Table of Contents
Factors Contributing to UTIs: The Role of Sexual Activity
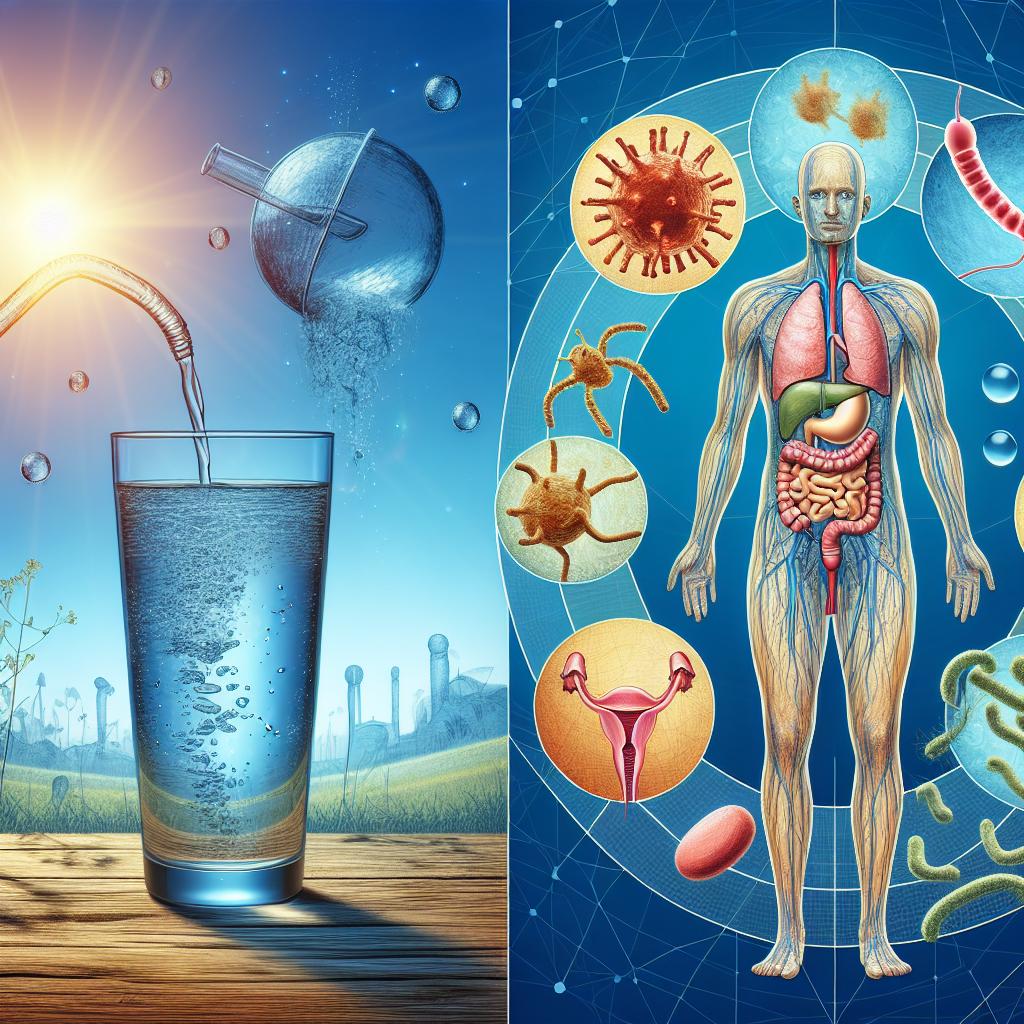
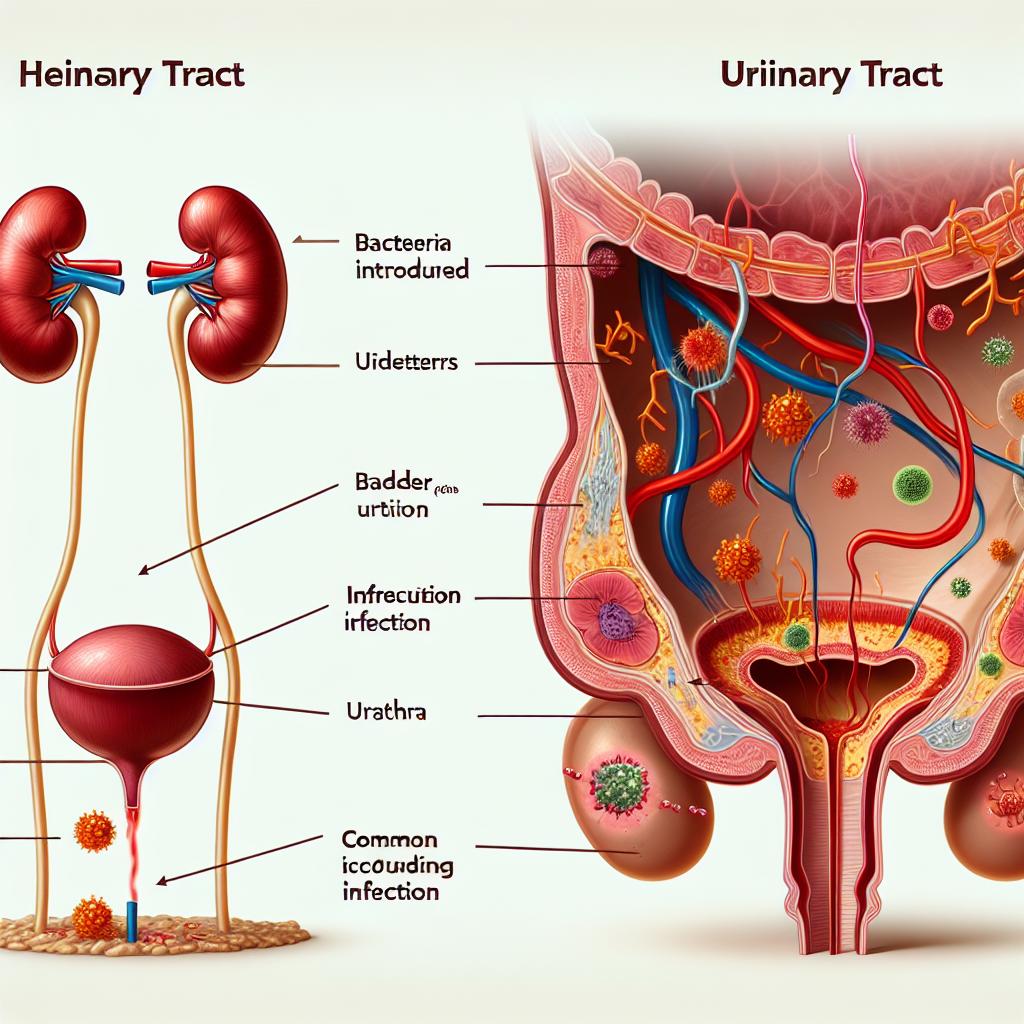
UTIs occur when bacteria enter the urinary tract, leading to inflammation and infection. Several factors can contribute to the development of UTIs, and sexual activity is frequently highlighted as a significant risk factor. The anatomy of the female urinary tract, including the proximity of the urethra to the vagina and anus, plays a crucial role.
During sexual intercourse, bacteria from the genital area can be pushed into the urethra. This can lead to an increased risk of infection, especially if there are pre-existing vulnerabilities such as a history of recurrent Utis, hormonal changes, or anatomical anomalies. Studies have shown that women who are sexually active are more likely to experience UTIs compared to those who do not engage in sexual activity. The introduction of bacteria during sexual activity can disrupt the natural flora of the urinary tract, leading to infection.
Additionally, factors such as the use of spermicides and diaphragms as contraceptive methods have been linked to a higher incidence of UTIs. Spermicides can alter the natural vaginal flora, making it easier for harmful bacteria to establish an infection. Understanding these risk factors is crucial for individuals who are sexually active, particularly women, as it can help in taking preventive measures to reduce the risk of UTIs.
How Sexual Intercourse Affects Women’s Urinary Tract Health
The impact of sexual intercourse on urinary tract health is multifaceted. Research indicates that sexual activity can lead to the introduction of bacteria into the urinary tract, increasing the likelihood of infection. The act of intercourse can also cause microtrauma to the vaginal lining, which may facilitate the entry of pathogens.
A study published in the Infection and Drug Resistance journal highlights that women who engage in frequent sexual activity are at an elevated risk of developing UTIs. The authors suggest that proper hygiene practices before and after sexual intercourse can significantly reduce this risk. Furthermore, the timing of urination relative to sexual activity can also play a role in urinary tract health. Urinating after intercourse helps flush out any bacteria that may have been introduced during sex, thereby reducing the risk of developing a UTI.
Additionally, hormonal changes associated with sexual activity and menstrual cycles may influence a woman’s susceptibility to UTIs. A fluctuation in hormone levels can affect the natural defense mechanisms of the urinary tract, making it more susceptible to infections.
