Table of Contents
Symptoms of UTI and Yeast Infection: How to Differentiate
Common Symptoms of UTI
UTIs primarily involve the bladder and urethra. Key symptoms include:
- Frequent Urination: A strong, persistent urge to urinate even if little comes out.
- Burning Sensation: Pain or burning during urination.
- Cloudy Urine: Urine may appear cloudy or have a strong odor.
- Pelvic Pain: Discomfort in the lower abdomen or pelvic region.
Common Symptoms of Yeast Infection
Yeast infections, particularly vulvovaginal candidiasis, primarily affect the vaginal area. Symptoms include:
- Itching and Irritation: Severe itching around the vagina and vulva.
- Abnormal Discharge: Thick, white discharge resembling cottage cheese.
- Redness and Swelling: Inflammation and swelling of the vulvar area.
- Pain during Intercourse: Discomfort during sexual activity.
Key Differences in Symptoms
While both conditions can involve discomfort and urinary symptoms, UTIs are characterized by urinary urgency and burning during urination, whereas yeast infections predominantly cause itching, irritation, and abnormal discharge (Nachum et al., 2025).
Causes of UTI vs. Yeast Infection: What You Need to Know
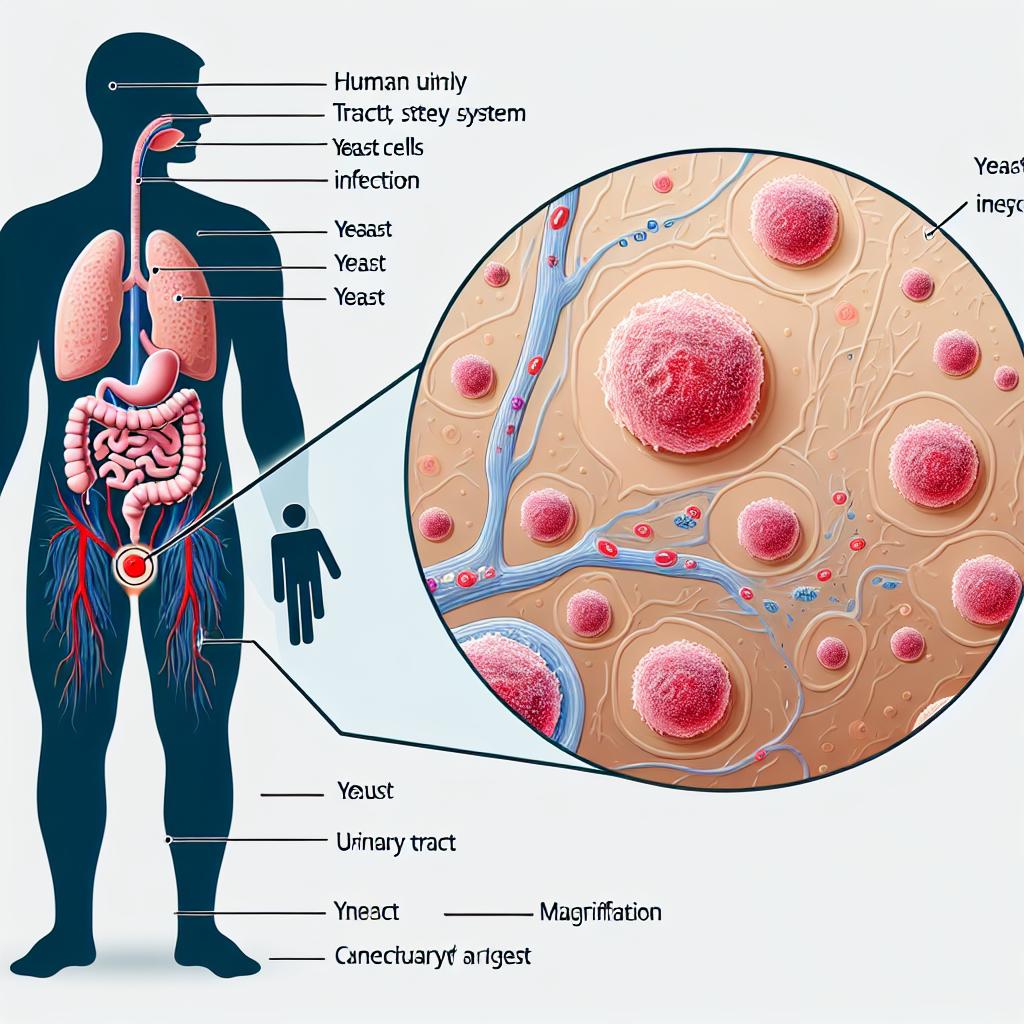
Causes of UTI
UTIs are typically caused by bacteria entering the urinary tract. The most common pathogen is Escherichia coli (E. coli), which is found in the gastrointestinal tract. Other bacteria such as Klebsiella spp. and Enterobacter spp. may also cause UTIs (Pathi et al., 2025).
