Table of Contents
Does Amoxicillin Work for UTI Treatment?
Amoxicillin is a penicillin-type antibiotic commonly used to treat bacterial infections, including UTIs. While it has been historically prescribed for uncomplicated cases, its effectiveness is now under scrutiny due to rising resistance patterns among uropathogenic E. coli strains. Studies show that resistance to amoxicillin is prevalent, with some regions reporting up to 69.3% resistance rates in uropathogenic E. coli (Alameer et al., 2024).
Table 1: Antibiotic Resistance Patterns in Uropathogenic E. coli
| Antibiotic | Resistance Rate (%) |
|---|---|
| Amoxicillin | 69.3 |
| Trimethoprim | 27.0 |
| Nitrofurantoin | 14.5 |
| Fosfomycin | 3.1 |
| Meropenem | 21.1 |
| Ceftazidime | 43.6 |
Amoxicillin’s historical use stems from its broad-spectrum activity against common pathogens. However, its efficacy is significantly compromised in the face of AMR. This reality necessitates careful consideration of local resistance patterns when selecting empirical therapy for UTIs.
Amoxicillin: An Overview of Its Use in UTIs
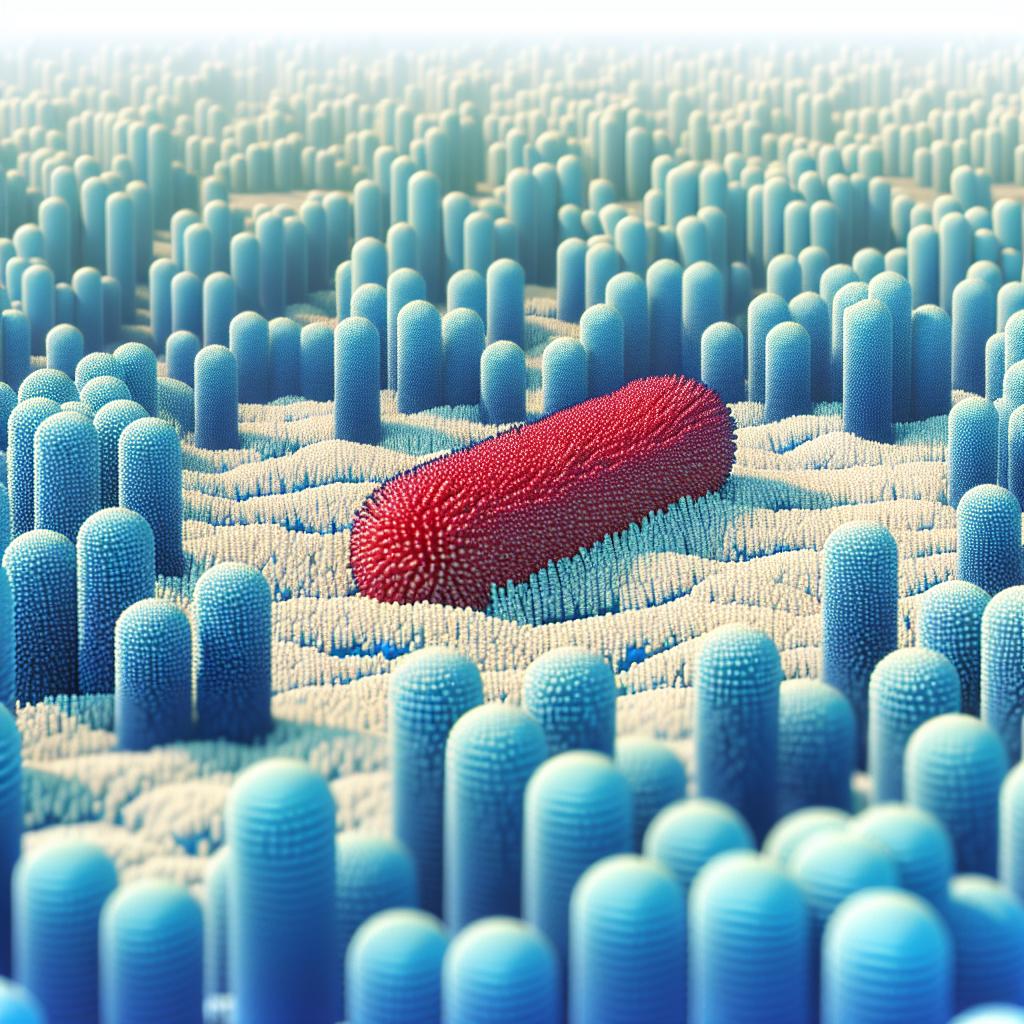
Amoxicillin is effective against a range of gram-positive and some gram-negative bacteria. Its mechanism involves inhibiting bacterial cell wall synthesis, leading to cell lysis. However, the emergence of beta-lactamase producing bacteria, particularly extended-spectrum beta-lactamase (ESBL) producing E. coli, poses a significant challenge to its use.