Preventative Measures: Reducing the Risk of UTIs During Sex
Implementing effective preventative measures is essential for reducing the risk of UTIs associated with sexual activity. Here are several strategies that can be employed:
-
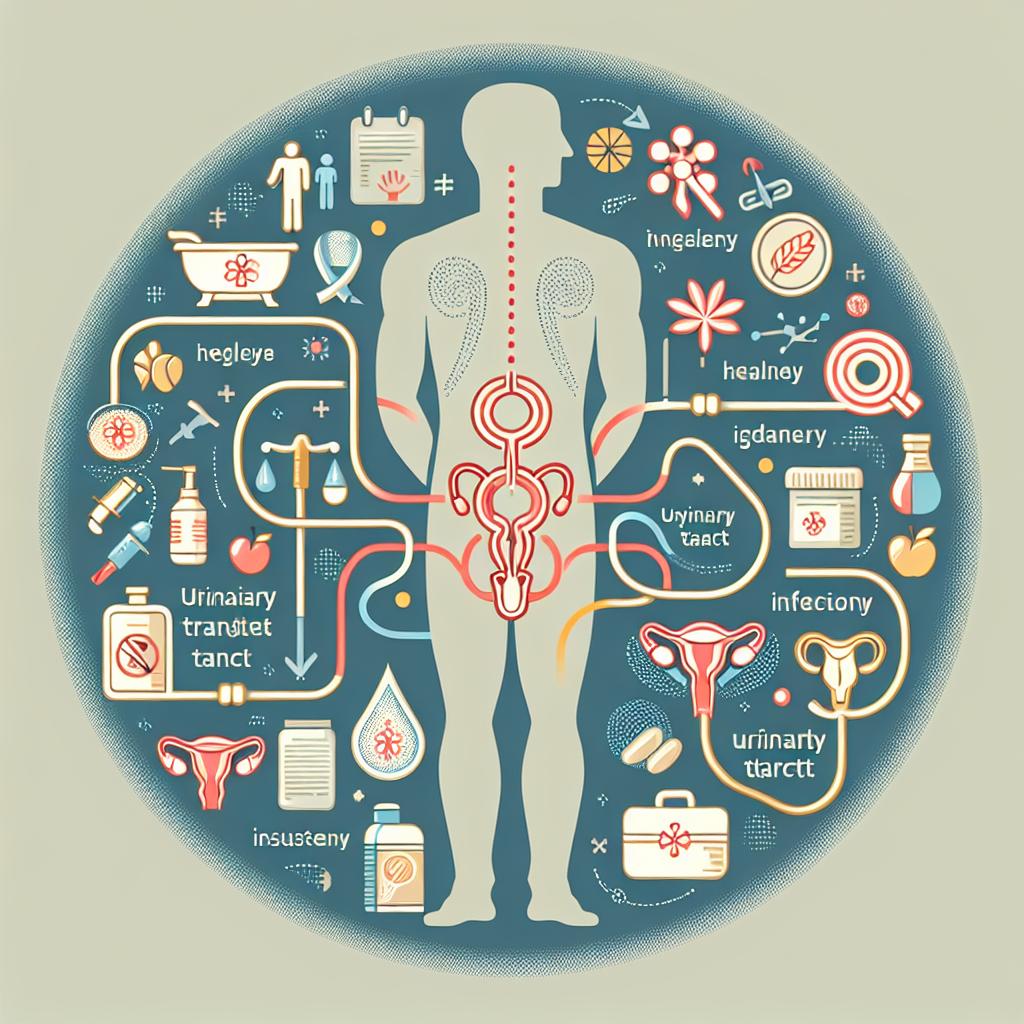
Hydration: Maintaining adequate hydration helps in diluting urine and flushing out bacteria. Drinking plenty of water before and after sexual activity can aid in this process.
-
Urination Post-Intercourse: Encouraging urination immediately after sexual intercourse can help clear the urethra of any bacteria that may have been introduced during sex.
-
Wiping Techniques: Women should be advised to wipe from front to back after using the toilet to minimize the risk of bacteria from the anal region entering the urethra.
-
Hygiene Practices: Practicing good genital hygiene before and after sexual activity is crucial. This includes showering and avoiding the use of irritating products in the genital area.
-
Contraceptive Choices: Women should consider using non-spermicidal contraceptive methods, as spermicides have been associated with an increased risk of UTIs.
-
Probiotics: Incorporating probiotics into the diet may help maintain a healthy balance of bacteria in the urinary tract and vagina, potentially reducing UTI risk.
-
Regular Medical Check-ups: Women who experience recurrent UTIs should consult healthcare professionals for personalized strategies and possible preventive antibiotic therapy.
By adopting these preventative measures, individuals can significantly lower their risk of developing UTIs associated with sexual activity.
