Table of Contents
Symptoms Distinguishing Yeast Infections from UTIs
Yeast infections and UTIs can manifest similar symptoms, but there are key differences that can help in distinguishing between them.
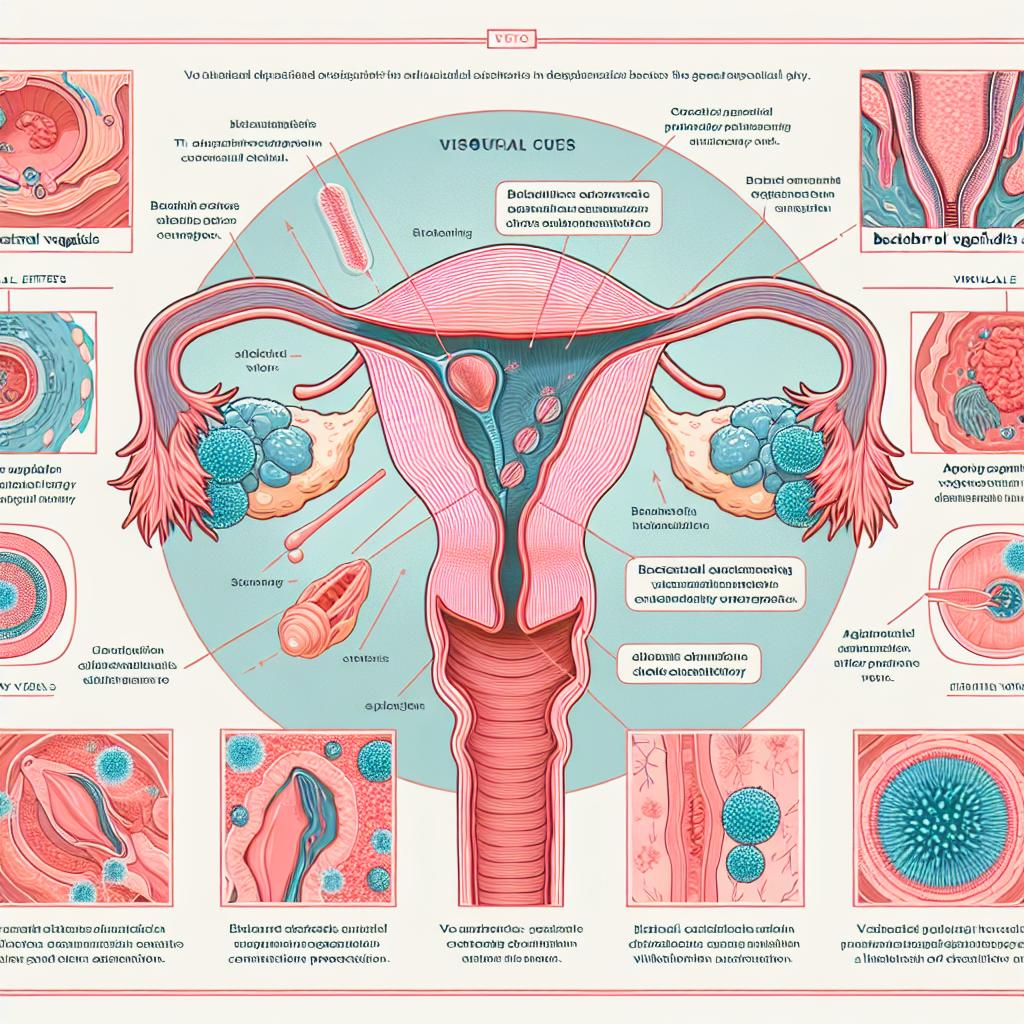
Symptoms of Yeast Infections
- Itching and Irritation: One of the most common symptoms of a yeast infection is intense itching in the vaginal area.
- Vaginal Discharge: Women may notice a thick, white discharge resembling cottage cheese, which is odorless.
- Pain During Intercourse: Discomfort or pain during sexual activity is frequently reported.
- Burning Sensation: A burning sensation during urination can also occur, but it is less common than in UTIs.
Symptoms of UTIs
- Frequent Urination: A strong urge to urinate frequently, often little urine is produced.
- Burning Sensation: A burning sensation during urination is a hallmark symptom of a UTI.
