Table of Contents
Introduction to Urinary Tract Infections and Bleeding
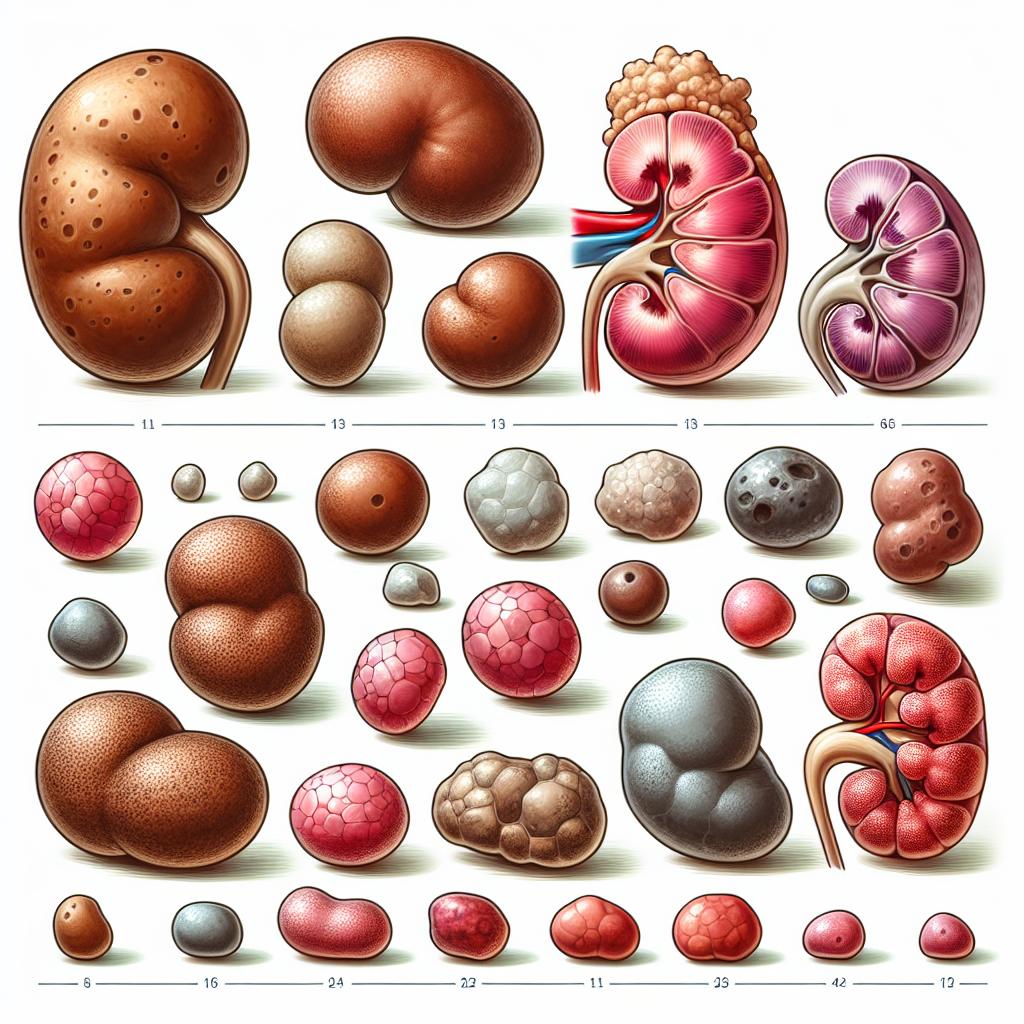
Urinary tract infections (UTIs) are among the most prevalent infections encountered in clinical practice, affecting millions worldwide annually. While UTIs are commonly characterized by symptoms such as dysuria, urgency, and frequency, they can also lead to more concerning manifestations, including bleeding. This article explores the relationship between UTIs and bleeding, examining the symptoms, mechanisms, risk factors, and treatment options associated with this condition.
Bleeding associated with UTIs can range from microscopic hematuria, detected only on urinalysis, to gross hematuria, where blood is visibly present in urine. Understanding the underlying causes of bleeding in UTI patients is crucial for effective diagnosis and management, as it can indicate complications or coexisting conditions that may require urgent intervention.
Symptoms of UTI: When to Expect Bleeding
The classic symptoms of a UTI include:
- Dysuria: Painful or burning sensation during urination.
- Increased Frequency: The urge to urinate more often than usual.
- Urgency: A sudden, strong need to urinate.