In uncomplicated cystitis, amoxicillin was once a first-line treatment; however, recent studies indicate a marked decline in its effectiveness. For instance, in a study conducted in Saudi Arabia, 31% of E. coli isolates were found to be ESBL producers, substantially reducing the efficacy of amoxicillin and other beta-lactam antibiotics (Alhazmi et al., 2024).
Resistance Patterns of Uropathogenic E. coli and Amoxicillin
The resistance landscape for uropathogenic E. coli is continuously evolving. Factors contributing to this rise include the overuse of antibiotics, improper prescribing practices, and the use of broad-spectrum antibiotics in non-specific infections. For example, a study conducted in the East of England reported high resistance rates of 27% for trimethoprim and 8.3% for cefalexin among the E. coli isolates tested (Drazich-Taylor et al., 2024).
Recommended Antibiotics for Uncomplicated Cystitis
Given the increasing resistance to amoxicillin, alternative antibiotics are often recommended for treating uncomplicated cystitis. First-line treatments now typically include:
- Nitrofurantoin - often preferred due to its effectiveness and lower resistance rates.
- Trimethoprim - still effective in many cases, but resistance is rising.
- Fosfomycin - a promising option with low resistance rates, particularly effective for single-dose therapy.
- Pivmecillinam - another alternative, particularly for women with recurrent infections.
Table 2: Recommended Antibiotics for Uncomplicated Cystitis
| Antibiotic | Common Use | Resistance Rate (%) |
|---|---|---|
| Nitrofurantoin | First-line | 14.5 |
| Trimethoprim | First-line | 27.0 |
| Fosfomycin | Single-dose | 3.1 |
| Pivmecillinam | Alternative | 21.0 |
Factors Influencing the Effectiveness of Amoxicillin in UTIs
Several factors influence the effectiveness of amoxicillin in treating UTIs, including:
- Antibiotic Resistance: The rise of ESBL-producing E. coli has rendered amoxicillin less effective, necessitating susceptibility testing before selection.
- Patient Factors: Age, sex, comorbidities, and prior antibiotic use can influence infection outcomes and resistance patterns.
- Geographical Variation: Resistance rates can vary significantly based on regional prescribing practices and local epidemiology, underscoring the importance of tailored treatment approaches (Alameer et al., 2024; Drazich-Taylor et al., 2024).
Table 3: Factors Affecting UTI Treatment Outcomes
| Factor | Impact on Efficacy |
|---|---|
| Antibiotic Resistance | Decreased effectiveness of amoxicillin |
| Patient Comorbidities | Higher risk of recurrent infections |
| Regional Resistance Patterns | Variable efficacy of empirical therapy |
Conclusion
In conclusion, while amoxicillin has been a staple in the treatment of uncomplicated Utis, its effectiveness is increasingly compromised by rising rates of resistance, particularly among uropathogenic E. coli. The emergence of ESBLs and other resistant strains necessitates a shift towards more effective alternatives, such as nitrofurantoin and fosfomycin, supported by rigorous antibiotic stewardship practices.
Frequently Asked Questions (FAQ)
Is amoxicillin still effective for all UTIs?
No, amoxicillin is not effective for all UTIs due to rising resistance rates, particularly among E. coli strains.
What are the first-line treatments for uncomplicated cystitis now?
First-line treatments typically include nitrofurantoin, trimethoprim, and fosfomycin, depending on local resistance patterns.
How can I prevent recurrent UTIs?
Preventive measures include staying hydrated, urinating after intercourse, and practicing good hygiene.
What should I do if I have recurrent UTIs?
Consult your healthcare provider for a tailored treatment plan, which may include testing for underlying conditions and potential use of prophylactic antibiotics.
How does antibiotic resistance develop?
Antibiotic resistance develops through overuse and misuse of antibiotics, allowing bacteria to adapt and survive treatments that would normally be effective.
References
-
Alameer, K. M., Abuageelah, B. M., Alharbi, R. H., Alfaifi, M. H., Hurissi, E., Haddad, M., Dhayhi, N., Jafar, A. S., Mobarki, M., Awashi, H., & Musawi, S. (2024). Retrospective Analysis of Antibiotic Resistance Patterns of Uropathogenic Escherichia coli With Focus on Extended‐Spectrum β‐Lactamase at a Tertiary Central Hospital in Saudi Arabia. Health Sci Rep
-
Drazich-Taylor, S., Moore, J., & Craine, A. (2024). Resistance to empirical antibiotics in urinary tract infections caused by Enterobacterales in the East of England. JAC Antimicrob Resist
-
Alhazmi, A. H., Alameer, K. M., Abuageelah, B. M., Alharbi, R. H., & Mobarki, M. (2023). Emergence of Extended spectrum β-lactamase (ESBL) and carbapenemase producing Escherichia coli (E. coli) in mid-stream urine cultures of patients presenting in outpatient department of tertiary care hospital with uncomplicated cystitis (2016-2022): A retrospective analysis of Laboratory data. PJMS. https://doi.org/10.12669/pjms.41.1.3379