Table of Contents
Causes of Urinary Tract Infections in Women
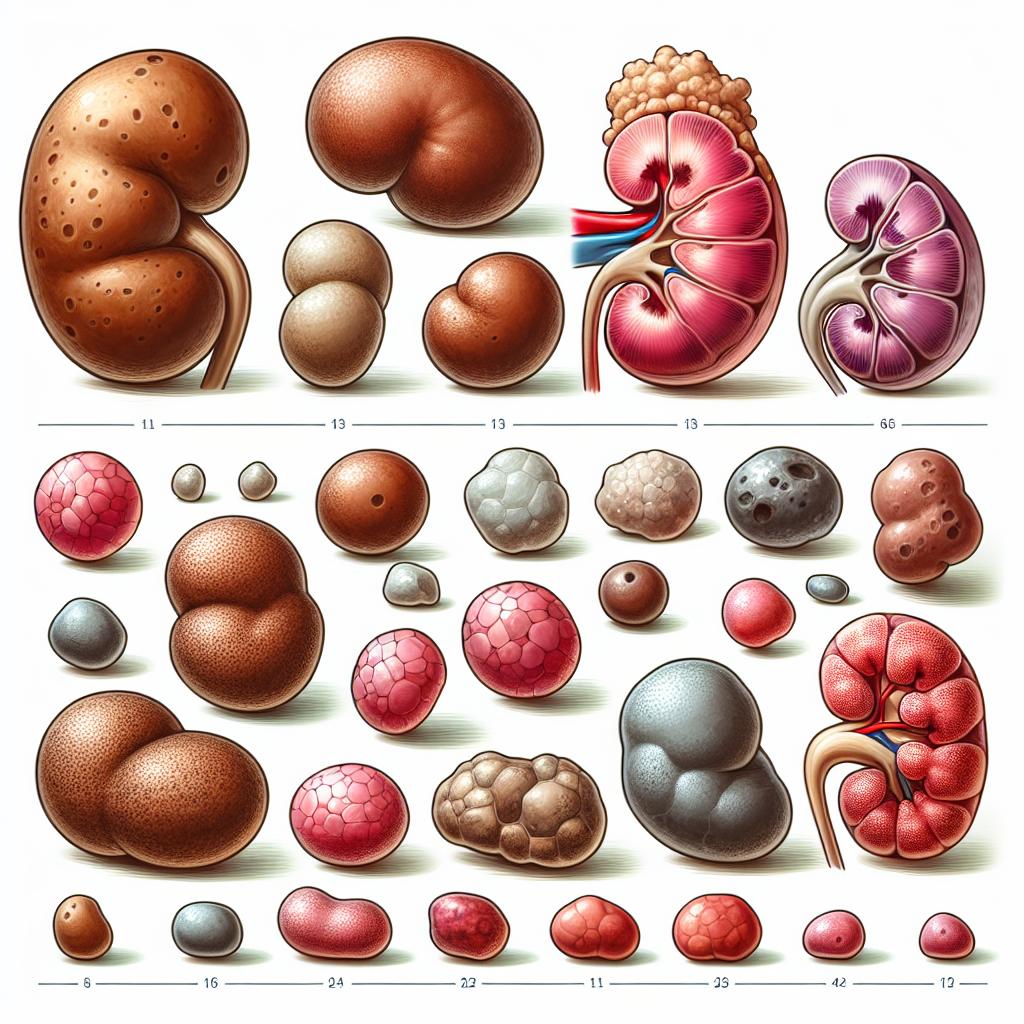
UTIs are primarily caused by bacteria, with Escherichia coli being the most common pathogen. However, factors contributing to the onset of UTIs can be multifaceted. The primary causes include:
-