- Nocturia: Frequent urination during the night.
- Suprapubic Pain: Discomfort or pain in the lower abdomen.
In some instances, patients may experience hematuria, which is the presence of blood in urine. Bleeding can occur due to irritation of the urinary tract lining, inflammatory responses, or more severe conditions such as urinary calculi or bladder cancer. It is essential for patients to report any occurrence of hematuria promptly, as it may indicate a more serious underlying condition, such as a urinary tract obstruction or malignancy.
Table 1: Symptoms of UTI
| Symptom | Description |
|---|---|
| Dysuria | Painful urination |
| Increased Frequency | Need to urinate more often |
| Urgency | Sudden, strong need to urinate |
| Nocturia | Frequent urination at night |
| Suprapubic Pain | Discomfort in the lower abdomen |
| Hematuria | Presence of blood in urine (microscopic or gross) |
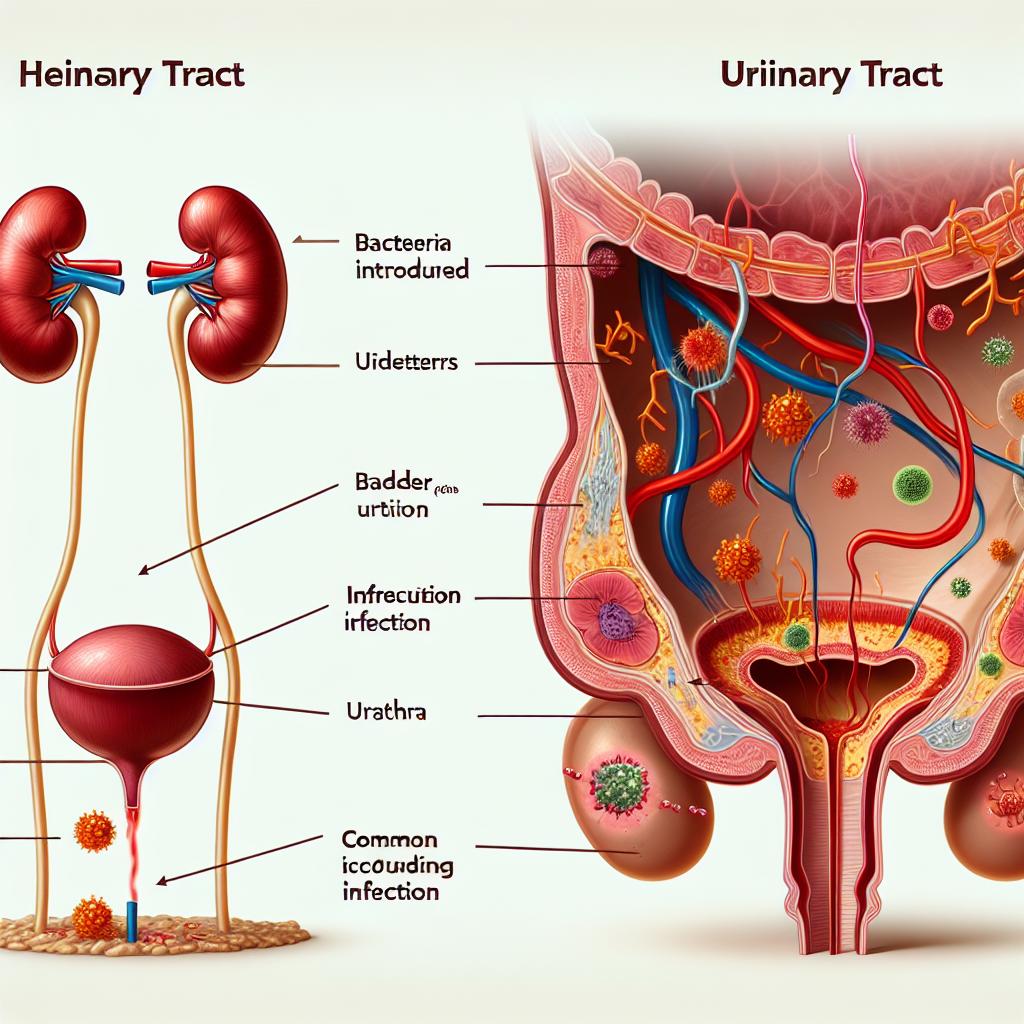
The Mechanism: How UTIs Can Lead to Bleeding
Bleeding in the context of UTIs can arise from several mechanisms:
- Mucosal Irritation: The inflammatory response due to infection can lead to irritation and damage to the mucosal lining of the bladder and urethra, resulting in bleeding.
