Table of Contents
Overview of Urinary Tract Infections and Proteinuria
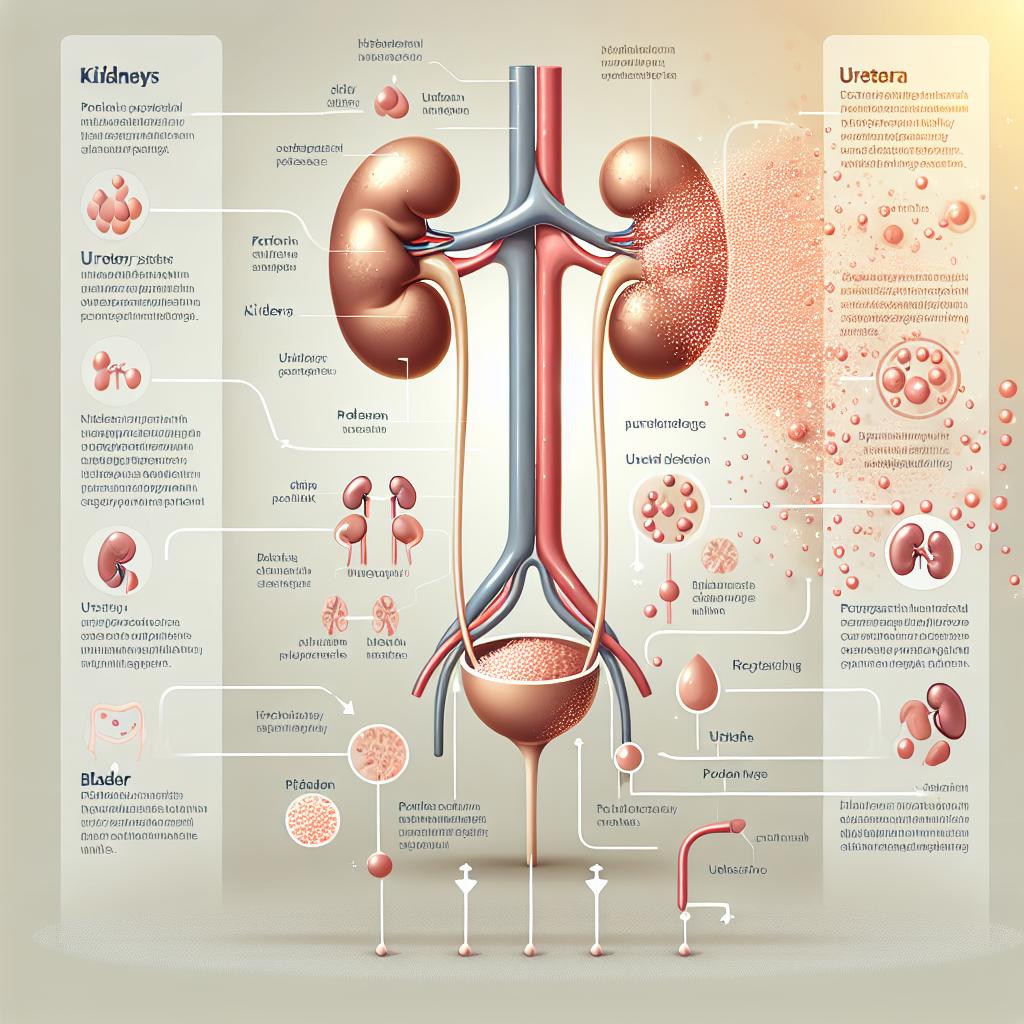
Urinary Tract Infections (UTIs) are among the most common infections encountered in the clinical setting, particularly among women. They occur when bacteria enter the urinary tract, leading to inflammation and infection. UTIs can manifest in various forms, including cystitis (bladder infection) and pyelonephritis (kidney infection). An important aspect of UTIs that has garnered attention is their potential association with proteinuria, which is the presence of excess proteins in urine. This condition can be indicative of various underlying disease processes, including kidney dysfunction.