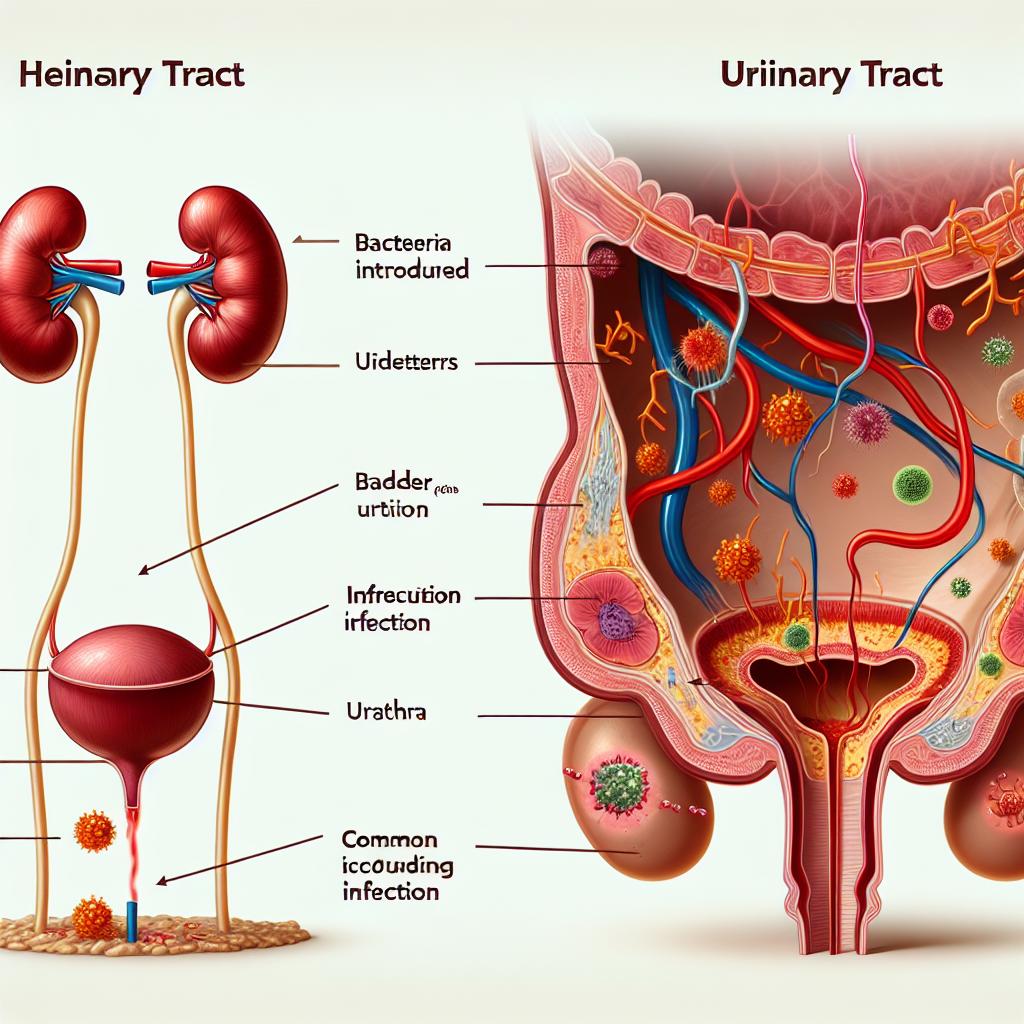
Bacterial Introduction: Sexual intercourse can introduce bacteria from the genital area into the urethra, leading to infection. Studies indicate that nearly 80-90% of UTIs in women are due to E. coli, which can travel from the anus to the urethra during sexual activity (Azra et al., 2025).
