Table of Contents
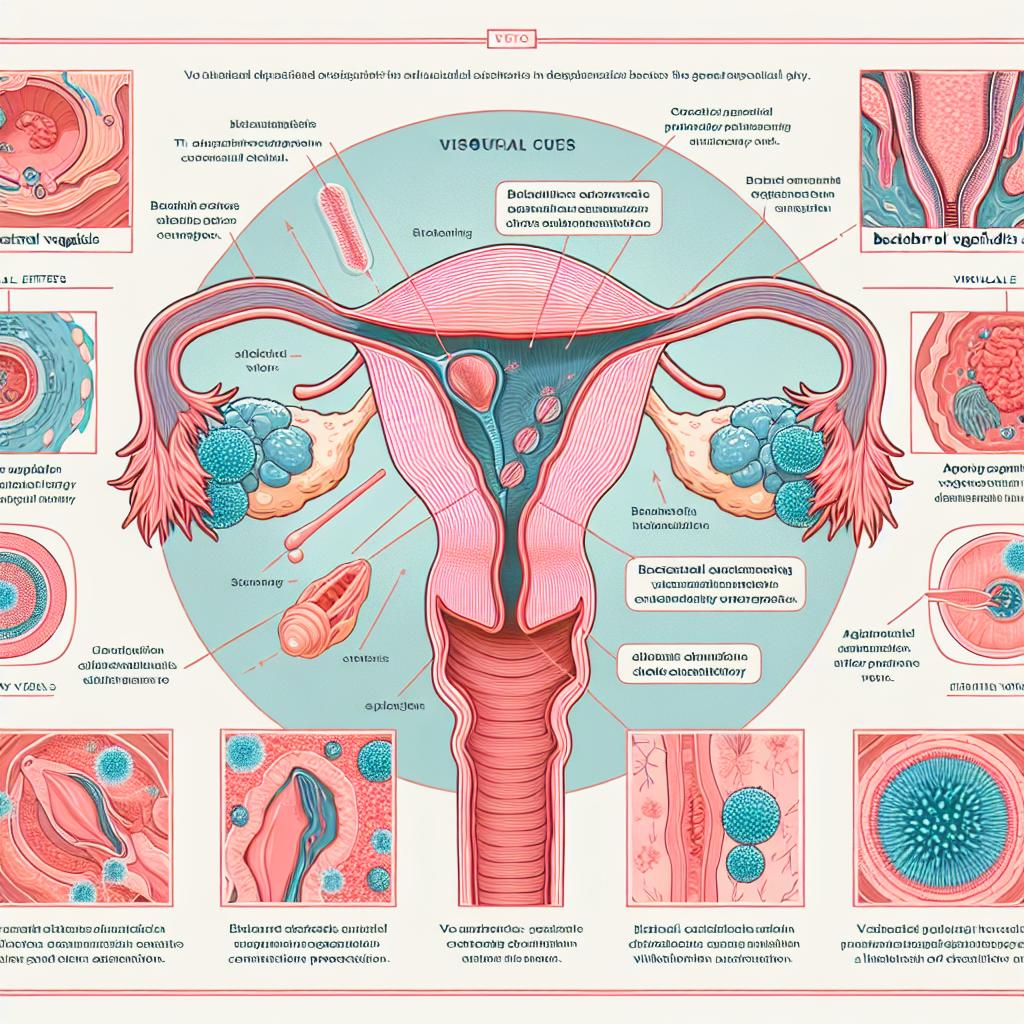
Overview of Yeast Infections and UTIs
Yeast infections, predominantly caused by Candida albicans, are common fungal infections that affect many women, particularly during their reproductive years. These infections can cause significant discomfort, presenting symptoms such as itching, burning, and unusual discharge. On the other hand, urinary tract infections (UTIs) are typically caused by bacteria, with a notable prevalence of Escherichia coli in these infections. UTIs can lead to serious complications if left untreated, including kidney infections and sepsis.
The connection between yeast infections and UTIs has been a point of discussion among healthcare providers. While they are distinct conditions, some studies suggest that the presence of a yeast infection may predispose individuals to UTIs. This can occur due to the alterations in the vaginal microbiome, which can affect the urogenital tract’s susceptibility to infections.
Connection Between Yeast Infections and UTIs
Research indicates that women with recurrent yeast infections may also experience an increased incidence of UTIs. This relationship may partially stem from overlapping risk factors, such as hormonal changes, antibiotic use, and poor hygiene practices. For example, antibiotic treatments for bacterial infections can disrupt the normal vaginal flora, allowing for yeast overgrowth. When the balance of the microbiome is altered, it might facilitate the growth of pathogenic bacteria, potentially leading to UTIs.
Furthermore, the physiological changes caused by a yeast infection, such as increased inflammation and changes in vaginal pH, may also contribute to an increased risk of UTIs. Studies have shown that women with diagnosed yeast infections have a higher likelihood of subsequently developing UTIs, indicating a possible link between the two conditions (Nachum et al., 2025).
