Table of Contents
Definition and Key Characteristics of Orthostatic Proteinuria
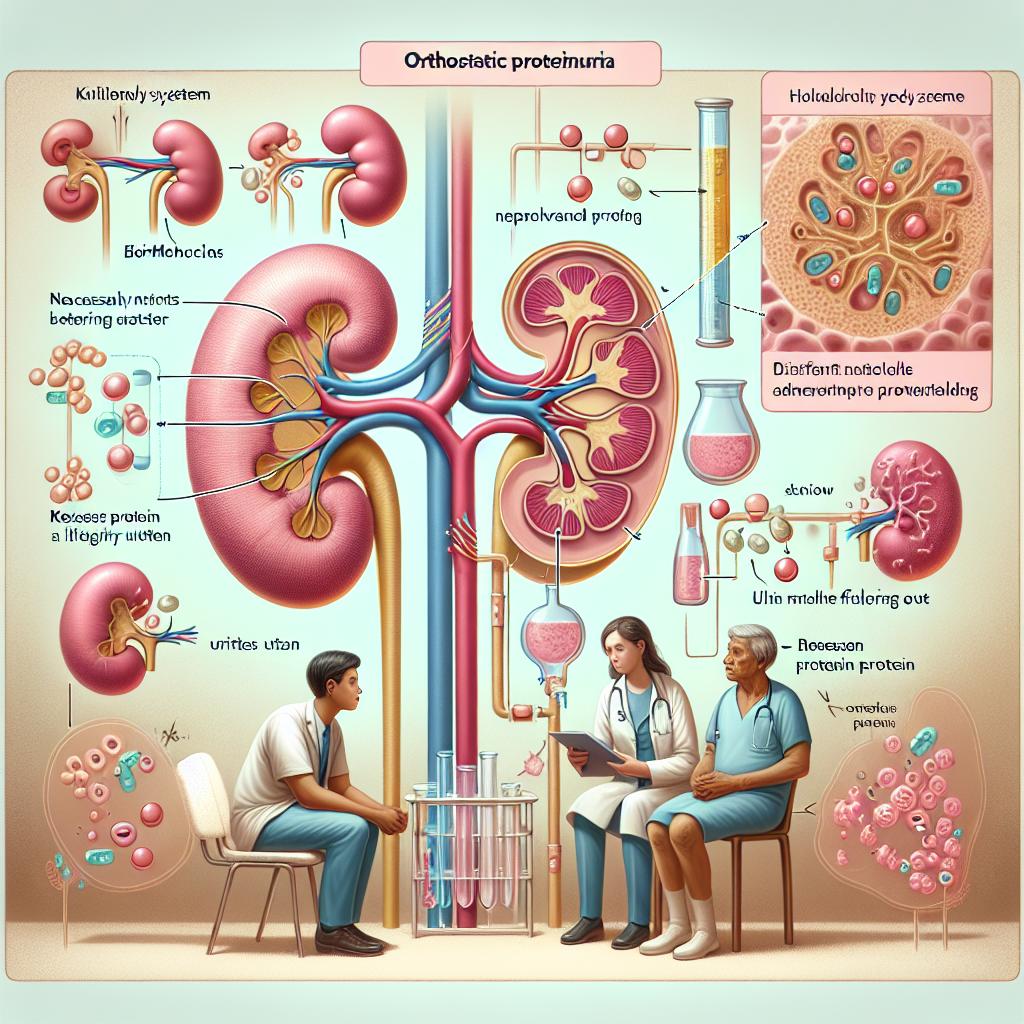
Orthostatic proteinuria (OP) is a benign condition characterized by the presence of protein in the urine, which occurs primarily when a person is in an upright position. This condition is most commonly observed in adolescents and young adults. In OP, protein levels in urine are typically normal when the patient is lying down but increase significantly upon standing. This phenomenon is thought to be linked to the physiological changes that occur with posture, particularly in the renal hemodynamics and glomerular filtration rate (GFR) [1].
Patients with OP often exhibit no other symptoms, and the condition is usually discovered incidentally during routine urinalysis or investigations for other conditions. The proteinuria in OP is generally non-nephrotic, meaning that the quantity of protein present is not sufficient to cause significant renal impairment or albuminuria that would typically be associated with more serious kidney diseases. Diagnosis is often confirmed through a 24-hour urine collection that shows elevated protein levels only in the upright position, distinguishing it from other forms of proteinuria associated with systemic diseases [2].
Causes and Risk Factors Associated with Orthostatic Proteinuria
Multiple factors contribute to the development of orthostatic proteinuria. The most common risk factors include:
- Age: OP is predominantly seen in adolescents and young adults, particularly those between the ages of 10 and 25.