- Cloudy or Strong-Smelling Urine: The urine may appear cloudy or have a strong odor.
- Pelvic Pain: Pain or pressure in the lower abdomen may be experienced.
In a study conducted by Bhavsar et al. (2024), it was found that the symptoms of UTIs, such as dysuria and frequent urination, were often mistaken for yeast infections, highlighting the importance of accurate diagnosis (Bhavsar et al., 2024).
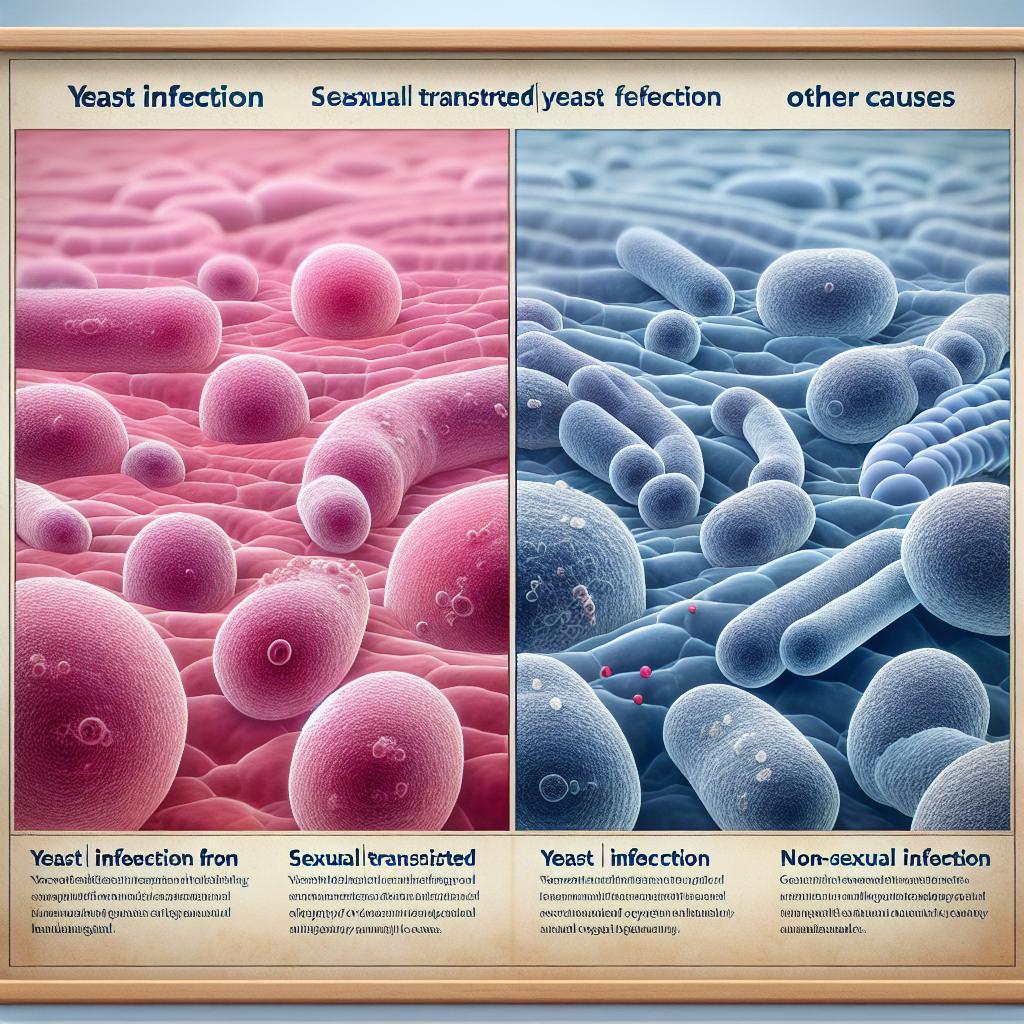
Common Causes of Yeast Infections and UTIs
Causes of Yeast Infections
Yeast infections are primarily caused by an overgrowth of Candida, a type of fungus. Factors contributing to this overgrowth include:
- Antibiotic Use: Antibiotics can disrupt the natural balance of bacteria, allowing yeast to thrive.
- Hormonal Changes: Fluctuations in hormones during menstruation, pregnancy, or menopause can increase susceptibility.
