Table of Contents
What is a Urinary Tract Infection (UTI)?
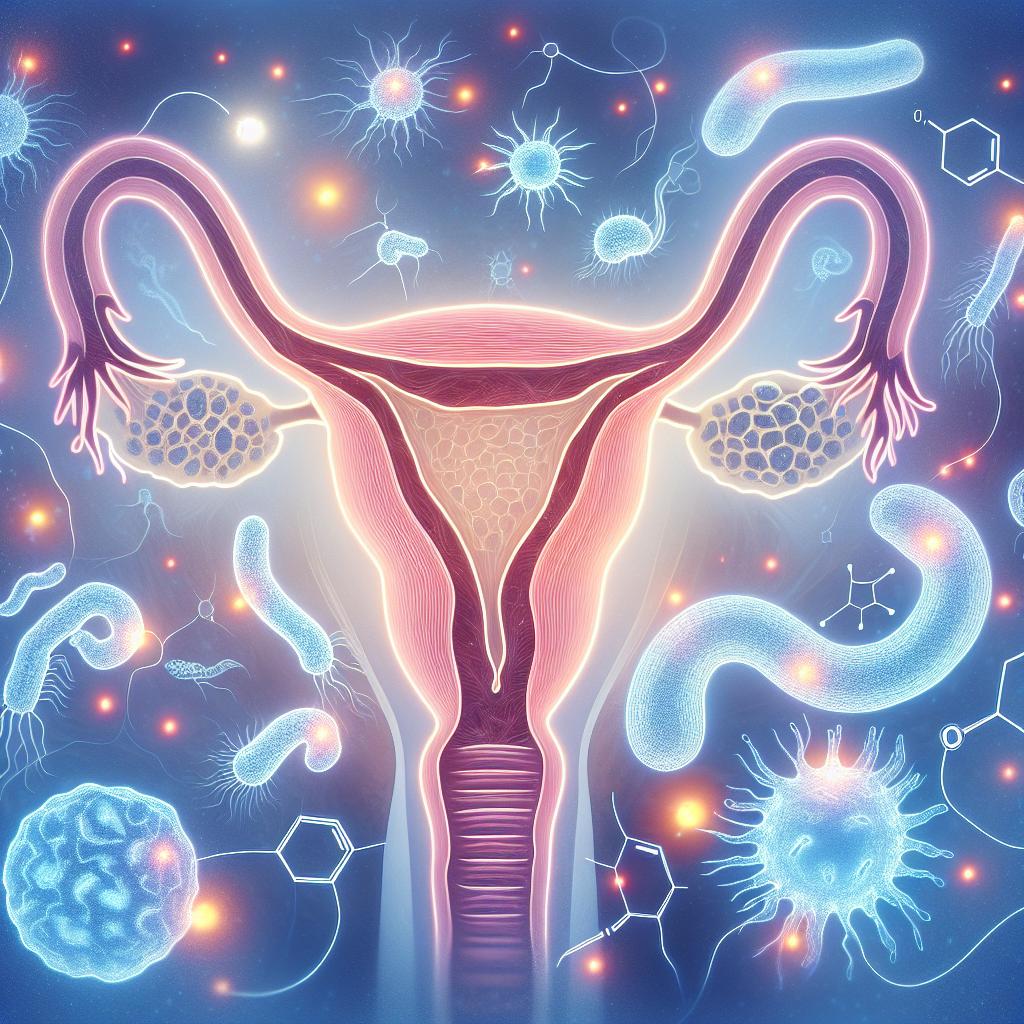
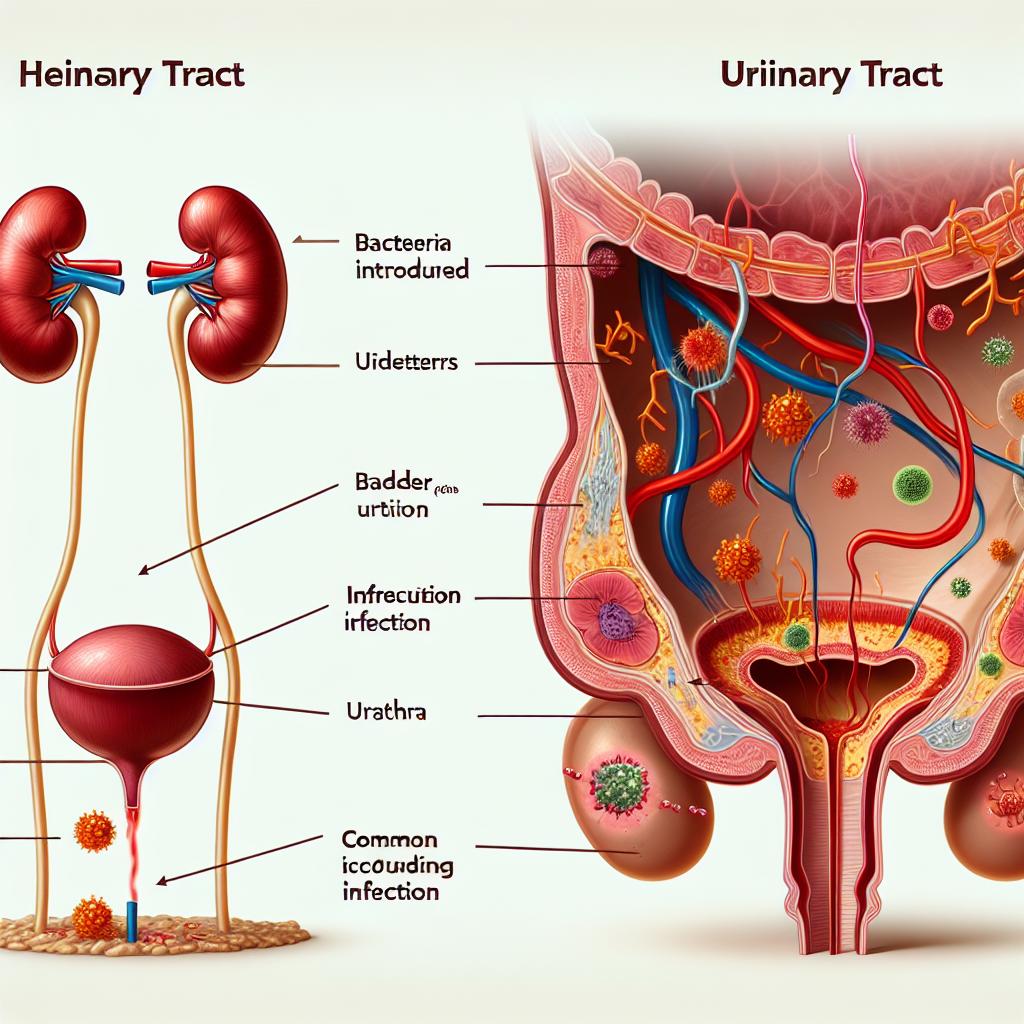
A Urinary Tract Infection (UTI) is a common medical condition that occurs when harmful bacteria invade the urinary tract, which includes the kidneys, ureters, bladder, and urethra. UTIs are primarily caused by the bacterium Escherichia coli (E. coli), which resides in the intestines but can migrate to the urinary tract, leading to infection. UTIs can affect anyone but are particularly prevalent among women due to their anatomical structure; the female urethra is shorter, allowing easier access for bacteria to reach the bladder.
The condition can manifest in various forms, such as cystitis (bladder infection) and pyelonephritis (kidney infection), each with its unique symptoms and severity. UTIs can be acute or recurrent, with recurrent infections defined as two or more UTIs within six months or three or more in a year. According to recent studies, nearly 60% of women will experience at least one UTI in their lifetime, making awareness and understanding of the condition crucial for effective management and prevention.
Symptoms of a UTI You Should Know
Recognizing the symptoms of a UTI is vital for early diagnosis and treatment. Common symptoms include:
- Frequent Urination: An increased urge to urinate, often accompanied by a small quantity of urine.
- Burning Sensation: A painful or burning sensation during urination, medically referred to as dysuria.
- Cloudy or Foul-Smelling Urine: The presence of bacteria and pus in the urine can lead to changes in color and odor.