Causes of Yeast Infection
Yeast infections are primarily caused by an overgrowth of Candida, a type of fungus. Factors contributing to this overgrowth include:
- Antibiotic Use: Disruption of normal vaginal flora.
- Hormonal Changes: Pregnancy, menstrual cycle, and birth control can influence yeast levels.
- Diabetes: High blood sugar levels provide a favorable environment for yeast growth.
- Immunocompromised Status: Conditions that weaken the immune system can lead to yeast infections.
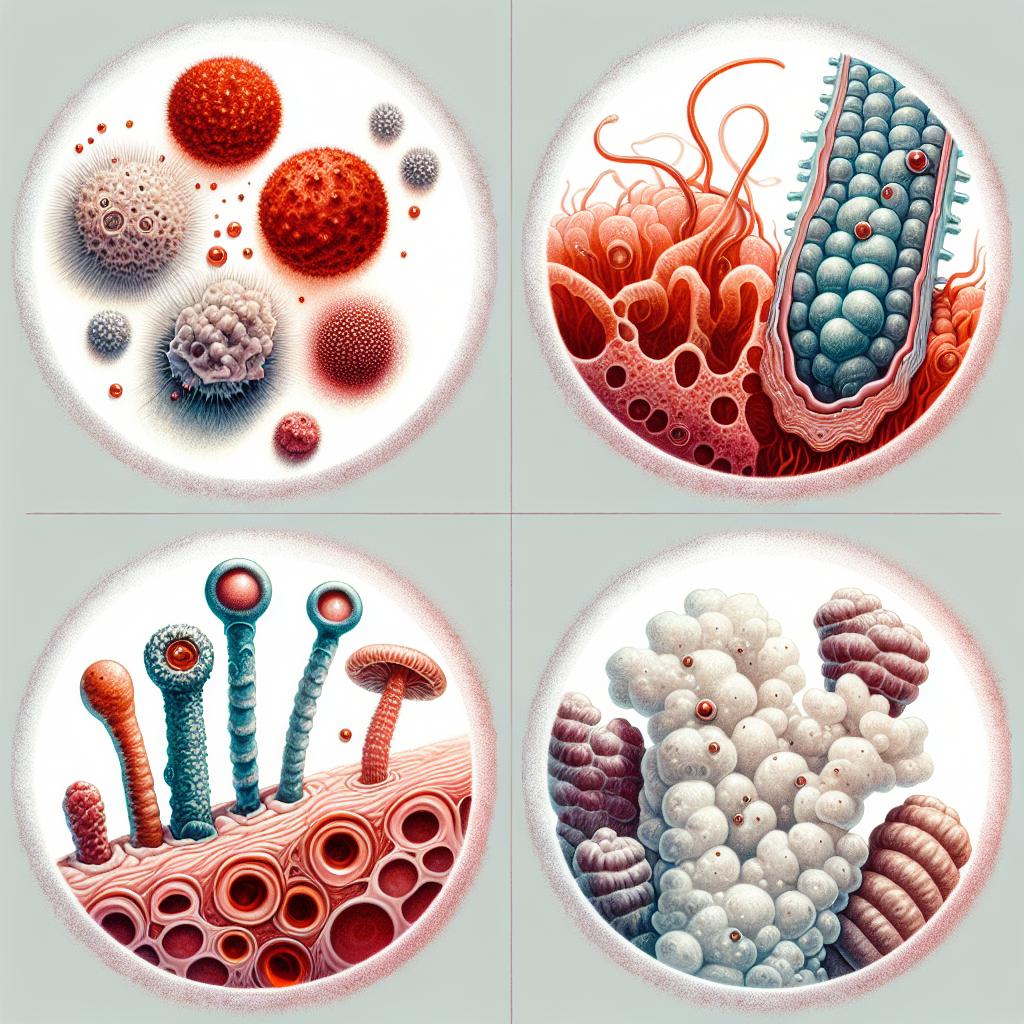
