Table of Contents
The Connection Between Antibiotics and Increased Urination
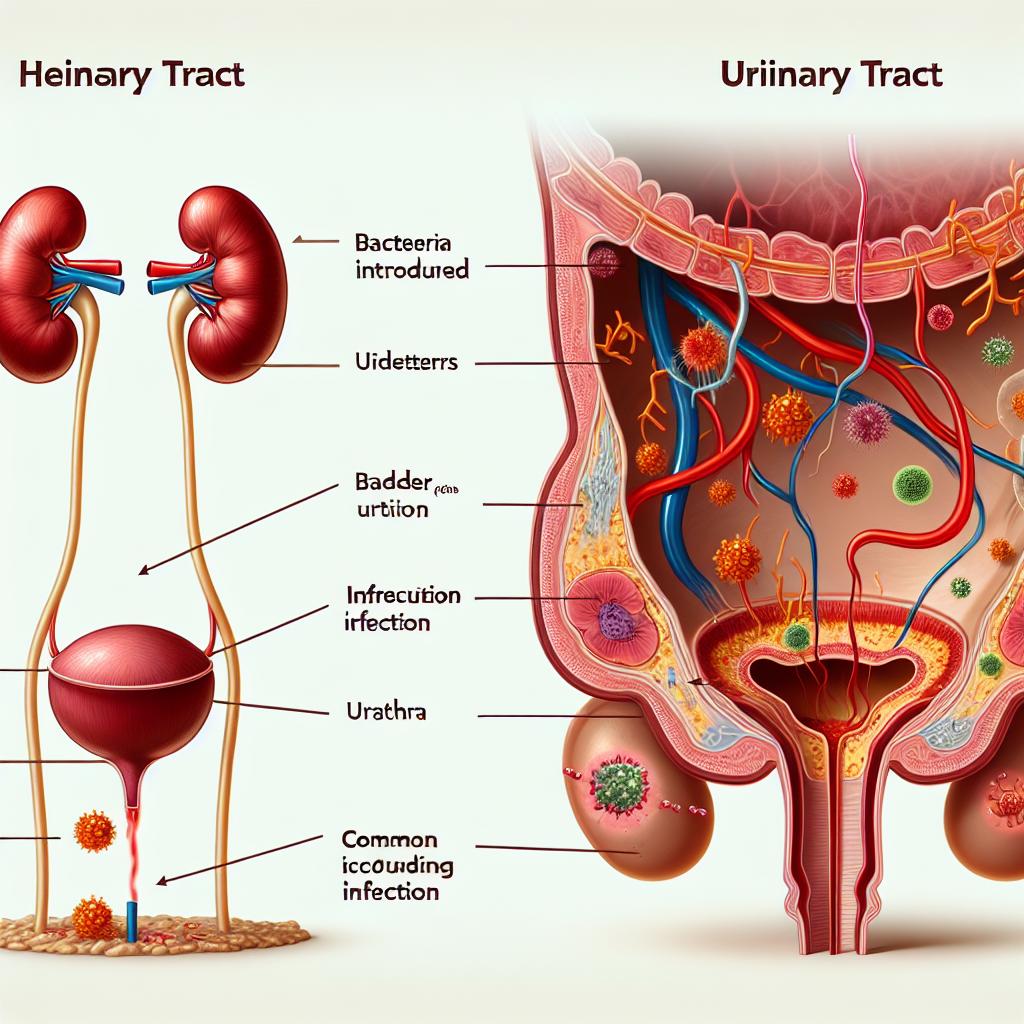
Antibiotics can influence urinary frequency through various mechanisms. The primary reason is the alteration of the gut and urinary microbiota, which can lead to changes in bladder function. Specifically, some antibiotics may disrupt the balance of beneficial bacteria in the gut and urinary tract, which can result in increased urinary urgency and frequency (Liu et al., 2024).
Moreover, certain antibiotics have diuretic effects, which can directly increase urine production. Diuretics are substances that promote the excretion of water from the body, increasing the volume of urine produced by the kidneys. This can lead to a more frequent need to urinate, especially in individuals who may already have underlying urinary issues.
Antibiotic-associated changes in the urinary tract can also lead to inflammation or irritation, contributing to an increased sensation of urgency and frequency (Abufaraj et al., 2021). As a result, patients on antibiotics may experience a noticeable increase in their need to urinate, which can be distressing and impact their daily activities.
Common Antibiotics That May Cause Frequent Urination
Several classes of antibiotics are known to potentially cause increased urination. Among these are:
-
Penicillins: Commonly used to treat infections like pneumonia and urinary tract infections (UTIs), penicillins can disrupt the natural flora of the urinary tract, leading to increased urgency and frequency (Witteman et al., 2021).
-
Cephalosporins: Similar to penicillins, cephalosporins are broad-spectrum antibiotics that can lead to urinary disturbances. They may also have mild diuretic effects, contributing further to increased urination (Smith et al., 2021).
-
Fluoroquinolones: This class includes antibiotics like ciprofloxacin and levofloxacin, which are often prescribed for UTIs. They have been associated with changes in bladder function and can lead to increased urinary urgency (Chen et al., 2020).
-
Nitrofurantoin: Frequently used for the treatment of uncomplicated UTIs, nitrofurantoin can cause bladder irritation, leading to increased urination frequency as a side effect (Jerkovic et al., 2023).
-
Tetracyclines: Known for treating a variety of infections, tetracyclines can also have impacts on urinary habits, although they are less commonly associated with increased urination compared to other classes (Mendes et al., 2017).
It is essential for patients to discuss their antibiotic use with healthcare providers, especially if they experience increased urination frequency or any other urinary symptoms.
