Table of Contents
Overview of Blood Types and Their Importance
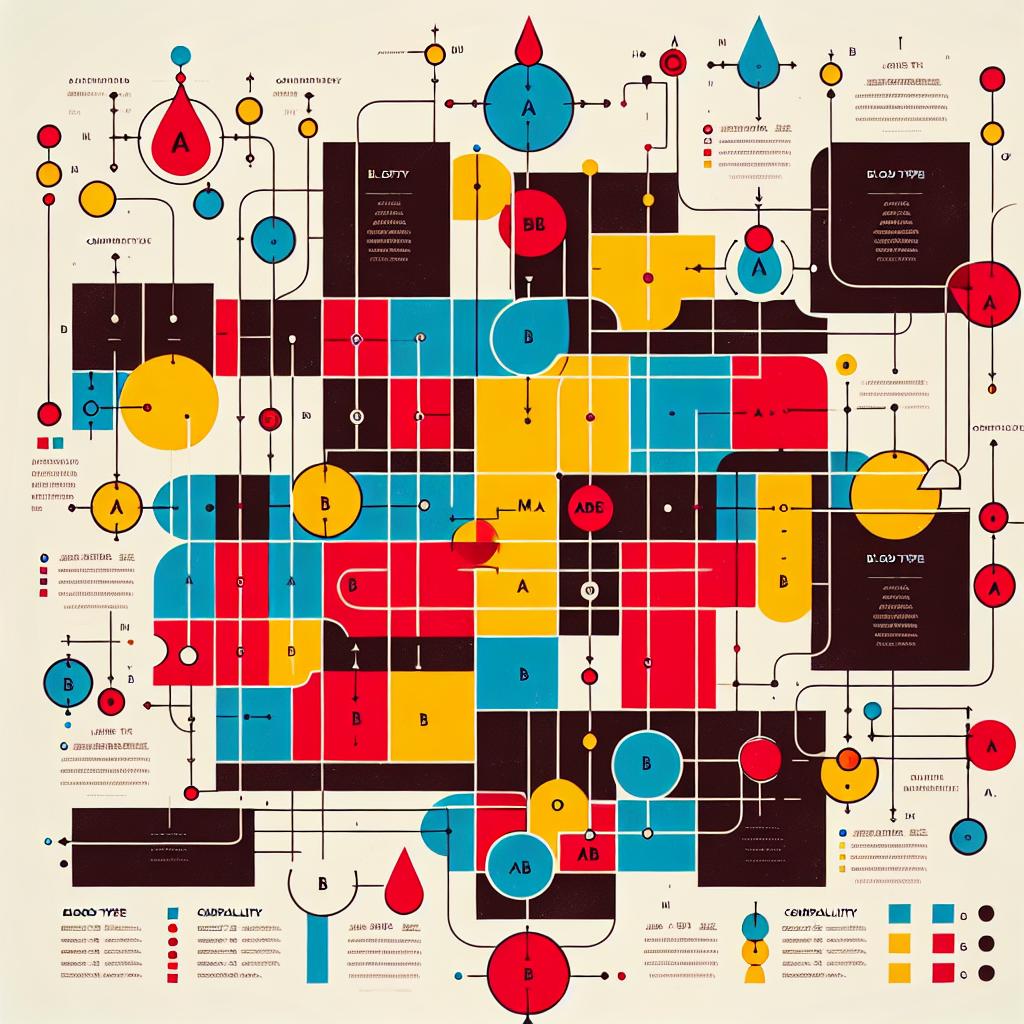
Blood types play a crucial role in human health, influencing everything from blood transfusions to organ transplants, and even certain disease susceptibilities. The primary blood group systems are the ABO system and the Rh system. The ABO blood group system categorizes blood into four main types: A, B, AB, and O, based on the presence or absence of specific antigens. Meanwhile, the Rh system classifies blood as either Rh-positive or Rh-negative, depending on the presence of the Rh factor (D antigen) on the surface of red blood cells.
Understanding blood types is vital in medical settings, particularly in emergencies where blood transfusions are necessary. For instance, individuals with type O blood are considered universal donors because their blood can be given to any other blood type without causing an adverse reaction. Conversely, AB positive individuals are universal recipients, able to receive blood from any type. This compatibility is essential not only for patient safety but also for effective treatment outcomes. Given the complexities involved in blood transfusions and organ transplants, a comprehensive understanding of blood type compatibility is essential for healthcare providers and patients alike.