- Diabetes: High sugar levels can promote yeast growth.
- Weakened Immune System: Conditions that impair the immune system can lead to infections.
Causes of UTIs
UTIs are predominantly caused by bacteria, with Escherichia coli (E. coli) being the most common pathogen. The causes include:
- Urinary Retention: Incomplete emptying of the bladder can foster bacterial growth.
- Sexual Activity: Sexual intercourse can introduce bacteria into the urinary tract.
- Diabetes: Diabetes can increase the risk of UTIs due to the presence of excess sugar in the urine.
- Urinary Tract Abnormalities: Structural abnormalities can lead to increased infection risk (Vautrin et al., 2024).
Diagnosis Methods for Yeast Infections vs. UTIs
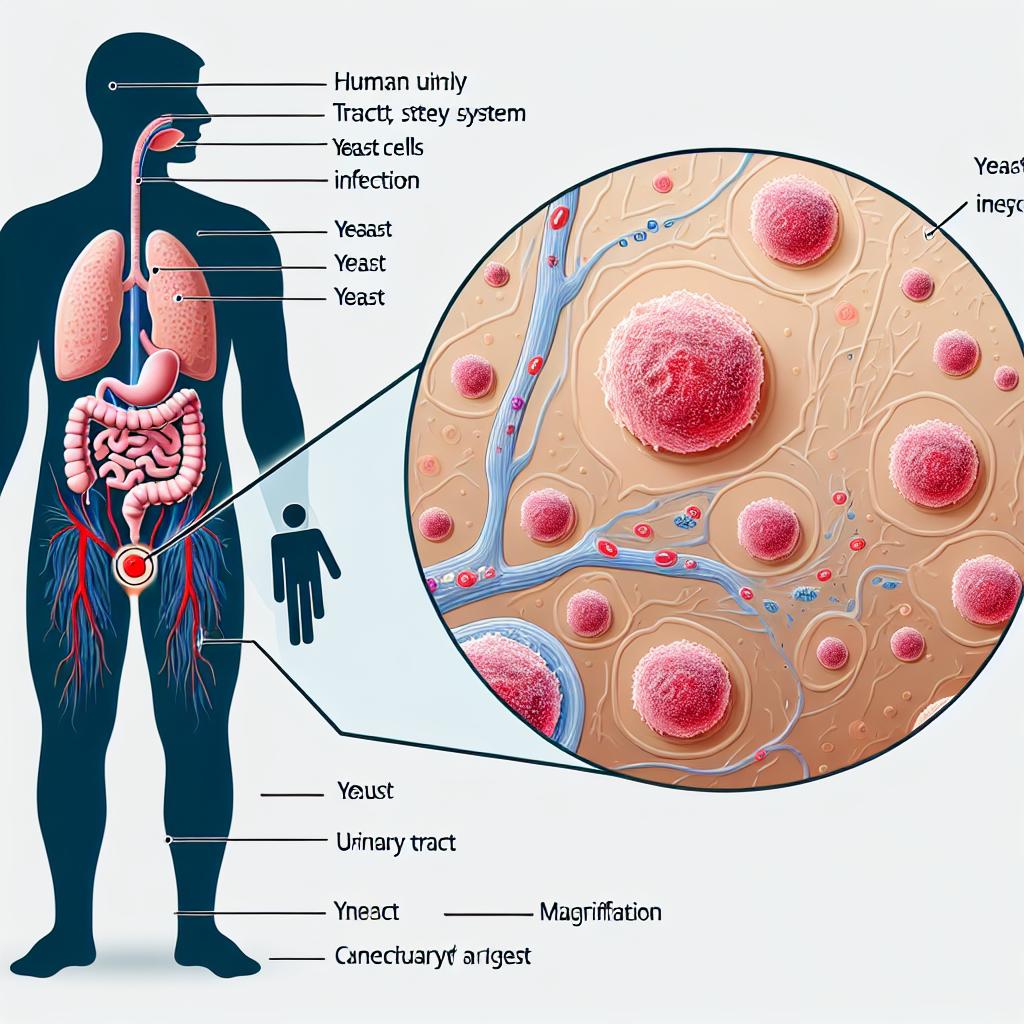
Diagnosis of Yeast Infections
Diagnosis typically involves:
- Medical History Review: Understanding symptoms and any previous infections.