- Postural Changes: The act of standing can induce venous pooling and alter renal blood flow, which may lead to increased protein filtration in susceptible individuals.
- Physical Activity: Strenuous exercise or prolonged standing can exacerbate the condition, leading to transient increases in urinary protein levels.
- Genetic Predisposition: Familial cases have been documented, suggesting a possible genetic component to the disorder.
- Environmental Factors: Situations that lead to dehydration or orthostatic stress can precipitate or worsen proteinuria in susceptible individuals [3].
Understanding these risk factors is essential for identifying and managing patients at risk for OP.
Diagnostic Approaches for Identifying Orthostatic Proteinuria
The diagnostic process for orthostatic proteinuria typically involves the following steps:
-
Initial Urinalysis: A routine urinalysis may reveal the presence of protein. However, additional tests are required to confirm OP.
-
24-Hour Urine Collection: This is a crucial test where urine is collected over a 24-hour period. In patients suspected of having OP, two separate collections are typically conducted: one while lying down and another while standing [4].
-
Postural Tests: Measuring the protein concentration in urine during different postures helps distinguish OP from other types of proteinuria. For example, a significant increase in protein levels when standing compared to lying down supports a diagnosis of OP.
-
Exclusion of Other Causes: It is vital to rule out other potential causes of proteinuria, such as diabetic nephropathy, glomerulonephritis, and other systemic conditions that may lead to renal impairment. This can be achieved through blood tests, imaging studies, and sometimes renal biopsy if indicated [5].
-
Follow-up: Regular monitoring of urinary protein levels over time can help confirm the diagnosis and assess the condition’s progression or resolution.
Treatment Options and Management Strategies for Orthostatic Proteinuria
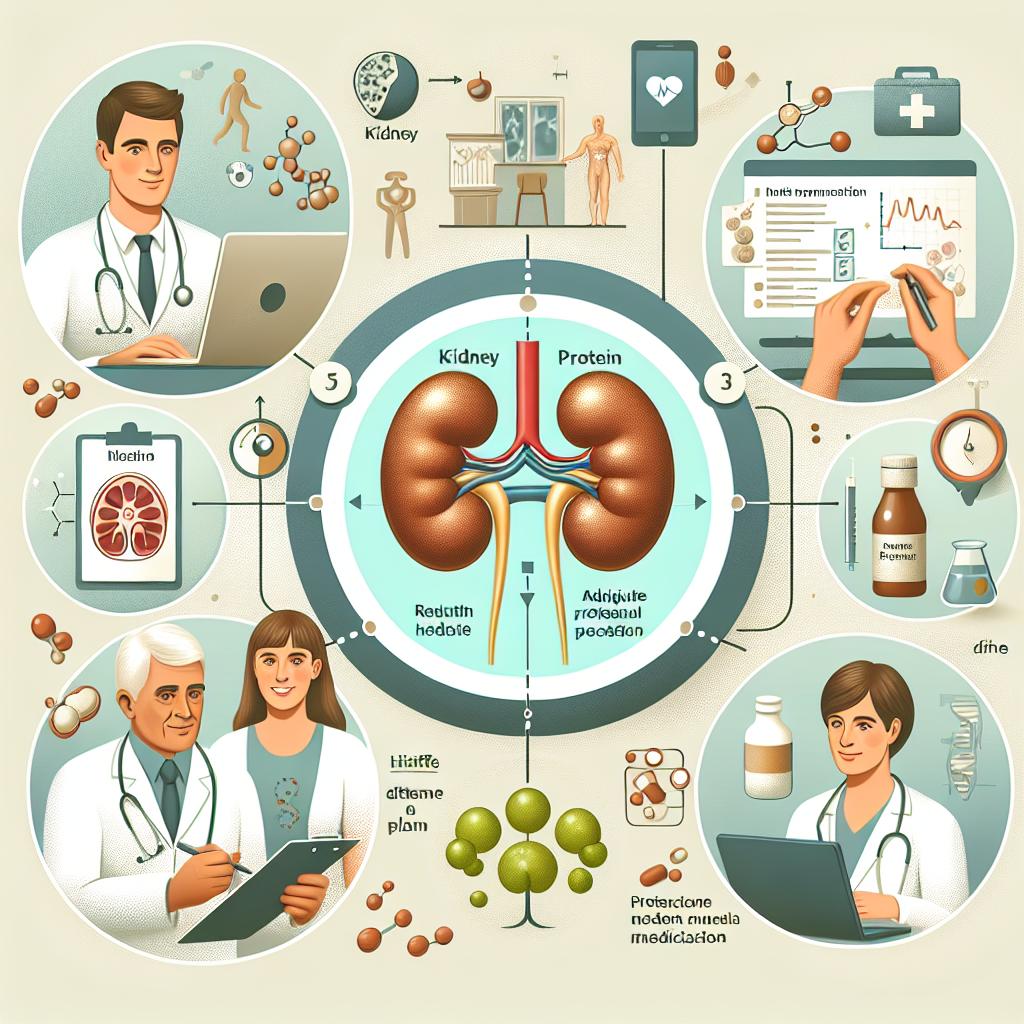
The management of orthostatic proteinuria is primarily supportive, as the condition is generally benign and self-limiting. Here are some common strategies:
-
Lifestyle Modifications: Patients are often advised to increase fluid intake to prevent dehydration, especially before engaging in activities that require prolonged standing.