- Blood in Urine: Hematuria, or blood in the urine, may occur, indicating a more severe infection.
- Pelvic Pain: Discomfort or pressure in the lower abdomen, often associated with bladder infections.
- Fever and Chills: In severe cases, systemic symptoms like fever and chills can occur, indicating that the infection may have reached the kidneys.
It’s essential to seek medical attention if you experience any of these symptoms, particularly if they are severe or persistent. Early intervention can prevent complications and lead to more effective treatment options.
Risks of Having Sex With a UTI
Having sex with a UTI is generally not advisable due to several risks associated with the condition. Engaging in sexual activity can exacerbate the symptoms of a UTI and potentially lead to more severe complications. Here are some of the key risks to consider:
Increased Discomfort and Pain
Intimacy during a UTI can lead to increased discomfort and pain. The inflammation and irritation of the urethra can be aggravated by sexual activity, making the already painful symptoms of dysuria and pelvic discomfort worse. Many individuals report that sexual intercourse during a UTI is painful, and the fear of pain can lead to anxiety surrounding intimacy.
Risk of Complications
Having sex with an active UTI can heighten the risk of complications, such as the infection spreading to the kidneys. Pyelonephritis, a severe form of UTI that affects the kidneys, can occur if the bacteria travel up the urinary tract. Symptoms of kidney infection include high fever, chills, and severe back pain, which require immediate medical attention.