The kidneys play a crucial role in filtering waste and excess substances from the blood, including proteins. When kidneys are damaged or inflamed—conditions that can occur due to severe UTIs—they may allow proteins to leak into the urine. This can lead to a state known as proteinuria. Understanding the connection between UTIs and proteinuria is essential, as it can provide insights into the severity of the infection and potential complications arising from it.
Table 1: Common Causes of Proteinuria
| Cause | Description |
|---|---|
| Urinary Tract Infection (UTI) | Infection leading to inflammation and damage to kidney filtration. |
| Diabetes Mellitus | Can cause damage to nephron structures, allowing protein leakage. |
| Hypertension | High blood pressure can lead to kidney damage over time. |
| Kidney Diseases | Glomerulonephritis and nephrotic syndrome can result in significant proteinuria. |
| Medications | Certain drugs may cause kidney damage, leading to protein leakage. |
How UTIs Lead to Protein Presence in Urine
UTIs can lead to proteinuria primarily through the inflammatory response they elicit in the urinary tract. When bacteria invade the urinary tract, the immune system responds by sending white blood cells to the site of infection. This immune response can cause damage to the cells in the kidneys and bladder, which in turn affects their filtering capabilities. The inflammation may disrupt the normal barrier function of the glomeruli, the filtering units in the kidneys, resulting in protein leakage into the urine.
Additionally, the type of bacteria causing the UTI can also influence the severity of the kidney damage. For instance, uropathogenic Escherichia coli (UPEC) is known to cause more severe kidney damage than other strains. A study found that the inflammatory markers associated with UTI, such as leukocyte counts and C-reactive protein (CRP) levels, correlate with the degree of proteinuria observed in patients (Pathi et al., 2025).
Key Insights:
- Inflammation and Damage: The inflammatory response to UTIs can lead to damage in the kidney filtering mechanism, allowing proteins to escape into the urine.
- Bacterial Virulence: The virulence of the bacteria involved in the UTI can play a role in the extent of kidney damage and the consequent proteinuria observed.
Symptoms Indicating UTI and Proteinuria Connection
Patients suffering from UTIs often present with a range of symptoms, including:
- Dysuria: Painful urination is a common symptom indicating irritation of the urinary tract.
- Increased Urinary Frequency: Patients may feel the need to urinate more often, even if small amounts of urine are produced.
- Hematuria: Blood in the urine can occur due to inflammation or damage to the urinary tract.
- Proteinuria: The presence of proteins in the urine can often be detected through urinalysis.
Furthermore, patients may exhibit systemic symptoms such as fever, chills, and malaise, especially in cases of pyelonephritis. Recognizing these symptoms is vital for timely diagnosis and treatment to avoid complications such as chronic kidney disease.
Table 2: Symptoms of UTI
| Symptom | Description |
|---|---|
| Dysuria | Painful urination |
| Increased Urinary Frequency | Frequent urge to urinate despite low urine volume |
| Hematuria | Blood in urine |
| Fever | Elevated body temperature indicating infection |
| Proteinuria | Presence of protein in urine detected via urinalysis |
Diagnostic Approaches for UTIs and Protein in Urine
Diagnosing a UTI involves several steps, with urinalysis being the cornerstone of diagnosis. Urinalysis can reveal the presence of leukocytes, nitrites, and proteins, providing a preliminary indication of a urinary tract infection. For definitive diagnosis, urine culture is conducted to identify the specific bacteria causing the infection and to determine their antibiotic sensitivity patterns.
- Urinalysis: A dipstick test can quickly indicate the presence of protein, glucose, ketones, and other substances. Microscopic examination may also reveal the presence of red and white blood cells.
- Urine Culture: This test determines the specific bacteria present in the urine and assesses their sensitivity to various antibiotics. A culture showing more than 100,000 CFUs/mL typically indicates a significant infection.
