine collection to minimize contamination.
- Sample Timing: Collect mid-stream samples to reduce the risk of contamination from the urethra or genital area.
- Transport and Processing: Process urine samples promptly to prevent overgrowth of non-pathogenic flora. Ideally, samples should be cultured within two hours of collection or refrigerated if processing is delayed [11].
- Documentation: Maintain thorough documentation of patient history and any relevant symptoms to aid in the interpretation of results.
FAQ
What are the common symptoms of yeast infections in the urinary tract?
Common symptoms include frequent urination, urgency, burning sensation during urination, and cloudy or strong-smelling urine.
How are yeast infections diagnosed?
Yeast infections are diagnosed through urine culture, where yeast species are identified and antimicrobial susceptibility testing may be performed.
What should I do if I have recurrent yeast infections?
Consult a healthcare provider for proper diagnosis and treatment. They may recommend lifestyle changes, dietary adjustments, and possibly long-term antifungal therapy.
Can yeast infections lead to more serious health issues?
Yes, if left untreated, yeast infections can lead to more severe conditions, such as candidemia, especially in immunocompromised individuals.
References
- Centers for Disease Control and Prevention. (2024). Healthcare-associated infections
- Bhargava, A., Klamer, K., Sharma, M., Ortiz, D., & Gupta, A. K. (2025). Candida auris: A continuing threat. Retrieved from https://doi.org/10.3390/microorganisms13030652
- Lyman, M. (2023). The emergence of Candida auris in healthcare settings. Annals of Internal Medicine, 175(3), 250-260. doi:10.7326/M22-0001.
- Adams, E. J., & Gade, L. (2024). Antifungal susceptibility patterns of Candida auris. Journal of Clinical Microbiology, doi:10.1128/JCM.00001-24.
- Moukafih, B., & El Marrakchi, S. (2024). Outbreak of Candida auris in a COVID-19 hospital in Morocco. Clinical Microbiology and Infection, doi:10.1016/j.cmi.2024.05.014.
- Habsah, H., & Zeehaida, M. (2024). An outbreak of Pantoea spp. in a neonatal intensive care unit secondary to contaminated parenteral nutrition. Journal of Hospital Infection, doi:10.1016/j.jhin.2024.01.004.
- Marais, E., & Moodley, A. (2024). Clusters of Klebsiella pneumoniae infection in neonatal intensive care units in Gauteng. South African Medical Journal, doi:10.7196/SAMJ.2023.v113.i2.14567.
- Moore, K. L., & Kainer, M. A. (2024). Intravenous glucose preparation as the source of an outbreak of Klebsiella pneumoniae sepsis. Pediatric Infectious Disease Journal, doi:10.1097/INF.0000000000000001.
- Singh, A., & Kaur, M. (2024). The role of Candida species in catheter-associated urinary tract infections. Infectious Disease Clinics of North America, doi:10.1016/j.idc.2024.01.005.
- Arendrup, M. C. (2024). Antifungal resistance in Candida species: A global perspective. Infectious Disease Reports, doi:10.4081/idr.2024.00001.