Transmission of Bacteria
During sexual activity, bacteria can be transmitted back into the urinary tract, potentially worsening the infection or leading to new infections. This is particularly concerning for individuals with recurrent Utis, as the introduction of more bacteria can complicate treatment and prolong recovery.
Psychological Impact
The discomfort associated with having a UTI can create psychological barriers to intimacy. Anxiety, fear of pain, and embarrassment may lead to decreased libido and strain relationships. Open communication with partners about the condition and its effects is crucial for maintaining intimacy and understanding.
Given these risks, it is advisable to avoid sexual activity until the UTI has been effectively treated and symptoms have resolved. Consulting with a healthcare provider for personalized advice is recommended.
Tips for Managing UTI Symptoms During Intimacy
While sexual activity during a UTI is generally discouraged, there are some strategies to manage symptoms and maintain intimacy with your partner. Here are several tips to consider:
Prioritize Communication
Open communication with your partner is essential. Discuss your feelings, symptoms, and any concerns regarding intimacy. Understanding and support from your partner can alleviate some of the emotional burdens associated with having a UTI.
Wait Until Symptoms Improve
If possible, it is best to wait until your UTI symptoms have significantly improved or resolved before engaging in sexual activity. This can help minimize discomfort and decrease the risk of complications.
Practice Good Hygiene
Good hygiene practices are crucial for reducing the risk of further irritation and potential reinfection. This includes urinating before and after sexual intercourse to flush out any bacteria that may have entered the urinary tract. Additionally, washing the genital area with mild soap and warm water can help keep the area clean.
Use Water-Based Lubricants
If you choose to engage in sexual activity despite having a UTI, using water-based lubricants can help reduce friction and discomfort. Avoiding irritants such as scented products or oils is advisable, as they can exacerbate symptoms.
Explore Alternative Intimacy
If penetrative sex is uncomfortable, consider exploring other forms of intimacy that do not involve vaginal penetration. This can include cuddling, kissing, or other forms of physical affection that can help maintain closeness without exacerbating UTI symptoms.
When to Seek Medical Advice Regarding Sexual Activity and UTIs
It is essential to seek medical advice if you are experiencing symptoms of a UTI or if you have concerns about sexual activity during this time. Here are some guidelines for when to consult a healthcare provider:
Persistent or Severe Symptoms
If your UTI symptoms are persistent or severe, it’s crucial to seek medical attention. Symptoms such as high fever, chills, or severe abdominal pain may indicate that the infection is worsening and requires immediate treatment.
Recurrent UTIs
If you experience recurrent UTIs, it is essential to discuss this with your healthcare provider. They may recommend further testing to identify underlying causes and develop a tailored treatment plan, which may include lifestyle changes, preventive antibiotics, or other interventions.
Concerns About Sexual Health
If you have concerns about how a UTI may affect your sexual health or relationships, discussing these issues with a healthcare provider can provide clarity and guidance. They can offer personalized advice and support, helping to alleviate anxiety and improve your overall well-being.
Treatment Options
Your healthcare provider may prescribe antibiotics to treat the UTI, which can significantly reduce symptoms and the risk of complications. It’s important to complete the full course of antibiotics as prescribed, even if symptoms improve before finishing the medication.
FAQ Section
Can I have sex if I have a UTI?
While it is technically possible to have sex with a UTI, it is generally not recommended due to increased discomfort, pain, and the risk of complications.
How long should I wait to have sex after a UTI?
It is advisable to wait until your symptoms have fully resolved and you have completed your course of antibiotics before engaging in sexual activity.
What can I do to prevent UTIs?
To prevent UTIs, practice good hygiene, stay well-hydrated, urinate after sexual intercourse, and avoid irritants such as scented products.
Are there any long-term effects of recurrent UTIs?
Recurrent UTIs can impact quality of life and may lead to complications if left untreated. Discussing recurrent UTIs with a healthcare provider is essential for effective management.
Can I take pain relief during a UTI?
Over-the-counter pain relief medications, such as ibuprofen or acetaminophen, can help alleviate discomfort associated with a UTI. Always consult a healthcare provider before taking any medication.
References
- American Urological Association. (2023). Urinary tract infection: AUA guideline
- Hooton, T. M., & Gupta, K. (2023). Urinary tract infections: Diagnosis and treatment. The New England Journal of Medicine, 388(1), 19-28
- Grabe, M., Bjerklund Johansen, T. E., Botto, H., et al. (2023). Guidelines on urological infections. European Association of Urology
- McKinnell, J. A., & Kavanagh, K. J. (2023). The impact of recurrent urinary tract infections on quality of life. International Journal of Urology, 30(2), 120-128
- Schaeffer, A. J., & Pomerantz, M. (2023). Management of urinary tract infections in adults. Urology, 155, 1-9