Detailed Blood Type Chart: Key Information at a Glance
| Blood Type | A Antigen | B Antigen | AB Antigen | O Antigen | Rh Factor | Compatibility (Donor → Recipient) |
|---|---|---|---|---|---|---|
| A | Present | Absent | Absent | Absent | Positive/Negative | A, AB |
| B | Absent | Present | Absent | Absent | Positive/Negative | B, AB |
| AB | Present | Present | Absent | Absent | Positive/Negative | AB |
| O | Absent | Absent | Absent | Present | Positive/Negative | O, A, B, AB |
This chart provides a clear overview of blood type characteristics, including antigens present or absent and compatibility for transfusions. Understanding these factors is essential for ensuring safe transfusions and avoiding complications such as hemolytic reactions.
Understanding Blood Type Compatibility for Transfusions
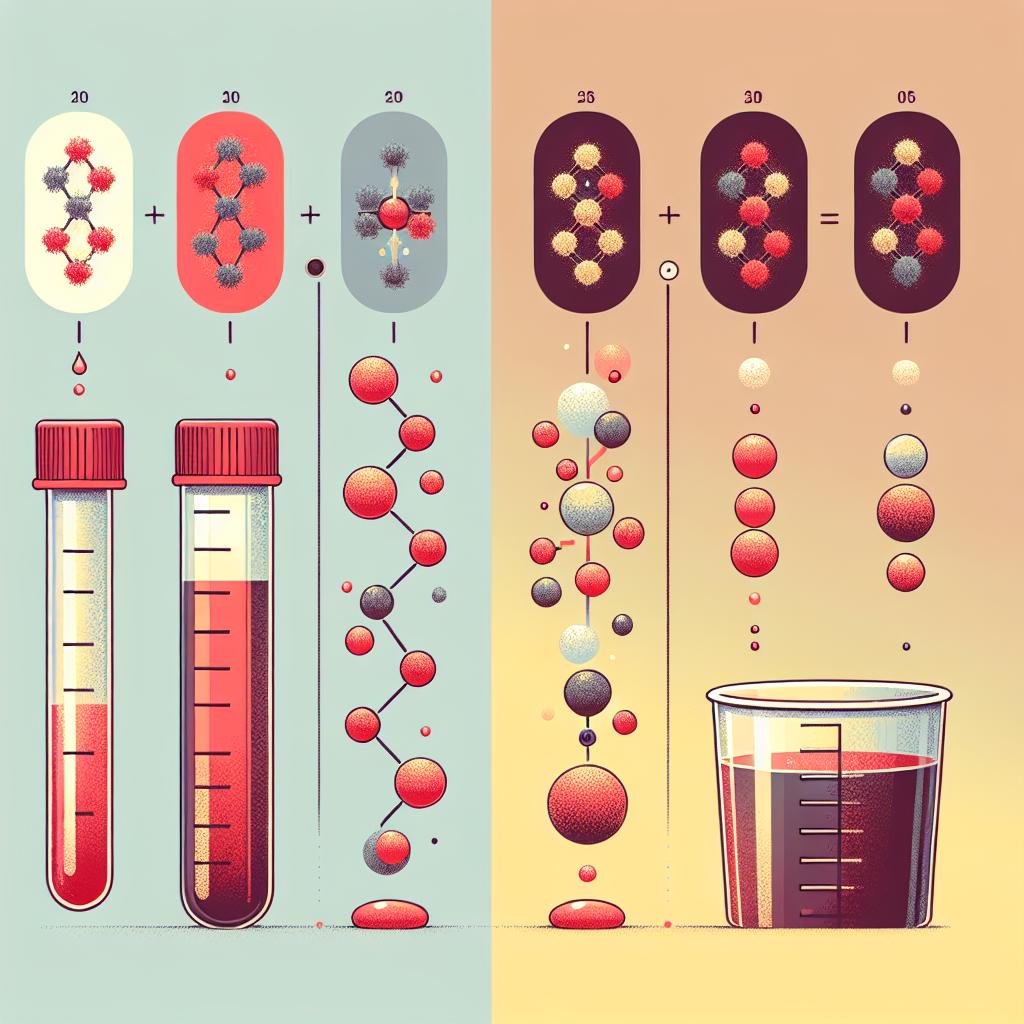
Blood type compatibility is determined by the presence or absence of specific antigens on the surface of red blood cells. When a person receives a blood transfusion, the donor’s blood must not contain antigens that the recipient’s immune system recognizes as foreign. For example, if a type A individual receives type B blood, their immune system will attack the transfused blood cells, leading to potentially fatal complications.