- Blood Tests: Blood tests may be conducted to assess kidney function (BUN and creatinine levels) and to check for signs of systemic infection.
Table 3: Diagnostic Tests for UTI
| Test | Purpose |
|---|---|
| Urinalysis | Initial screening for infection and kidney function |
| Urine Culture | Identify specific pathogens and antibiotic sensitivity |
| Blood Tests | Assess overall kidney function and systemic infection |
Treatment Options for UTIs and Managing Protein Levels
Treatment of UTIs typically involves the use of antibiotics, with the choice of antibiotic guided by culture results. Commonly prescribed antibiotics include:
- Nitrofurantoin: Effective for uncomplicated Utis.
- Trimethoprim-sulfamethoxazole: Often used for its broad-spectrum effectiveness.
- Ciprofloxacin: A fluoroquinolone used in cases where other antibiotics are ineffective.
In addition to antibiotics, management of proteinuria involves addressing the underlying cause. For instance, if the proteinuria is due to a UTI, effective treatment of the infection may resolve the proteinuria. However, if the protein levels remain elevated after treatment, further evaluation for chronic kidney disease or other underlying renal issues may be necessary.
Key Treatment Insights:
- Antibiotic Therapy: Early initiation of appropriate antibiotics is crucial for effective management of UTIs.
- Monitoring Protein Levels: Regular urinalysis post-treatment is necessary to monitor for resolution of proteinuria and to assess kidney function.
Table 4: Common Antibiotics for UTI Treatment
| Antibiotic | Spectrum of Activity |
|---|---|
| Nitrofurantoin | Effective against E. coli and other common uropathogens |
| Trimethoprim-sulfamethoxazole | Broad-spectrum activity against many bacteria |
| Ciprofloxacin | Effective against a wide range of gram-negative bacteria |
FAQ Section
Can a UTI cause long-term kidney damage?
Yes, if left untreated, a UTI can lead to complications such as pyelonephritis, which may result in kidney damage over time.
How is proteinuria diagnosed?
Proteinuria is typically diagnosed through urinalysis, which may show elevated protein levels in the urine. Further tests may be conducted to determine the underlying cause.
What are the risk factors for developing a UTI?
Risk factors include being female, sexual activity, certain contraceptive methods, a weakened immune system, and pre-existing urinary tract abnormalities.
What should I do if I suspect a UTI?
If you suspect a UTI, it is important to consult a healthcare provider for an accurate diagnosis and appropriate treatment.
Can diet affect UTI occurrence?
Yes, dietary habits can influence UTI risk. Staying well-hydrated and consuming a diet rich in fruits and vegetables may help reduce the risk.
References
-
Pathi, B. K., Mohapatra, S., Sharma, V., Mohapatra, I., & Panigrahi, K. (2025). Antimicrobial Sensitivity Patterns of Bacteria Causing Urinary Tract Infections: A Retrospective Study of Elderly Patients Admitted to a Tertiary Care Hospital in Bhubaneswar, India. Cureus. Retrieved from https://doi.org/10.7759/cureus.77399
-
Senda, J. C. N. M., & Phillippi, J. C. (2024). Acute Cystitis in a Transfeminine Patient: Assessment and Treatment of Urinary Tract Symptoms. Journal of Midwifery & Women’s Health
-
Khodaparast, L., et al. (2025). Co-translational protein aggregation and ribosome stalling as a broad-spectrum antibacterial mechanism. Nature Communications. Retrieved from https://doi.org/10.1038/s41467-025-56873-z
-
Popova, E., Tkachev, S., & Shapoval, A. (2025). Kidney Stones as Minerals: How Methods from Geology Could Inform Urolithiasis Treatment. Journal of Clinical Medicine. Retrieved from https://doi.org/10.3390/jcm14030997
-
2025 iCatCare consensus guidelines on the diagnosis and management of lower urinary tract diseases in cats