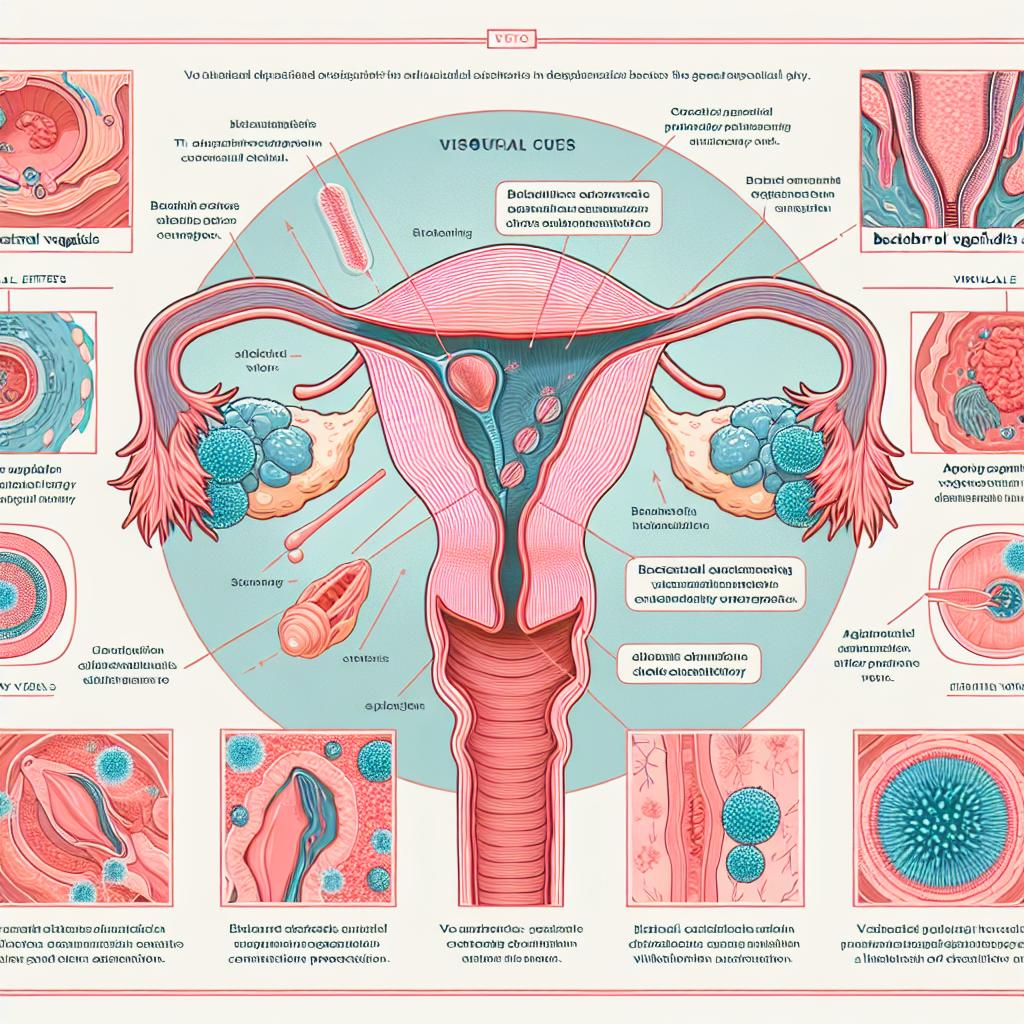
Understanding the Pathogens
The pathogens involved in UTIs and yeast infections differ significantly in their biological characteristics and treatment responses. While UTIs are bacterial and often respond to antibiotics, yeast infections require antifungal treatments.
Diagnosis Methods for UTI and Yeast Infection: A Comparison
Diagnostic Methods for UTI
- Urinalysis: A test that examines urine for signs of infection, such as white blood cells, red blood cells, and bacteria.