In addition to the ABO blood group, the Rh factor is crucial in determining compatibility. Rh-positive blood contains the Rh antigen, while Rh-negative blood does not. An Rh-negative person can develop antibodies against Rh-positive blood if exposed. Therefore, Rh-negative individuals should ideally receive Rh-negative blood to prevent hemolytic reactions.
| Donor Type | Recipient Type | Compatibility |
|---|---|---|
| A+ | A+, A-, AB+, AB- | Compatible |
| A- | A-, AB- | Compatible |
| B+ | B+, B-, AB+, AB- | Compatible |
| B- | B-, AB- | Compatible |
| AB+ | AB+ | Compatible |
| AB- | AB- | Compatible |
| O+ | O+, A+, B+, AB+ | Compatible |
| O- | O-, A-, B-, AB- | Compatible |
This table illustrates the complexities of blood type compatibility in transfusions. It is crucial for healthcare providers to have access to accurate blood type information to minimize risks during transfusions.
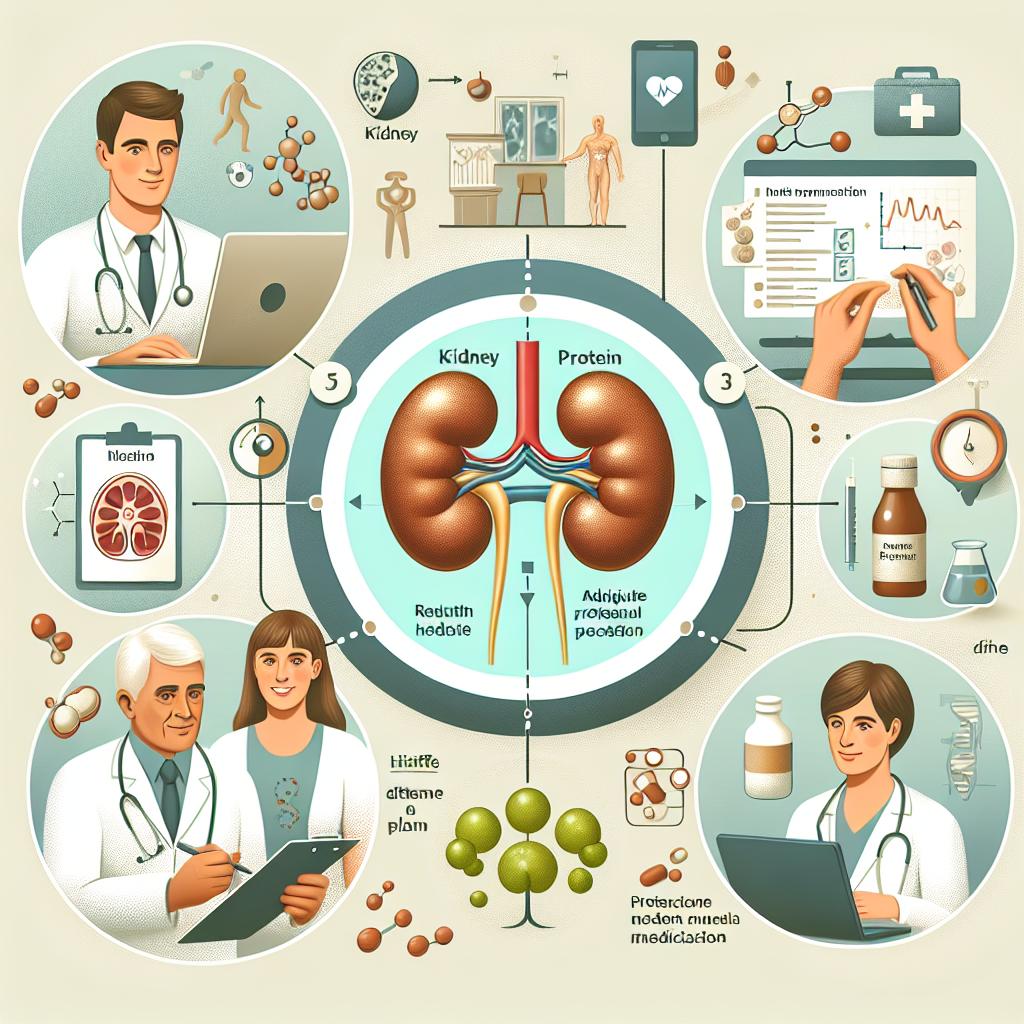
How Blood Types Affect Health and Disease Risk
Research has shown that blood types may influence susceptibility to certain diseases and health conditions. For example, individuals with type O blood may be less likely to develop blood clots, while those with type A blood may have a higher risk of cardiovascular diseases. Furthermore, studies have indicated that blood type can impact the effectiveness of certain vaccines, including those against viruses like influenza.