-
Education and Reassurance: Informing patients and their families about the benign nature of OP can alleviate anxiety associated with the diagnosis. Regular follow-ups can help monitor the condition and ensure patients understand the importance of hydration.
-
Physical Therapy: For patients who experience symptoms associated with postural changes, physical therapy may be helpful in improving overall stability and managing symptoms related to orthostatic intolerance [6].
-
Observation: In many cases, OP resolves spontaneously as patients age. Regular monitoring may be all that is required in mild cases.
-
Medications: While pharmacological intervention is not typically necessary for OP, in cases where symptoms are significant, medications that improve blood volume or pressure may be considered. However, these are not commonly required.
Long-term Prognosis and Impact of Orthostatic Proteinuria on Health
The long-term prognosis for individuals with orthostatic proteinuria is generally favorable. Most patients do not progress to chronic kidney disease or other renal disorders. However, there are a few considerations to keep in mind:
-
Monitoring: Regular follow-up tests are essential to ensure that protein levels remain stable and that no other renal pathology develops over time.
-
Impact on Quality of Life: While OP is usually asymptomatic, some patients may experience anxiety related to their diagnosis. Education and reassurance play crucial roles in mitigating these concerns.
-
Potential Associations: Research suggests that while OP itself is benign, it may be associated with other conditions, such as hypermobility syndromes, which could require further evaluation and management [7].
-
Psychosocial Factors: The diagnosis of OP can have psychological effects on patients, particularly adolescents who may feel different from their peers. Providing appropriate support and counseling can be beneficial.
FAQ
Can orthostatic proteinuria lead to chronic kidney disease?
No, orthostatic proteinuria is typically benign and does not lead to chronic kidney disease.
How is orthostatic proteinuria diagnosed?
Diagnosis is mainly through urinalysis, 24-hour urine collection while standing and lying down, and exclusion of other causes of proteinuri
What lifestyle changes can help manage orthostatic proteinuria?
Increasing fluid intake and avoiding prolonged standing or strenuous exercise may help manage symptoms.
Is treatment necessary for orthostatic proteinuria?
Most cases do not require treatment; management is usually supportive and involves monitoring.
At what age does orthostatic proteinuria usually resolve?
Orthostatic proteinuria often resolves by late adolescence or early adulthood.
References
-
de Carvalho, M., et al. (2024). Brazilian Guidelines on evaluation and clinical management of Nephrolithiasis: Brazilian Society of Nephrology. https://pubmed.ncbi.nlm.nih.gov/11913452/
-
da Luz, L. G., et al. (2024). A Rare Presentation of Sjögren’s Syndrome With Hypokalemic Periodic Paralysis Treated Based on Renal Biopsy Findings. https://doi.org/10.7759/cureus.79404
-
González-Pérez, A., et al. (2025). Proton Pump Inhibitor Use and Worsening Kidney Function: A Retrospective Cohort Study Including 122,606 Acid-Suppressing Users. https://doi.org/10.1007/s11606-024-09213-8
-
Alladin-Karan, A., et al. (2025). Is Childhood IgA Nephropathy Different From Adult IgA Nephropathy? A Narrative Review. https://pubmed.ncbi.nlm.nih.gov/11898040/
-
Tang, J., et al. (2025). Prevalence of metabolic syndrome in people living with HIV and its multi-organ damage: a prospective cohort study. https://doi.org/10.1186/s12879-025-10735-7
-
Santos, S., et al. (2025). Anemia in Elderly Patients: Contribution of Renal Aging and Chronic Kidney Disease. https://doi.org/10.3390/geriatrics10020043
-
Lee, M. A., et al. (2024). How obesity and metabolic syndrome affect cardiovascular events, progression to kidney failure and all-cause mortality in chronic kidney disease. Nephrol Dial Transpl.