Table of Contents
Overview of Antibiotics and Their Role in Infections
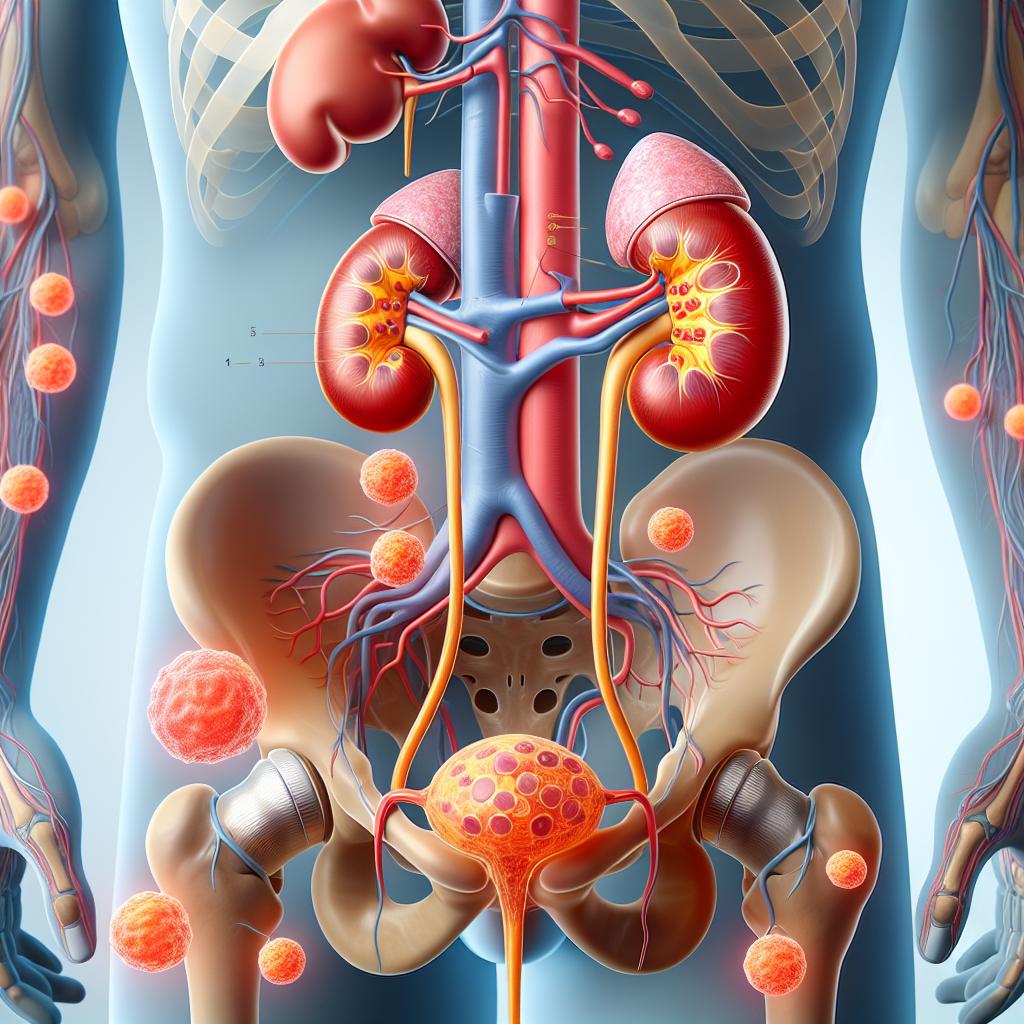
Antibiotics are crucial in the treatment of various bacterial infections, including urinary tract infections (UTIs), which are among the most common bacterial infections globally. An estimated 400 million UTIs occur annually, leading to over 200,000 related deaths. Women are disproportionately affected, with up to 60% experiencing at least one UTI in their lifetime. The most common causative agent of UTIs is Escherichia coli, accounting for approximately 65% to 75% of cases (Pathi et al., 2025) [7].