-
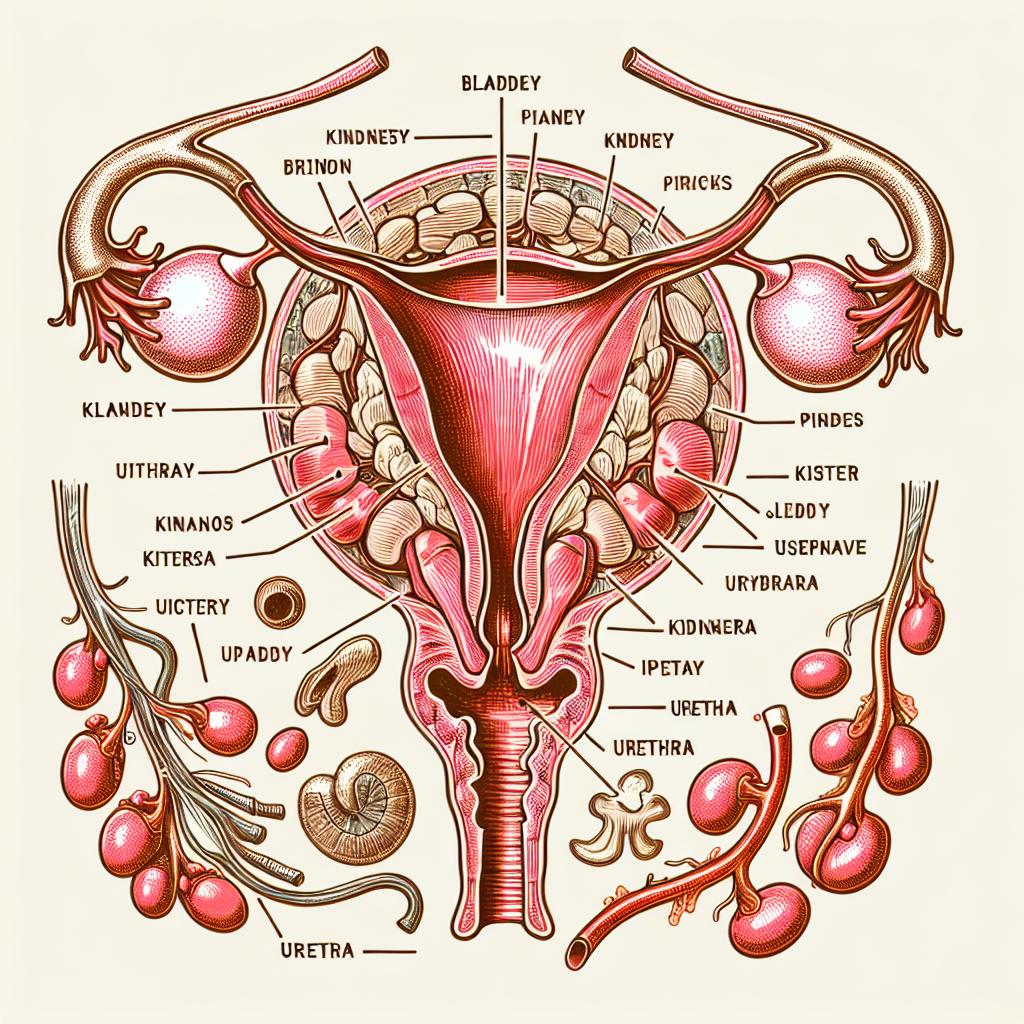
Anatomical Factors: Women have shorter urethras than men, making it easier for bacteria to reach the bladder. The proximity of the urethra to the vaginal opening and anus increases the likelihood of bacterial contamination (Cuccu et al., 2024).
-
Hormonal Changes: Hormonal fluctuations during menstrual cycles or menopause can alter the vaginal flora, making women more susceptible to infections (Gullo et al., 2024).
-
Hygiene Practices: Poor hygiene can play a significant role in UTI development. Women are often advised to wipe from front to back and urinate after intercourse to help flush out bacteria (Griesser et al., 2022).
-
Contraceptive Methods: Certain contraceptive methods, particularly diaphragms or spermicides, can increase the risk of UTIs by altering vaginal flora or blocking the urethra’s opening.
The Role of Sperm in Urinary Tract Health
While the primary concern with sperm is its role in reproduction, there are implications for urinary tract health. Sperm itself does not directly cause UTIs; however, its interaction with the female body during intercourse can affect the vaginal environment and bacterial flora.
Research suggests that certain proteins in semen may alter the vaginal microbiome, potentially leading to an imbalance favorable for bacterial growth (Cuccu et al., 2024). Additionally, the presence of sperm in the urinary tract post-intercourse can create an environment that allows bacteria to thrive.
Table 1: Factors Influencing UTI Risk Related to Sperm
| Factor | Effect on UTI Risk |
|---|---|
| Semen Composition | May alter vaginal flora |
| Timing of Intercourse | Urination post-intercourse can reduce risk |
| Contraceptive Methods | Some methods may increase susceptibility |
| Hygiene Practices | Proper hygiene can mitigate risk |
Understanding the Transmission of Infections Through Sperm
The transmission of infections through sperm is not as straightforward as it may seem. While sperm itself is not a vehicle for UTIs, the act of sexual intercourse can lead to the introduction of bacteria into the urinary tract.
Bacterial Transmission Mechanisms
-
Physical Transfer: During intercourse, bacteria from the genital area can be physically transferred to the urethra. If the male partner carries bacteria in his urethra or on his skin, these can be introduced into the female’s urinary tract (Azra et al., 2025).