- Infection Severity: Severe UTIs can progress to pyelonephritis, where the kidneys become involved. This condition can lead to increased intrarenal pressure, resulting in bleeding.
- Presence of Stones: The formation of urinary calculi can cause mechanical irritation of the urinary tract, leading to bleeding.
- Underlying Conditions: Conditions such as bladder cancer or severe clotting disorders can cause bleeding that may initially be attributed to a UTI.
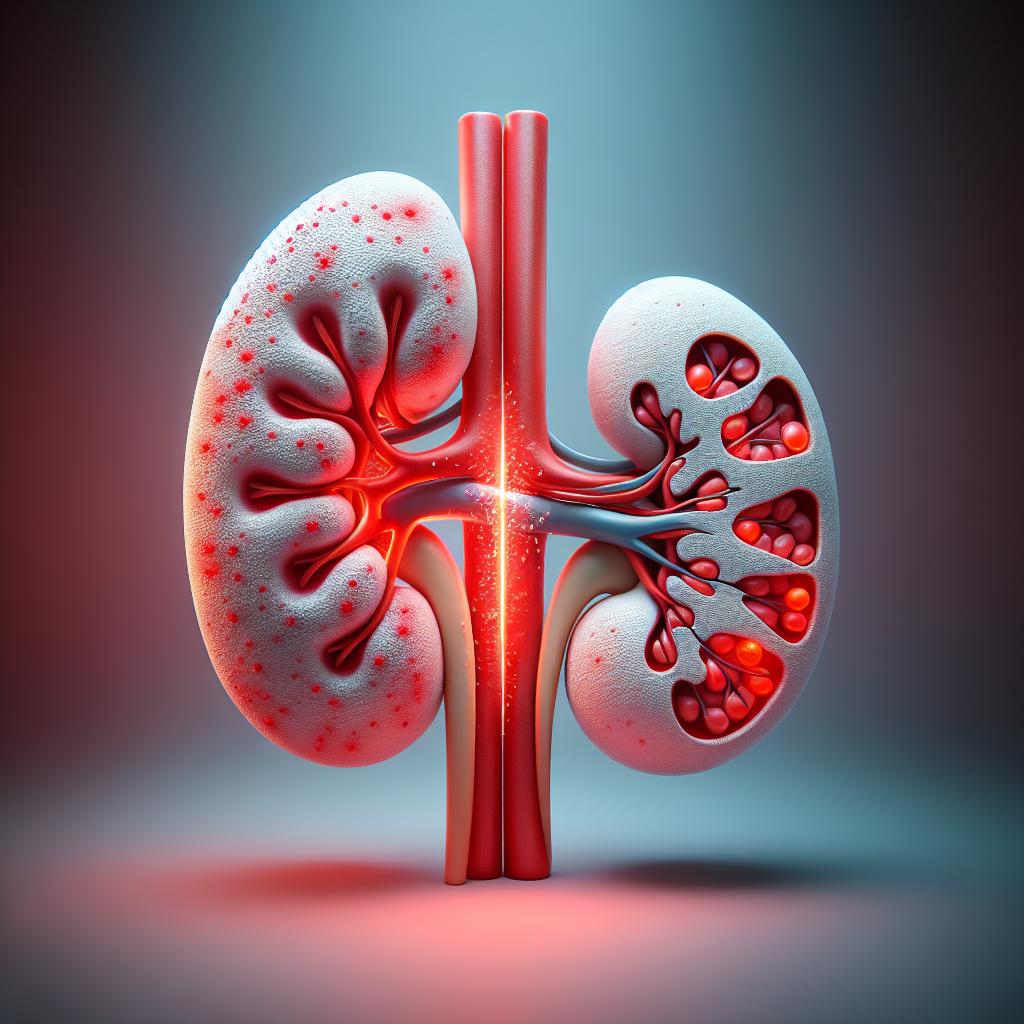
Figure 1: Mechanisms of UTI-Induced Bleeding
- Mucosal Damage: Caused by inflammation and infection.
- Severe Infection: Progression to pyelonephritis.
- Stones: Mechanical irritation leading to bleeding.
- Underlying Pathology: Malignancies or clotting disorders.