How Antibiotics Affect Bladder Function and Urgency
Antibiotics can influence bladder function through several pathways:
-
Microbiota Disruption: The gut and urinary microbiomes play critical roles in maintaining normal bladder function. Antibiotics can disrupt these microbiomes, leading to dysbiosis, which may affect urinary symptoms. A study by Magruder et al. (2020) highlighted the connection between gut microbiota composition and urinary tract health.
-
Inflammation: Antibiotic use can lead to inflammation of the urinary tract, which can increase sensitivity and urgency. This inflammation can arise from bacterial die-off or from the introduction of new bacteria that may provoke an immune response.
-
Direct Diuretic Effects: Certain antibiotics may have diuretic properties, leading to increased urine production. This effect can be particularly pronounced in individuals with pre-existing renal issues or those taking other medications that influence fluid balance.
-
Patient Factors: Individual factors such as age, pre-existing urinary conditions, and overall health can also modulate how antibiotics affect bladder function. Older adults, for example, may be more susceptible to changes in urinary habits due to the natural decline in bladder function with age.
Managing Urination Issues While on Antibiotic Treatment
Managing increased urination frequency while on antibiotics can be challenging but is essential for maintaining quality of life. Here are several strategies:
-
Hydration Management: Drinking adequate fluids is crucial, but patients may need to balance this with the timing of fluid intake to reduce nighttime urination. Limiting fluids before bedtime can help prevent nocturia.
-
Scheduled Bathroom Visits: Establishing a regular schedule for bathroom visits can help manage urgency and frequency. Patients should attempt to void at regular intervals, even if they do not feel an urgent need to go.
-
Pelvic Floor Exercises: Engaging in pelvic floor exercises, such as Kegel exercises, can strengthen the muscles that support the bladder and improve control over urination.
-
Discussing Medication Alternatives: Patients experiencing significant urinary issues should consult their healthcare provider about possible alternatives to their current antibiotics or additional medications that can alleviate symptoms.
-
Monitoring Symptoms: Keeping a diary of urinary symptoms can help identify patterns and triggers, enabling better management strategies. Patients should report any concerning symptoms to their healthcare provider for further evaluation.
When to Consult a Doctor About Urination Changes During Antibiotics
It is vital to seek medical advice if any of the following symptoms occur while taking antibiotics:
- Persistent or worsening urinary frequency and urgency
- Painful urination or blood in the urine
- Symptoms of a urinary tract infection, such as fever or flank pain
- Symptoms that interfere significantly with daily activities or quality of life
Consulting a healthcare professional can help determine whether the symptoms are a result of antibiotic use or if they indicate a more serious underlying condition that requires treatment.
FAQ
Can all antibiotics cause increased urination frequency?
Not all antibiotics will cause increased urination frequency, but certain classes, particularly those that affect the urinary tract or have diuretic properties, may lead to this side effect.
Is it normal to experience increased urination frequency while on antibiotics?
While some increase in urination frequency can occur, it is essential to monitor any changes and consult a healthcare provider if symptoms are bothersome or concerning.
What should I do if I experience painful urination while on antibiotics?
Painful urination should be reported to a healthcare provider immediately, as it may indicate a urinary tract infection or another complication that requires treatment.
Are there any specific antibiotics known to cause increased urination frequency?
Yes, antibiotics such as nitrofurantoin, penicillins, and cephalosporins have been associated with increased urinary symptoms.
How can I manage increased urination frequency while on antibiotics?
Managing increased urination can involve strategies such as fluid management, scheduled bathroom visits, pelvic floor exercises, and discussing medication alternatives with your healthcare provider.
References
-
Liu, H., Wei, Y., Xu, Z., Lin, H., Zhao, Y., Wang, S., Gao, F., & Feng, N. (2024). Exploring Factors Affecting Acceptance of Fecal Microbiota Transplantation for Patients with Recurrent Urinary Tract Infections: a Descriptive Qualitative Study. Patient Preference and Adherence. https://doi.org/10.2147/PPA.S452328
-
Abufaraj, M., Xu, T., Cao, C., Siyam, A., Isleem, U., Massad, A., Soria, F., Shariat, S. F., Sutcliffe, S., & Yang, L. (2021). Prevalence and trends in urinary incontinence among women in the United States, 2005-2018. American Journal of Obstetrics and Gynecology, 225(2), 166.e1–166.e12. https://doi.org/10.1016/j.ajog.2021.03.016
-
Witteman, L., van Wietmarschen, H. A., & van der Werf, E. T. (2021). Complementary medicine and self-care strategies in women with (recurrent) urinary tract and vaginal infections: A cross-sectional study on use and perceived effectiveness in The Netherlands. Antibiotics, 10(3), 250. https://doi.org/10.3390/antibiotics10030250
-
Chen, H. C., Liu, C. Y., Liao, C. H., & Tsao, L. I. (2020). Self-perception of symptoms, medical help seeking, and self-help strategies of women with interstitial cystitis/painful bladder syndrome. Lower Urinary Tract Symptoms, 12(3), 183–189
-
Mendes, A., Hoga, L., Goncalves, B., Silva, P., & Pereira, P. (2017). Adult women’s experiences of urinary incontinence: A systematic review of qualitative evidence. Joanna Briggs Institute Database of Systematic Reviews and Implementation Reports, 15(5), 1350–1408
-
Smith, A. L., Chen, J., Wyman, J. F., Newman, D. K., Berry, A., Schmitz, K., Stapleton, A. E., Klusaritz, H., Lin, G., Stambakio, H., & Sutcliffe, S. (2021). Survey of lower urinary tract symptoms in United States women using the new lower urinary tract dysfunction research network symptom Index-29 (LURN-SI-29) and a national research registry. Neurourology and Urodynamics, 41(2), 650–661