- Urine Culture: A culture test is performed to identify the specific bacteria causing the infection and their antibiotic susceptibility.
Diagnostic Methods for Yeast Infection
- Vaginal Swab: A sample from the vaginal area is taken to check for the presence of Candida.
- Microscopic Examination: The sample can be examined under a microscope to identify yeast cells and hyphae.
- Culture Tests: In some cases, a culture may be grown to confirm the presence of Candida (Ezenarro et al., 2025).
Key Differences in Diagnosis
UTI diagnosis focuses on urine samples and bacterial growth, while yeast infections rely on vaginal samples and microscopic examination.
Treatment Options for UTI and Yeast Infection: What Works Best
Treatment for UTI
- Antibiotics: The primary treatment for UTIs. Common antibiotics include:
- Nitrofurantoin
- Trimethoprim-sulfamethoxazole
- Ciprofloxacin
- Symptomatic Relief: Pain relief medications may be prescribed to alleviate urinary discomfort.
Treatment for Yeast Infection
- Antifungal Medications: The standard treatment for yeast infections includes:
- Topical Antifungals: Such as clotrimazole and miconazole applied directly to the affected area.
- Oral Antifungals: Fluconazole is often prescribed for more severe cases.
Key Differences in Treatment
The treatment for UTIs is antibiotic-based, while yeast infections require antifungal medication. Misdiagnosis can lead to inappropriate treatment, worsening symptoms, and increasing resistance patterns (Ghorbani et al., 2023).
Conclusion
Understanding the differences between UTIs and yeast infections is vital for proper diagnosis and treatment. While both conditions can cause discomfort and share some overlapping symptoms, their underlying causes, diagnostic methods, and treatment approaches are distinct. If symptoms persist or worsen, seeking medical attention is essential for effective management.
Frequently Asked Questions (FAQ)
Can a UTI cause a yeast infection? Yes, antibiotics used to treat UTIs can disrupt the normal vaginal flora, leading to an overgrowth of yeast.
Are UTIs and yeast infections contagious? No, neither condition is considered contagious. UTIs are caused by bacteria that are typically present in the body, while yeast infections are caused by an overgrowth of fungi that are also naturally present.
How can I prevent UTIs and yeast infections? Maintaining good personal hygiene, staying hydrated, urinating after intercourse, and wearing breathable cotton underwear can help reduce the risk of both conditions.
When should I see a doctor? If you experience severe symptoms, such as fever, back pain, or persistent urinary symptoms, it’s important to seek medical attention promptly.
References
-
Nachum, Z., Suleiman, A., Colodner, R., Battino, S., Wattad, M., Kuzmin, O., & Yefet, E. (2025). Oral Probiotics to Prevent Recurrent Vulvovaginal Infections During Pregnancy—Multicenter Double-Blind, Randomized, Placebo-Controlled Trial. Nutrients, 17(3), 460. https://doi.org/10.3390/nu17030460
-
Pathi, B. K., Mohapatra, I., Sharma, V., & Panigrahi, K. (2025). Antimicrobial Sensitivity Patterns of Bacteria Causing Urinary Tract Infections: A Retrospective Study of Elderly Patients Admitted to a Tertiary Care Hospital in Bhubaneswar, India. Cureus, 12(6), e77399. https://doi.org/10.7759/cureus.77399
-
Ghorbani, M., Mohammadi, M., & Mohammadi, M. (2023). Antifungal Lock Therapy: An Eternal Promise or an Effective Alternative Therapeutic Approach? Gels, 11(1), 23. https://doi.org/10.3390/gels11010023
-
Ezenarro, J. J., Al Ktash, M., Vigues, N., Gordi, J. M., Muñoz-Berbel, X., & Brecht, M. (2025). Spectroscopic characterization of bacterial colonies through UV hyperspectral imaging techniques. Frontiers in Chemistry, 11, 1530955. https://doi.org/10.3389/fchem.2025.1530955
-
Sadanandan, B., Vijayalakshmi, V., Ashrit, P., & Kumar, L. M. S. (2025). In Situ Aqueous Spice Extract-Based Antifungal Lock Strategy for Salvage of Foley’s Catheter Biofouled with Candida albicans Biofilm Gel. Gels, 11(1), 23. https://doi.org/10.3390/gels11010023