- Physical Examination: Visual inspection of the vaginal area by a healthcare provider.
- Laboratory Tests: A sample of vaginal discharge may be examined under a microscope to identify yeast cells.
Diagnosis of UTIs
Diagnosing UTIs generally includes:
- Urinalysis: A dipstick test to detect the presence of nitrites, leukocytes, and blood.
- Urine Culture: Culturing urine to identify specific bacteria and their antibiotic susceptibility (Haley et al., 2024).
- Symptoms Evaluation: A thorough assessment of symptoms and their duration.
In a recent study comparing M-PCR/Pooled Antibiotic Susceptibility Testing and standard urine culture, it was shown that M-PCR provided more accurate identification of uropathogens, thus aiding in effective treatment plans for patients with complicated UTIs (Haley et al., 2024).
Treatment Options for Yeast Infections and UTIs
Treatment for Yeast Infections
- Antifungal Medications: Over-the-counter treatments, such as clotrimazole and miconazole, are commonly prescribed.
- Prescription Medications: In severe cases, fluconazole may be prescribed.
- Lifestyle Changes: Maintaining proper hygiene, wearing breathable clothing, and managing blood sugar levels can help prevent recurrence.
Treatment for UTIs
- Antibiotics: Common antibiotics for UTIs include trimethoprim/sulfamethoxazole, nitrofurantoin, and fosfomycin.
- Pain Relief: Phenazopyridine can provide symptom relief but does not treat the infection.
- Hydration: Increased fluid intake can help flush bacteria from the urinary tract.
Preventative Measures for Yeast Infections and UTIs
Prevention of Yeast Infections
- Wear Loose Clothing: Breathable fabrics can help reduce moisture.
- Limit Antibiotic Use: Only use antibiotics when necessary and under a physician’s guidance.
- Maintain Hygiene: Regular bathing and proper wiping techniques.
Prevention of UTIs
- Stay Hydrated: Drink plenty of fluids to help dilute urine and flush out bacteria.
- Urinate After Intercourse: This can help remove bacteria that may have entered the urethra.
- Wipe Front to Back: This reduces the risk of bacteria from the anal region entering the vaginal area.
FAQ
What are the main differences between a yeast infection and a UTI?
Yeast infections are caused by fungal overgrowth, usually Candida, and typically result in itching and thick discharge. UTIs are caused by bacterial infections and present with symptoms like burning during urination and frequent urination.
Can a UTI be mistaken for a yeast infection?
Yes, due to overlapping symptoms such as burning during urination, it is possible for patients to confuse the two conditions.
How are yeast infections treated?
Yeast infections are primarily treated with antifungal medications, which can be found over-the-counter or prescribed by a doctor.
What are common antibiotics used to treat UTIs?
Common antibiotics include nitrofurantoin, trimethoprim/sulfamethoxazole, and fosfomycin.
How can I prevent yeast infections and UTIs?
Preventative measures include maintaining proper hygiene, staying hydrated, and avoiding unnecessary antibiotic use.
References
- Bhavsar, S. M., Polavarapu, N., Haley, E., Luke, N., Mathur, M., Chen, X., … & Lieberman, K. (2024). Noninferiority of Multiplex Polymerase Chain Reaction Compared to Standard Urine Culture for Urinary Tract Infection Diagnosis in Pediatric Patients at Hackensack Meridian Health Children’s Hospital Emergency Department. Pediatric Health, Medicine and Therapeutics, 15, 1-8. https://doi.org/10.2147/PHMT.S491929
- Vautrin, N., Dahyot, S., Leoz, M., Caron, F., Grand, M., Feldmann, A., … & Alexandre, K. (2024). Are Escherichia coli causing recurrent cystitis just ordinary uropathogenic E. coli (UPEC) strains? Virulence, 15(1), 1-10
- Haley, E., Luke, N., Korman, H., Rao, G. S., Baunoch, D., & Mathur, M. (2024). Comparing Prescribing Behaviors and Clinician Experiences Between Multiplex PCR/Pooled Antibiotic Susceptibility Testing and Standard Urine Culture in Complicated UTI Cases. Journal of Clinical Medicine, 13(23), 1-10. https://doi.org/10.3390/jcm13237453