A recent study highlighted the relationship between blood type and susceptibility to infectious diseases, particularly COVID-19. Research indicates that individuals with type A blood may have a higher risk of severe infection compared to those with type O blood. While more studies are necessary to confirm these findings, they underscore the importance of blood type in overall health and disease management.
Frequently Asked Questions About Blood Types and Chart Usage
What is the most common blood type?
Type O is the most common blood type worldwide, followed by type A, type B, and type AB.
Can a person with type O blood donate to anyone?
Yes, individuals with type O negative blood are universal donors, as their blood lacks A and B antigens.
Why is it important to know my blood type?
Knowing your blood type is crucial for safe blood transfusions, organ transplants, and understanding any potential health risks associated with your blood type.
Are blood types inherited?
Yes, blood types are inherited from your parents based on the combination of alleles they pass on.
How can I find out my blood type?
You can determine your blood type through a blood test at a healthcare facility or by using home testing kits available at pharmacies.
References
-
Abu-Yousef, M. M., Narayana, A. S., & Brown, R. C. (1984). Catheter-induced cystitis: evaluation by cystosonography. Radiology, 151(2), 471-473 (https://doi.org/10.1148/radiology.151.2.6709921)
-
Ekelund, P., & Johansson, S. (1979). Polypoid cystitis: a catheter associated lesion of the human bladder
-
Goble, N. M., Clarke, T., & Hammonds, J. C. (1989). Histological changes in the urinary bladder secondary to urethral catheterisation
-
Grocela, J. A., & Jura, Y. H. (2010). Top-vented urinary drainage catheters cause fewer epithelial and vascular changes in the bladder mucosa compared to conventional catheters and may reduce susceptibility to urinary tract infections
-
Norlén, L. J., Ekelund, P., Hedelin, H., & Johansson, S. L. (1988). Effects of indwelling catheters on the urethral mucosa (polypoid urethritis)
-
Shey, H. H., & Bors, E. (1966). PSEUDOPAPILLOMATA OF LOWER URINARY TRACT COMPLICATING SPINAL CORD INJURIES
-
Ekelund, P., Anderstrom, C., Johansson, S. L., & Larsson, P. (1983). The reversibility of catheter-associated polypoid cystitis 17)51248-3)
-
Wall, B. M., Dmochowski, R. R., Malecha, M., et al. (2001). Inducible nitric oxide synthase in the bladder of spinal cord injured patients with a chronic indwelling urinary catheter 01)00799-2)
-
Palma, D., Guillaumes, M., Pericas, C., et al. (2025). A new STI in the city: MPOX in Barcelona. First outbreak (5/2022-5/2023) and subsequent resurgence. PLOS ONE, 39(1), e0296141. https://doi.org/10.1371/journal.pone.0296141
-
Chang, H., Tao, Q., Wei, L., Wang, Y., & Tu, C. (2025). Spatiotemporal landscape of kidney in a mouse model of hyperuricemia at single‐cell level
-
Göransson, K. E., von Vogelsang, A.-C., & Engström, G. (2025). Mucosal injuries from indwelling catheters: A scoping review. PLOS ONE, 39(1), e0317501. https://doi.org/10.1371/journal.pone.0317501
-
Fadeyi, A. et al. (2024). Prevalence and Mitigation of Cardiovascular Disease Risk Factors Among the Corporate Workforce in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Cureus, 12(2), e75888. https://doi.org/10.7759/cureus.75888