-
Semen’s Biochemical Environment: The biochemical properties of semen, including pH and osmolarity, may create a conducive environment for certain bacteria to thrive once they are introduced into the urinary tract.
Preventive Measures Against UTIs Related to Sexual Activity
Preventing UTIs, especially those potentially linked to sexual activity, involves several proactive measures:
-
Hydration: Drinking plenty of water can help flush bacteria from the urinary tract, reducing the risk of infection (Cuccu et al., 2024).
-
Post-Intercourse Urination: Women are encouraged to urinate shortly after sexual intercourse to help expel any bacteria that may have entered the urethra (Gullo et al., 2024).
-
Proper Hygiene: Maintaining good genital hygiene is crucial. This includes washing the genitalia before and after intercourse and avoiding irritants like harsh soaps or douches (Griesser et al., 2022).
-
Choice of Contraceptives: Choosing non-spermicidal forms of contraception may reduce the risk of UTIs. Diaphragms and spermicides are known to increase susceptibility (Cuccu et al., 2024).
-
Regular Medical Check-ups: Women with recurrent Utis should consult healthcare providers for potential underlying issues and personalized advice on prevention.
Impact of Sexual Practices on UTI Risks in Women
Sexual practices can significantly influence the risk of developing UTIs. Understanding these practices can help in implementing effective preventive strategies.
Factors to Consider
-
Frequency of Intercourse: More frequent sexual activity can increase exposure to potential bacterial transfer.
-
Types of Sexual Practices: Certain sexual practices, such as anal intercourse, can increase the risk of bacterial transfer from the anus to the vagina or urethra, necessitating more stringent hygiene practices afterward (Azra et al., 2025).
-
Partner Health: The health status of sexual partners can also impact UTI risk. Partners with urinary tract infections or asymptomatic bacterial colonization can contribute to the risk (Gullo et al., 2024).
Table 2: Sexual Practices and UTI Risk
| Sexual Practice | Effect on UTI Risk |
|---|---|
| Vaginal Intercourse | Moderate risk without precautions |
| Anal Intercourse | High risk if hygiene is inadequate |
| Frequency of Intercourse | Increased risk with higher frequency |
| Use of Spermicides | Increased risk |
FAQ
Can male sperm directly cause UTIs in females?
No, male sperm itself does not directly cause UTIs; however, the act of sexual intercourse can introduce bacteria into the urinary tract, leading to infections.
What measures can women take to reduce UTI risk after sex?
Women can urinate after intercourse, stay hydrated, maintain good hygiene practices, and consider their contraceptive choices to reduce UTI risk.
Are there specific sexual practices that increase UTI risk?
Yes, practices such as anal intercourse can increase UTI risk due to the potential transfer of bacteria from the anus to the vaginal area if proper hygiene is not maintained.
What is the role of hydration in preventing UTIs?
Staying hydrated helps flush out bacteria from the urinary tract, lowering the likelihood of infection.
References
-
Azra, A., Khan, T. A., Ull Haq, I., Hinthong, W., Campino, S. (2025). Antibiotic Susceptibility Patterns and Virulence Profiles of Classical and Hypervirulent Klebsiella pneumoniae Strains Isolated from Clinical Samples in Khyber Pakhtunkhwa, Pakistan. Retrieved from https://doi.org/10.3390/pathogens14010079
-
Cuccu, I., Golia D’Augè, T., Firulli, I., De Angelis, E., Buzzaccarini, G., D’Oria, O., Besharat, A. R., Caserta, D., Bogani, G. (2024). Update on Genitourinary Syndrome of Menopause: A Scoping Review of a Tailored Treatment-Based Approach. Retrieved from https://doi.org/10.3390/life14111504
-
Gullo, G., Etrusco, A., Cucinella, G., Basile, G., Fabio, M., Perino, A., De Tommasi, O., Buzzaccarini, G., Morreale, C. (2024). Hormonal management of menopausal symptoms in women with a history of gynecologic malignancy. Menopause
-
Griesser, H., Skonietzki, S., Fischer, T., Fielder, K., Suesskind, M. (2022). Vaginal moisturizers and lubricants. Clinical Obstetrics and Gynecology, 61(5), 508-516