Risk Factors for Bleeding in UTI Patients
Certain risk factors can increase the likelihood of experiencing bleeding associated with UTIs:
- Age: Older adults are more susceptible to UTIs and may experience complications, including bleeding.
- Gender: Women are more prone to UTIs due to anatomical differences, and they may experience bleeding due to hormonal changes affecting the urinary tract.
- History of UTIs: Recurrent Utis may lead to chronic inflammation and increase bleeding risk.
- Immunocompromised States: Individuals with weakened immune systems may have a higher risk of severe infections, leading to complications like bleeding.
- Urinary Tract Abnormalities: Structural abnormalities in the urinary tract can predispose individuals to UTIs and bleeding.
Table 2: Risk Factors for UTI-Related Bleeding
| Risk Factor | Description |
|---|---|
| Age | Older adults may experience complications |
| Gender | Women are at higher risk due to anatomy |
| History of UTIs | Recurrent infections can lead to increased risk |
| Immunocompromised | Weakened immune systems increase infection severity |
| Structural Abnormalities | Physical irregularities in the urinary tract |
Treatment Options for UTI-Related Bleeding and Prevention
Management of UTIs and associated bleeding involves several strategies:
- Antibiotic Therapy: The cornerstone of UTI treatment is the use of appropriate antibiotics to eradicate the infection. This also helps to reduce inflammation and associated bleeding.
- Hydration: Increasing fluid intake can help flush out bacteria and irritants from the urinary tract, potentially reducing bleeding.
- Pain Management: Nonsteroidal anti-inflammatory drugs (NSAIDs) may be used to alleviate discomfort associated with UTIs.
- Surgical Intervention: In cases where bleeding is due to stones or tumors, surgical intervention may be required to address the underlying cause.
- Preventive Measures: Educating patients on proper hygiene, adequate hydration, and avoiding irritants such as caffeine and alcohol can help reduce the risk of recurrent UTIs.
Figure 2: Treatment Options for UTI-Related Bleeding
- Antibiotics: Targeted antibiotic therapy.
- Hydration: Increase fluid intake.
- Pain Management: Use of NSAIDs.
- Surgery: Intervention for stones or tumors.
- Prevention: Hygiene and lifestyle modifications.
Frequently Asked Questions (FAQs)
Can a UTI cause bleeding in urine?
Yes, a UTI can cause bleeding in urine due to irritation and inflammation of the urinary tract lining.
What should I do if I notice blood in my urine?
If you notice blood in your urine, it is essential to seek medical attention promptly, as it may indicate a serious underlying condition.
Are there specific risk factors for bleeding with a UTI?
Yes, risk factors include age, gender, history of UTIs, immunocompromised status, and urinary tract abnormalities.
How are UTIs treated to prevent bleeding?
UTIs are treated with antibiotics, hydration, and pain management. Preventive measures include good hygiene and lifestyle changes.
What complications can arise from a UTI if left untreated?
Untreated UTIs can lead to severe complications such as pyelonephritis, kidney damage, and in some cases, systemic infections.
References
- How to Diagnose and Manage Urinary Tract Infections in Adults. Retrieved from https://doi.org/10.56305/001c.122941
- Comparison of Urinary Tract Infection Rates Between Transperineal Prostate Biopsies with and Without Prophylactic Antibiotics: An Updated Systematic Review and Meta-Analysis. Retrieved from https://doi.org/10.3390/medicina61020198
- Understanding oncologic emergencies and related emergency department visits and hospitalizations: a systematic review. Retrieved from https://doi.org/10.1186/s12873-025-01183-2
- Solid Organ Transplants Caused by COVID-19 Infection and the Outcome of Transplantation Post-COVID-19: A Systematic Review. Retrieved from https://doi.org/10.3390/biomedicines13020428
- A rare case of female urinary retention caused by urethral leiomyoma: A case report. Retrieved from https://doi.org/10.1016/j.ijscr.2025.110849
- Hemorrhagic adenovirus cystitis in a newborn. Retrieved from https://doi.org/10.1515/crpm-2022-0018
- Low Rates of 30-Day Postoperative Complications After Meniscal Allograft Transplantation: A Retrospective Study Using the National Surgical Quality Improvement Program Database. Retrieved from https://doi.org/10.1016/j.asmr.2024.101015
- The utility of flexible and navigable suction access sheath (FANS) in patients undergoing same session flexible ureteroscopy for bilateral renal calculi: a global prospective multicenter analysis by EAU endourology. Retrieved from https://doi.org/10.1007/s00345-025-05477-9