Table 1: Common Symptoms of Yeast Infections and UTIs
| Symptom | Yeast Infection | Urinary Tract Infection |
|---|---|---|
| Itching | Yes | No |
| Burning sensation | Yes | Yes |
| Unusual discharge | Yes | No |
| Frequent urination | No | Yes |
| Cloudy or foul-smelling urine | No | Yes |
| Pain during intercourse | Yes | No |
| Lower abdominal pain | No | Yes |
Symptoms and Diagnosis of Yeast Infections and UTIs
Both yeast infections and UTIs present with overlapping symptoms, making diagnosis challenging without proper examination. Common symptoms of yeast infections include:
- Intense itching and irritation in the vaginal area
- Thick, white, odorless discharge resembling cottage cheese
- Redness and swelling of the vulva
- Pain during intercourse or urination
For UTIs, symptoms typically manifest as:
- A strong, persistent urge to urinate
- Burning sensation during urination
- Frequent urination, often in small amounts
- Cloudy or strong-smelling urine
- Pelvic pain in women
Diagnosis for yeast infections is primarily conducted through a pelvic examination and laboratory tests, such as a wet mount or culture to identify fungal elements. For UTIs, a urinalysis is performed, often followed by a urine culture to pinpoint the specific bacteria causing the infection.
Table 2: Diagnostic Methods
| Condition | Diagnostic Method |
|---|---|
| Yeast Infection | Pelvic examination, wet mount, culture |
| Urinary Tract Infection | Urinalysis, urine culture |
Treatment Options for Yeast Infections and UTIs
The treatment for yeast infections typically involves antifungal medications, which can be administered orally or topically. Common antifungal treatments include fluconazole and clotrimazole. It’s essential for individuals experiencing recurrent yeast infections to consult with a healthcare provider to rule out underlying conditions that might contribute to the problem.
For UTIs, treatment usually consists of antibiotics, with common choices including nitrofurantoin and trimethoprim-sulfamethoxazole. In cases of complicated UTIs or those caused by resistant strains, alternative antibiotics may be necessary.
Table 3: Treatment Options
| Condition | First-line Treatment |
|---|---|
| Yeast Infection | Oral fluconazole or topical clotrimazole |
| Urinary Tract Infection | Nitrofurantoin or trimethoprim-sulfamethoxazole |
Prevention Strategies for Yeast Infections and UTIs
Preventing yeast infections and UTIs involves similar strategies centered around maintaining a healthy vaginal microbiome and urinary tract health. Here are some effective prevention strategies:
-
Maintain Proper Hygiene: Regular bathing and proper wiping techniques after using the toilet can reduce microbial load and prevent infections.
-
Wear Breathable Clothing: Cotton underwear and loose-fitting clothing can help maintain a balanced vaginal environment.
-
Limit Antibiotic Use: Avoid unnecessary antibiotic treatments to prevent disruption of the normal flora, which can lead to yeast overgrowth.
-
Probiotics: Some studies suggest that oral probiotics may help restore the natural balance of bacteria in the vaginal microbiome, potentially preventing recurrent infections (Nachum et al., 2025).
-
Stay Hydrated: Drinking plenty of water can help flush out bacteria from the urinary tract, reducing the risk of UTIs.
-
Urinate After Intercourse: This practice can help eliminate bacteria that may have entered the urethra during sexual activity.
Table 4: Prevention Strategies
| Prevention Strategy | Yeast Infection | Urinary Tract Infection |
|---|---|---|
| Maintain proper hygiene | Yes | Yes |
| Wear breathable clothing | Yes | Yes |
| Limit antibiotic use | Yes | Yes |
| Use probiotics | Yes | Potentially |
| Stay hydrated | No | Yes |
| Urinate after intercourse | No | Yes |
FAQ
Can yeast infections cause UTIs?
While yeast infections do not directly cause UTIs, the conditions that lead to a yeast infection can also increase the risk of developing a UTI due to overlapping risk factors.
How can I prevent recurrent yeast infections?
Practices such as maintaining proper hygiene, wearing breathable underwear, and possibly taking probiotics can help prevent recurrent yeast infections.
Are there any dietary changes that can help prevent UTIs?
Drinking plenty of water and cranberry juice may help prevent UTIs by flushing bacteria out of the urinary tract.
How long does treatment for a yeast infection or UTI typically last?
Treatment for a yeast infection typically lasts 1 to 7 days, depending on the medication used, while antibiotic treatment for UTIs usually lasts from 3 to 7 days, depending on the severity and type of bacteri
When should I see a doctor for a yeast infection or UTI?
If you experience severe symptoms, frequent recurrences, or if you are pregnant, you should consult a healthcare provider for appropriate diagnosis and treatment.
References
- Nachum, Z., Suleiman, A., Colodner, R., Battino, S., Wattad, M., Kuzmin, O., & Yefet, E. (2025). Oral Probiotics to Prevent Recurrent Vulvovaginal Infections During Pregnancy—Multicenter Double-Blind, Randomized, Placebo-Controlled Trial. Nutrients, 17(3), 460. https://doi.org/10.3390/nu17030460
- Khan, S., Cai, L., Bilal, H., Khan, M. N., Fang, W., Zhang, D., … & Zeng, Y. (2025). An 11-Year retrospective analysis of candidiasis epidemiology, risk factors, and antifungal susceptibility in a tertiary care hospital in China. Scientific Reports, 14(1), 92100. https://doi.org/10.1038/s41598-025-92100-x
- Araújo, S., Silva, V., Quintelas, M., Martins, Â., Igrejas, G., & Poeta, P. (2025). From soil to surface water: exploring Klebsiella’s clonal lineages and antibiotic resistance odyssey in environmental health. BMC Microbiology, 25(1), 379. https://doi.org/10.1186/s12866-025-03798-8