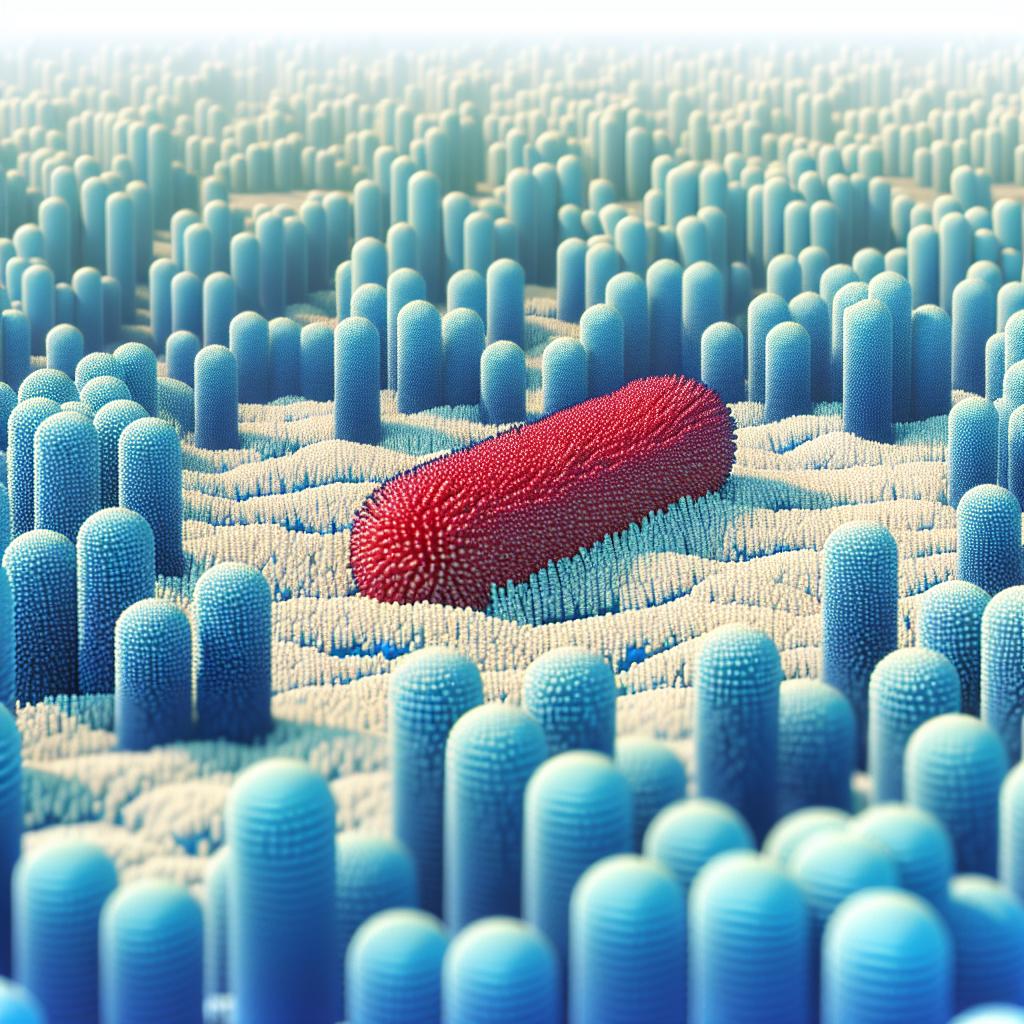
The use of antibiotics has been pivotal in managing infections, but the misuse and overuse have led to increased antimicrobial resistance (AMR), complicating treatment options. Inappropriate use of antibiotics can lead to adverse effects, including disruption of the normal microbiota, making patients more susceptible to infections, including UTIs. A significant concern is that antibiotics can alter the urinary microbiome, potentially increasing the risk of UTI development.
Mechanisms by Which Antibiotics May Lead to UTIs
Antibiotics can inadvertently contribute to the development of UTIs through several mechanisms:
-
Disruption of Normal Flora: Antibiotics kill both pathogenic and beneficial bacteria, disrupting the natural balance of the urinary microbiome. This can allow opportunistic pathogens to proliferate, leading to infections.
-
Selection for Resistant Strains: The use of antibiotics can select for resistant strains of bacteria, making infections harder to treat. For instance, extended-spectrum beta-lactamase (ESBL)-producing bacteria, such as Klebsiella pneumoniae, have been increasingly identified in UTI cases, particularly in antibiotic-treated populations (Achan et al., 2025) [1].
-
Increased Colonization: Antibiotic use can lead to the overgrowth of certain bacteria, including E. coli, which may increase the likelihood of reinfection or recurrent Utis. It has been shown that 50% of patients experiencing recurrent UTIs have been previously treated with antibiotics (Achan et al., 2025) [1].
-
Immunosuppression: Some antibiotics may have immunosuppressive effects, reducing the body’s ability to fight off infections. This can lead to higher rates of bacterial colonization and subsequent UTIs.