Common Myths: Debunking Misconceptions About Sex and UTIs
Several myths surrounding UTIs and sexual activity persist, leading to confusion and misinformation. Here are some common misconceptions:
-
Myth: Only Women Get UTIs
Fact: While women are more prone to UTIs due to anatomical factors, men can also develop UTIs, particularly in cases of urinary obstruction or prostate issues. -
Myth: UTIs are Caused Only by Sexual Activity
Fact: While sexual activity is a contributing factor, UTIs can be caused by various factors including poor hygiene, certain medical conditions, and sexual practices. -
Myth: You Can’t Get a UTI After Taking Antibiotics
Fact: Antibiotics may treat existing UTIs but can also disrupt the natural flora of the urinary tract, making individuals more susceptible to new infections. -
Myth: Cranberry Juice Prevents UTIs
Fact: While cranberry juice may help in some cases, it is not a guaranteed preventive measure. More research is needed to establish its effectiveness. -
Myth: UTIs Always Cause Pain and Discomfort
Fact: Some individuals may have UTIs without experiencing noticeable symptoms, making it essential to get regular check-ups.
Debunking these myths is vital for individuals to understand their health better and take appropriate steps towards prevention and treatment.
When to Seek Medical Help: Recognizing UTI Symptoms After Sex
It’s crucial to recognize the symptoms of a UTI early to seek appropriate medical help. Common symptoms include:
- A strong, persistent urge to urinate
- A burning sensation during urination
- Frequent urination, often in small amounts
- Cloudy or strong-smelling urine
- Pelvic pain or pressure
If these symptoms occur following sexual activity, individuals should consult a healthcare professional promptly. Early diagnosis and treatment can prevent complications and further infections.
Table 1: Common Symptoms of UTIs
| Symptom | Description |
|---|---|
| Urgent Need to Urinate | Persistent urge to urinate frequently |
| Burning Sensation | Pain or discomfort during urination |
| Frequent Urination | Increased frequency of urination, often in small amounts |
| Cloudy Urine | Urine that appears murky or discolored |
| Strong Odor | Unpleasant or strong-smelling urine |
| Pelvic Pain | Discomfort or pain in the pelvic region |
Conclusion
Understanding the relationship between sexual activity and UTIs is essential for prevention and management. By recognizing the risks, implementing preventative measures, and debunking common myths, individuals can take proactive steps towards maintaining urinary tract health. Awareness of symptoms and prompt medical attention can further aid in effectively managing UTIs.
FAQ
Can men get UTIs?
A1: Yes, men can also develop UTIs, although they are less common than in women.
Is it safe to have sex if I have a UTI?
A2: It is generally advised to avoid sexual activity during a UTI to prevent further irritation and the potential spread of infection.
How often should I urinate to prevent UTIs?
A3: It is recommended to urinate every 2-4 hours and especially after sexual intercourse to help flush out bacteri
Can I use antibiotics to prevent UTIs?
A4: Some healthcare providers may prescribe antibiotics as a preventive measure for recurrent UTIs, but this should be discussed with a doctor.
Are there any home remedies for UTIs?
A5: Drinking plenty of water, urinating frequently, and consuming cranberry products may help, but they should not replace medical treatment.
References
-
Kim, T., Son, E., Wook, S. M., Jeon, D., Yeo, H. J., Lee, S. E. (2025). Predicting Healthcare-Associated Infection in Patients with Pneumonia via QuantiFERON®-Monitoring. Infect Drug Resist. https://doi.org/10.2147/IDR.S499765
-
Summary of guidelines from the Polish Urological Association, Polish Society of Gynaecologists and Obstetricians, and Polish Society of Family Medicine on the diagnosis, therapy, and management of community-acquired lower urinary tract infections. (2024). https://doi.org/10.5173/ceju.2024.01.Guid
-
Zhou, X., Liao, J., Lei, Z., Yao, H., Zhao, L., Yang, C. (2025). Nickel-based nanomaterials: a comprehensive analysis of risk assessment, toxicity mechanisms, and future strategies for health risk prevention. J Nanobiotechnol. https://doi.org/10.1186/s12951-025-03248-7
-
Ahamed, M., Alhadlaq, H. A., Akhtar, M. J., Khan, M. I., Al-Khedher, H., Alrokayan, S. A. (2023). Aetiology, antimicrobial susceptibility patterns and factors associated with bacteriuria among HIV-infected women attending Prevention of Mother-to-Child Transmission (PMTCT) clinic at Bukoba Municipality, Tanzania. PLoS One. https://doi.org/10.1371/journal.pone.0311474
-
Efficacy of 0.2% povidone‐iodine and 0.1% polyhexamethylene biguanide as preoperative antiseptics in equine ophthalmic procedures. (2021). https://pubmed.ncbi.nlm.nih.gov/11911974/
-
Antibiotic Use at the End of Life: Current Practice and Ways to Optimize. (2021). https://pubmed.ncbi.nlm.nih.gov/11915761/