Table 1: Mechanisms Through Which Antibiotics Can Induce UTIs
| Mechanism | Description |
|---|---|
| Disruption of Normal Flora | Antibiotics eliminate beneficial bacteria, allowing pathogenic bacteria to thrive. |
| Selection for Resistant Strains | Antibiotic use promotes the survival of resistant bacterial strains. |
| Increased Colonization | Overgrowth of certain bacteria increases infection risk. |
| Immunosuppression | Reduced immune response can lead to increased susceptibility to infections. |
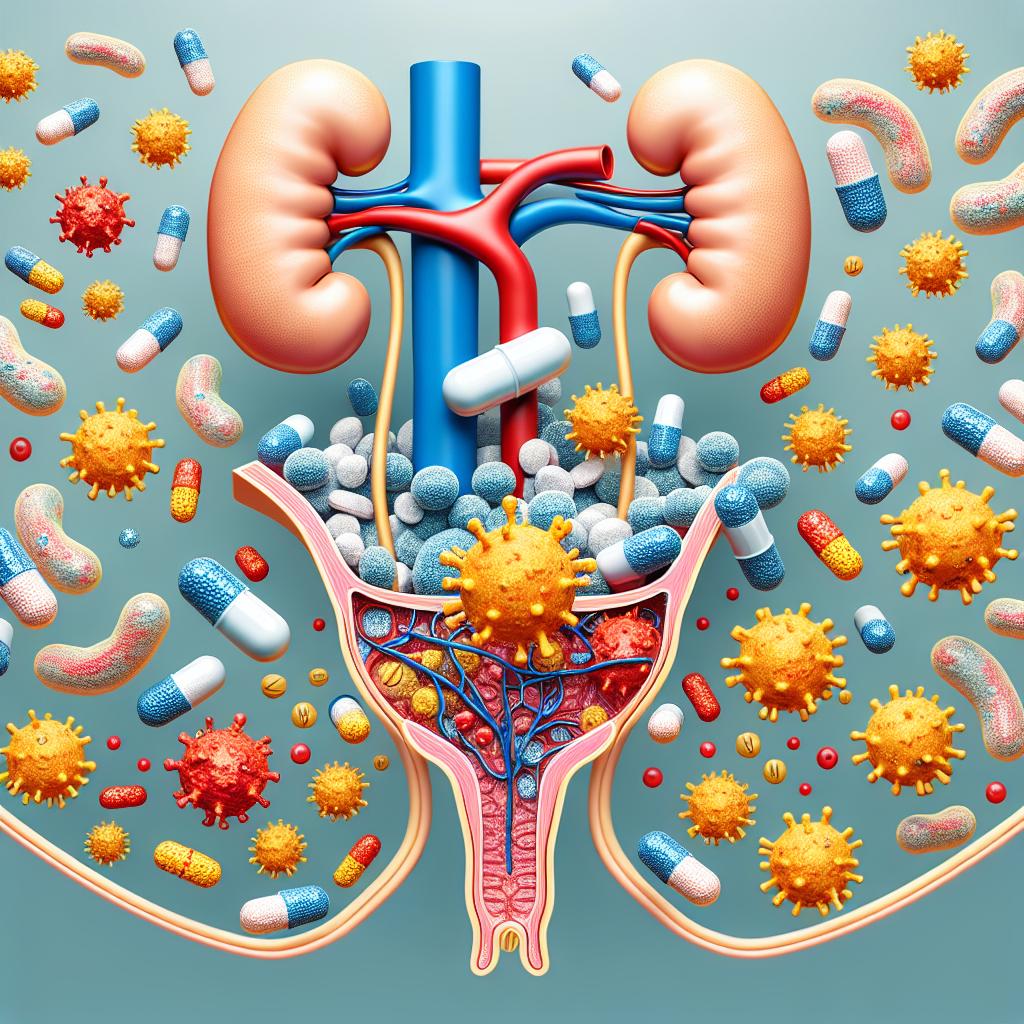
Common Antibiotics Associated with Increased UTI Risk
Several classes of antibiotics have been implicated in increasing the risk of UTIs. The following are among the most frequently noted:
- Penicillins: While generally effective against a range of bacteria, their use can disrupt the normal flora, leading to opportunistic infections.
- Cephalosporins: Similarly to penicillins, cephalosporins can lead to the dominance of resistant bacteria in the urinary tract.
- Fluoroquinolones: Although effective for treating UTIs, their overuse has been linked to the emergence of resistant strains such as E. coli.
- Trimethoprim-Sulfamethoxazole (TMP-SMX): One of the common treatments for UTIs, TMP-SMX has been associated with cases of antibiotic-induced aseptic meningitis, complicating its use in susceptible populations (Ibrahim et al., 2025) [10].
Table 2: Antibiotics Commonly Associated with Increased UTI Risk
| Antibiotic Class | Mechanism of Increased Risk |
|---|---|
| Penicillins | Disruption of normal flora; potential for opportunistic infections. |
| Cephalosporins | Similar to penicillins; selection for resistant strains. |
| Fluoroquinolones | Overuse linked to resistance; may fail to treat recurrent infections effectively. |
| TMP-SMX | Associated with adverse reactions, including drug-induced aseptic meningitis. |
Preventive Measures Against Antibiotic-Induced UTIs
To mitigate the risk of developing UTIs as a result of antibiotic use, several preventive strategies can be employed:
-
Antibiotic Stewardship: Promote responsible use of antibiotics through proper prescribing practices, ensuring they are only used when necessary.
-
Probiotics: Consider the use of probiotics to help restore normal flora during and after antibiotic treatment, thus maintaining a healthy microbiome.
-
Hydration: Encourage adequate fluid intake to help flush out bacteria from the urinary tract.
-
Education: Educate patients on the appropriate use of antibiotics and the risks associated with misuse, including the potential development of UTIs.
-
Regular Monitoring: Implement regular follow-up for patients on long-term antibiotic therapy to monitor for signs of recurrent infections.
Table 3: Preventive Measures Against Antibiotic-Induced UTIs
| Preventive Measure | Description |
|---|---|
| Antibiotic Stewardship | Responsible antibiotic prescribing and usage to minimize resistance. |
| Probiotics | Restoring normal flora to reduce the risk of infection. |
| Hydration | Increasing fluid intake to flush bacteria from the urinary tract. |
| Education | Informing patients about the risks of antibiotic misuse. |
| Regular Monitoring | Follow-up assessments for patients on long-term antibiotics to detect UTIs early. |
Conclusion: Balancing Antibiotic Use and UTI Risk
The relationship between antibiotic use and the development of urinary tract infections highlights a complex interplay that necessitates careful management. While antibiotics remain a vital component of modern medicine, their misuse can lead to adverse outcomes such as the increased incidence of UTIs. By implementing preventive measures, promoting responsible antibiotic use, and educating patients, healthcare professionals can help mitigate the risks associated with antibiotic-induced UTIs. As antimicrobial resistance continues to rise, developing effective stewardship programs and alternative treatments, such as bacteriophage therapy, may also play a crucial role in addressing this public health challenge (Ibrahim et al., 2025) [14].
References
- Achan, B., Luggya, T., Ebwongu, R. I., Sekyanzi, S., & Kajumbula, H. (2025). Tossing the coin of extended-spectrum β-lactamase: prevalence of extended-spectrum β-lactamase-producing Klebsiella pneumoniae isolated from patients with sepsis. Microbiology Society. https://doi.org/10.1099/acmi.0.000962.v3
- Ibrahim, R., Aranjani, J. M., Kalikot Valappil, V., & Nair, G. (2025). Unveiling the potential bacteriophage therapy: a systematic review. Future Science OA. https://pubmed.ncbi.nlm.nih.gov/11845108/
- Pathi, A., Adler, J. R., Patil, B. K., Mohapatra, S., Sharma, V., & Mohapatra, I. (2025). Antimicrobial sensitivity patterns of bacteria causing urinary tract infections: A retrospective study of elderly patients admitted to a tertiary care hospital in Bhubaneswar, India. Cureus. https://doi.org/10.7759/cureus.77399
- Ndaki, P. M., Mwanga, J. R., Mushi, M. F., & Konje, E. T. (2025). Drivers of inappropriate use of antibiotics among community members in low- and middle-income countries: a systematic review of qualitative studies. BMC Public Health. https://doi.org/10.1186/s12889-025-21553-6
- Muacevic, A., & Pathi, B. K. (2025). A Case of Trimethoprim‐Sulfamethoxazole Associated Aseptic Meningitis. Cureus. https://pubmed.ncbi.nlm.nih.gov/11839736/
FAQ
Can antibiotics cause urinary tract infections? While antibiotics are used to treat UTIs, their misuse can disrupt normal flora, leading to an increased risk of subsequent infections.
What are the common antibiotics associated with UTI risks? Common antibiotics include penicillins, cephalosporins, fluoroquinolones, and TMP-SMX.
What preventive measures can be taken to avoid antibiotic-induced UTIs? Preventive measures include responsible antibiotic use, hydration, education on proper medication use, and regular patient monitoring.
How can probiotics help in preventing UTIs? Probiotics can help restore the normal microbiome disrupted by antibiotics, potentially reducing the risk of UTIs.
Why is antibiotic stewardship important? Antibiotic stewardship is crucial in preventing the development of antibiotic resistance and ensuring effective treatment for infections.